© Borgis - New Medicine 4/2009, s. 79-81
*Magdalena Fršckiewicz, Lechosław P. Chmielik, Mieczysław Chmielik
BACTERIOLOGICAL AETIOLOGY OF CHRONIC RHINOSINUSITIS IN CHILDREN DURING 2007–2009
Department of Paediatric Otorhinolaryngology, Medical University of Warsaw, Poland
Head of Department: Prof. Mieczysław Chmielik, MD, PhD
Summary
Introduction:Chronic rhinosinusitis (CRS) is an inflammatory process affecting the mucosa of the nasal cavities and paranasal sinuses. The inflammation lasts more than 4-6 weeks. The aetiology of CRS is multifactorial. A number of conditions predispose to rhinosinusitis, among others microbial infection.
Aim: To evaluate the bacteriological testing of samples taken from the middle nasal turbinates and lumen of maxillary sinuses of children operated on for chronic rhinosinusitis.
Material and method: The research included 139 children, treated surgically in the Department of Paediatric Otolaryngology, Warsaw Medical University between 2007 and 2009. The material for bacteriological examination was collected during endoscopic sinus surgery from the middle nasal turbinates and maxillary sinuses.
Results: Two diagrams presented below show the most frequent pathogens co-existing with chronic rhinosinusitis in the examined group. Both in the material from the maxillary sinuses and from the middle nasal turbinates Staphylococcus spp. coagulase(-) was cultured most frequently.
Discussion: Chronic rhinosinusitis develops as a result of a composite and multistage inflammatory process. At least one component of the pathogenesis of CRS is bacterial infection. In our research in fairly many cases we have noticed a lack of correlation between the results from the nasal turbinates and from the maxillary sinuses.
Conclusions: 1. The results of bacteriological testing in the examined group differ from the most common aetiology that causes rhinosinusitis described in the literature. 2. The results taken from the middle nasal turbinate in most cases differ from the results taken from the lumen of the maxillary sinuses. 3. Examination of samples taken from the middle nasal turbinates and maxillary sinuses play a vital role in establishing the aetiology of rhinosinusitis and in choosing the exact treatment in case of recurrence of rhinosinusitis.
INTRODUCTION
Chronic rhinosinusitis (CRS) is a common clinical condition. It is caused by a chronic inflammatory process affecting the mucosa of the nasal cavities and paranasal sinuses that lasts constantly for more than 4-6 weeks, and which cannot be cured by pharmacological treatment [1,3,5].
According to Meltzer the symptoms of CRS can be divided into two groups, as major and minor symptoms [4,5]:
Major symptoms include:
– muco-purulent discharge present in the anterior rhinoscopy and/or in posterior nostrils and posterior wall of the pharynx,
– impaired patency of the nose,
– dull headaches.
And minor symptoms include:
– headaches of different character,
– bursting otalgia,
– cough,
– sub-febrile body temperature,
– fatigue,
– fetor ex ore,
– toothaches.
Chronic rhinosinusitis is manifested by the presence of at least 2 major symptoms, or 1 major and at least 2 minor symptoms for more than 4-6 weeks.
The aetiology of chronic rhinosinusitis is multifactorial. Repeated acute upper respiratory tract infections can lead to mucosal swelling, obstruction of sinus outflow, and, eventually, chronic infection. A number of conditions predispose to rhinosinusitis, including allergies, decongestant spray abuse (rhinosinusitis medicamentosa), immunoglobulin deficiencies, disorders of mucociliary transport, and changes in glandular secretions. In addition, anatomical factors such as septal deviations, hypertrophic middle turbinates, and concha bullosa can affect the nasal cavity and sinus ostia airflow. Gradually processes occurring in the mucosa lead to impatency of natural openings of the sinuses and disturbance of their ventilation. This causes the retention of infected secretions in the lumen of sinuses [1, 2, 3].
AIM
To evaluate the bacteriological testing of samples taken from the middle nasal turbinates and lumen of the maxillary sinuses of children operated on for chronic rhinosinusitis.
MATERIAL AND METHOD
The research included 139 patients with chronic rhinosinusitis (69 females, 70 males), aged 5 to 17, treated surgically in the Department of Paediatric Otolaryngology, of Warsaw Medical University in the period between January 2007 and March 2009. In all cases endoscopic sinus surgery was performed. The material for bacteriological examination was collected during the surgical procedure from both the middle nasal turbinates and from the maxillary sinuses. Inoculation of bacteria was cultured into a medium produced by Biomerieux company. In all cases in which the result of the microbiological examination was positive, antibiograms were made. Results with the antibiogram were attached to the patient´s records in the out-patient clinic in case of aggravation of symptoms of CRS.
RESULTS
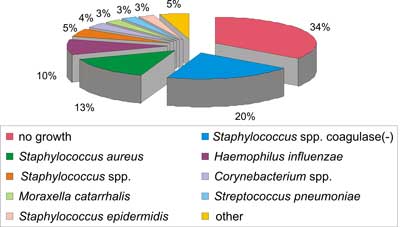
The most common pathogens cultured from samples from the middle nasal turbinates included: Staphylococcus spp. coagulase(-), Staphylococcus aureus, Haemophilus influenzae, Staphylococcus spp., Corynebacterium spp., Moraxella catarrhalis, Streptococcus pneumoniae, and Staphylococcus epidermidis. The group "other pathogens” included (each pathogen in 0.6%): Klebsiella oxytoca, Streptococcus viridans, Streptococcus spp. α-hemolizing, Staphylococcus haemolyticus MS, Alcaligenes spp., Pseudomonas aeruginosa, and Streptococcus spp.
Fig. 1. Bacteriological testing from middle nose turbinates.
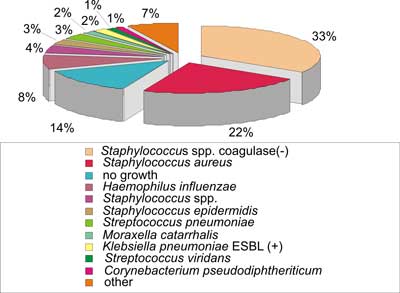
The most common pathogens cultured from samples from the maxillary sinuses were: Staphylococcus spp. coagulase(-), Staphylococcus aureus, Haemophilus influenzae, Staphylococcus spp., Staphylococcus epidermidis, Streptococcus pneumoniae, Moraxella catarrhalis, Klebsiella pneumoniae ESBL (+), Streptococcus viridans, and Corynebacterium pseudodiphteriticum. The group "other pathogens” included (each pathogen in 0.6%): Moraxella osloensis, Acinetobacter lwoffii, Escherichia coli, Pseudomonas aeruginosa, Corynebacterium spp., Staphylococcus simulans, Bacillus spp., Actinomyces naeslundii, Peptostreptococcus spp., and Prevotella spp.
Fig. 2. Bacteriological testing from maxillary sinuses.
Barely in 40.3% of cases we noticed a correlation between results from the nasal turbinates and from the maxillary sinuses. In this group in 18% of cases there was no growth of any pathogens.
DISCUSSION
Chronic rhinosinusitis develops as a result of a composite and multistage inflammatory process. This state most frequently can be caused by chronic and reoccurring bacterial infections. The consequence of this is a disturbance of normal functioning of the nasal mucosa [2, 3, 10, 11].
Most investigators agree that at least one component of the pathogenesis of CRS is microbial infection. Because of the important role of bacterial infection in CRS, most treatment guidelines recommend antibiotics in the medical management of CRS before consideration of surgical therapy. In addition, despite adequate surgical therapy, typically with endoscopic sinus surgery (ESS), a small but significant number of patients may continue to experience acute bacterial exacerbations of their CRS, often requiring antibiotic therapy. In our research the material was taken during endoscopic sinus surgery from the middle nasal turbinates and maxillary sinuses. The three most frequently occurring pathogens were: Staphylococcus spp. coagulase(-), Staphylococcus aureus MS, and Haemophilus influenzae. They are not the same pathogens that are responsible for causing acute rhinosinusitis most frequently (these are: Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis). This difference is probably caused by the use of antibiotics in aggravation of the chronic process. If antibiotic therapy is needed amoxicillin, macrolides and folate inhibitors (trimethoprim/sulfamethoxazole) are reasonable initial selections. Antibiotic selection should be guided by local epidemiological patterns of infection and antibiotic sensitivity. Recently we can observe overuse of antibiotics especially in the practice of family doctors [6,7,8,9]. In our research in some cases we discovered a lack of correlation between the results of inoculation from the middle turbinates and from the maxillary sinuses.
CONCLUSIONS
1. Results of bacteriological testing in the examined group differ from the most common aetiology that causes rhinosinusitis described in the literature.
2. Results taken from the middle nasal turbinate in most cases differ from the results taken from the lumen of the maxillary sinuses.
3. Examination of samples taken from the middle nasal turbinates and maxillary sinuses play a vital role in establishing the aetiology of rhinosinusitis and in choosing the exact treatment in case of recurrence of rhinosinusitis.
Piśmiennictwo
1. „Otolaryngologia Dziecięca” pod redakcjš Danuty Gryczyńskiej, 2007. 2. Hadley J. Sharp, David Denman, Susan Puumala, Donald A. Leopold. Treatment of acute and chronic rhinosinusitis in the United States, 1999-2002. Arch Otolaryngol Head Neck Surg/Vol 133, Mar 2007 s. 260-265. 3. Otorynolaryngologia praktyczna pod redakcjš Grzegorza Janczewskiego, 2005. 4. Meltzer and col. Rhinosinusitis: establishing definitions for clinical research and patient care Journal of Allergy And Clinical Immunology, 2004 Dec. 114(6). 5. Bluestone, Stool, Alper, Arjmand, Casselbrant, Dohar, Yellon "Pediatric Otolaryngology”. 6. Valerie J. Lund. Therapeutic targets in rhinosinusitis: Infection or inflammation? Medscape J Med. 2008; 10(4): 105. 7. Dzierżanowska-Fangrat Katarzyna, Dzierżanowska Danuta Zakażenia w otolaryngologii - etiopatogeneza i terapia. Stand. Med. 2006: 3 (1) s.12-16. 8. Neil Bhattacharyya, Lynn J. Kepnes. The risk of development of antimicrobial resistance in individual patients with chronic rhinosinusitis Arch Otolaryngol Head Neck Surg. 2004;130:1201-1204. 9. Daniel A. Power, Jeremy P. Burton, Chris N. Chilcott, John R. Tagg, Patrick J. Dawes. Non-culture-based analysis of bacterial populations from patients with chronic rhinosinusitis J. Clin. Microbiol. Nov. 2005, Vol. 43, No. 11, p. 5822–5824. 10. Vaidya, Abhay M.; Chow, James M.; Stankiewicz, James A.; Young, M. Rita I.; Mathews, Herbert L. Correlation of Middle Meatal and Maxillary Sinus Cultures in Acute Maxillary Sinusitis American Journal of Rhinology Vol 11, Number 2, March-April 1997, pp. 139-143(5). 11. Axelsson, A M.D.; Brorson, J E M.D. The correlation between bacteriological findings in the nose and maxillary sinus in acute maxillary sinusitis. Laryngoscope. 83(12):2003-2011, December 1973.