© Borgis - Postępy Nauk Medycznych 4/2016, s. 238-240
*Magdalena Naorniakowska, Elwira Kołodziejczyk, Karolina Piwczyńska, Grzegorz Oracz
Autoimmune pancreatitis in a 13.5-year-old child – a case report
Autoimmunologiczne zapalenie trzustki u 13,5-letniego dziecka – opis przypadku
Department of Gastroenterology, Hepatology, Feeding Disorders and Pediatrics, The Children’s Memorial Health Institute, Warsaw
Head of Department: prof. Józef Ryżko, MD, PhD
Streszczenie
Autoimmunologiczne zapalenie trzustki (AIP) jest rzadko rozpoznawaną jednostką chorobową, która może sprawiać trudności diagnostyczne. Dotychczas w literaturze opisano jedynie kilka przypadków pacjentów pediatrycznych. Jest to forma przewlekłego zapalenia trzustki (PZT), w której często pierwszą manifestacją jest guz w jamie brzusznej, który może być mylnie rozpoznany jako rak trzustki. Zmiany nowotworowe trzustki zazwyczaj są leczone operacyjnie, podczas gdy leczenie autoimmunologicznego zapalenia trzustki opiera się głównie na terapii farmakologicznej. Dlatego też różnicowanie tych dwóch jednostek chorobowych jest niezwykle istotne. Objawy autoimmunologicznego zapalenia trzustki mogą być zróżnicowane, jakkolwiek u niektórych pacjentów nie obserwujemy żadnych dolegliwości. AIP należy podejrzewać wtedy, gdy klinicznym i radiologicznym objawom guza towarzyszą odchylenia w badaniach laboratoryjnych, takie jak podwyższony poziom autoprzeciwciał oraz frakcji G4 immunoglobuliny G. Natomiast gdy badania serologiczne nie są wystarczające do postawienia rozpoznania, wykonanie biopsji guza może uchronić pacjenta od niepotrzebnego zabiegu operacyjnego.
W artykule przedstawiono przypadek 13,5-letniego chłopca z guzem głowy trzustki oraz zdwojeniem przewodu trzustkowego, u którego ostatecznie rozpoznano autoimmunologiczne zapalenie trzustki.
Summary
Autoimmune pancreatitis (AIP) is a rare, newly recognized disease and there are only few reports of pediatric patients. It is a form of chronic pancreatitis that frequently presents as a mass which can be mistakenly diagnosed as a pancreatic cancer. Pancreatic neoplasms are generally treated by resection, while the management of autoimmune pancreatitis is mostly pharmacological, so it is very important to distinguish one from another. The presenting symptoms in AIP are variable although asymptomatic patients can occur as well. Autoimmune pancreatitis should be suspected when characteristic clinical signs and radiographic images are associated with a higher level of autoimmune antibodies and IgG4, but when serologic tests are not diagnostic, a biopsy may spare a child a pancreatic resection.
We report the case of a 13.5-year-old child who presented with a 4 cm mass in the head of the pancreas with a double duct sign who was finally diagnosed with autoimmune pancreatitis.

Introduction
Autoimmune pancreatitis (AIP) is a rare, usually an adult-onset inflammatory autoimmune disease, a form of chronic pancreatitis, extremely uncommon in children. AIP is usually associated with a mass in the pancreas, thus mimicking pancreatic neoplasia. Failure to consider this condition could lead to unnecessary medical procedures or pancreatic resection, whereas it often completely resolves with steroid treatment (1-3).
The first observations of pancreatitis to suggest the concept of AIP were reported about 50 years ago by Sarles et al. (4), however the term autoimmune pancreatitis was originally introduced by Yoshida et al. (5) in 1995. In 2002, the Japan Pancreas Society published the diagnostic criteria of AIP based on a combination of the findings of imaging, laboratory testing, and histological analysis (6). AIP likely accounts for a significant proportion of cases previously classified as idiopathic pancreatitis (7). In 2011, the International Association of Pancreatology proposed International Consensus Diagnostic Criteria (ICDC), which composed of five cardinal features such as imaging, serology, other organ involvement, histology, and response to steroid therapy, categorized as type 1 or 2 AIP findings depending on the diagnostic reliability (8).
The presenting symptoms are variable and most commonly include painless jaundice, weight loss and abdominal pain. Patients rarely present with acute attacks of pain, more typical of acute pancreatitis, some of patient with AIP have diabetes mellitus (7). Although asymptomatic patients can occur as well.
Case report
13.5-year-old previously healthy girl was admitted to Department of Gastroenterology, Hepatology, Feeding Disorders and Pediatrics, The Children’s Memorial Health Institute with suspicion of pancreatic tumor.
The mass was accidentally found while the physical examination on periodic health evaluation. An abdominal ultrasound (US scan) examination and computer tomography (CT) were performed and revealed enlarged head of pancreas with the mass measuring 40 x 33 x 38 mm. Laboratory tests were within normal limits. Immunoglobulin levels including IgG 4 subclass were normal as well as CEA and CA19-9 levels.
The patient was transferred to our hospital for further investigation. On physical examination no abnormalities except for the mass in the left upper quadrant of abdomen were found. Laboratory tests revealed slightly elevated serum amylase (102 U/l) and lipase (210 U/l) activity. US scan similarly to previous examinations showed 33 x 22 mm heterogeneous solid mass in the enlarged pancreatic head and mild dilation of the pancreatic duct (2.5 mm).
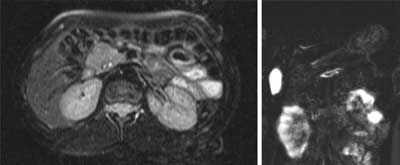
In order to better visualization of the change – magnetic resonance imaging (MRI) of the abdomen was performed. It showed difficult to distinguishable change of size 30 x 25 mm. The pancreatic duct was widened (as in the US scan) and in the distal part of the pancreas doubled (pancreas divisum was suspect) (fig. 1).
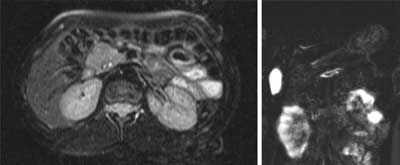
Fig. 1. MRI image. Focal mass in the head of the pancreas. Widened pancreatic duct, doubled in the distal part. Material of the Department of Diagnostic Imaging, The Children’s Memorial Health Institute, Warsaw, Poland
Powyżej zamieściliśmy fragment artykułu, do którego możesz uzyskać pełny dostęp.
Mam kod dostępu
- Aby uzyskać płatny dostęp do pełnej treści powyższego artykułu albo wszystkich artykułów (w zależności od wybranej opcji), należy wprowadzić kod.
- Wprowadzając kod, akceptują Państwo treść Regulaminu oraz potwierdzają zapoznanie się z nim.
- Aby kupić kod proszę skorzystać z jednej z poniższych opcji.
Opcja #1
24 zł
Wybieram
- dostęp do tego artykułu
- dostęp na 7 dni
uzyskany kod musi być wprowadzony na stronie artykułu, do którego został wykupiony
Opcja #2
59 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 30 dni
- najpopularniejsza opcja
Opcja #3
119 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 90 dni
- oszczędzasz 28 zł
Piśmiennictwo
1. Finkelberg DL, Sahani D, Deshpande V, Brugge WR: Autoimmune pancreatitis. N Engl J Med 2006; 355(25): 2670-2676.
2. Ghazale A, Chari ST: Optimising corticosteroid treatment for autoimmune pancreatitis. Gut 2007; 56(12): 1650-1652.
3. Kamisawa T, Shimosegawa T, Okazaki K et al.: Standard steroid treatment for autoimmune pancreatitis. Gut 2009; 58(11): 1504-1507.
4. Sarles H, Sarles JC, Muratore R et al.: Chronic inflammatory sclerosis of the pancreas: an autoimmune pancreatic disease? Am J Dig Dis 1961; 6: 688-698.
5. Yoshida K, Toki F, Takeuchi T et al.: Chronic pancreatitis caused by an autoimmune abnormality. Proposal of the concept of autoimmune pancreatitis. Dig Dis Sci 1995; 40(7): 1561-1568.
6. Members of the Criteria Committee for Autoimmune Pancreatitis of the Japan Pancreas Society. Diagnostic criteria for autoimmune pancreatitis by the Japan Pancreas Society. J Jpn Pan Soc 2002; 17: 585-587.
7. Zandieh I, Byrne MF: Autoimmune pancreatitis: a review. World J Gastroenterol 2007; 13: 6327-6332.
8. Shimosegawa T, Chari ST, Frulloni L et al.: International consensus diagnostic criteria for autoimmune pancreatitis: guidelines of the International Association of Pancreatology. Pancreas 2011; 40(3): 352-358.
9. Blejter J, Weller S, Pace R et al.: Autoimmune pancreatitis: an adolescent case and review of the literature. J Pediatr Surg 2008; 43: 1368-1372.
10. Gargouri L, Ponsot P, Viala J et al.: Recurrent autoimmune pancreatitis in a 10-year-old boy. J Pediatr Gastroenterol Nutr 2009; 48: 374-377.
11. Refaat R, Harth M, Proschek P et al.: Autoimmune pancreatitis in an 11-year-old boy. Pediatr Radiol 2009; 39: 389-392.
12. Takase M, Imai T, Nozaki F: Relapsing autoimmune pancreatitis in a 14 year old girl. J Nippon Med Sch 2010; 77: 29-34.
13. Friedlander J, Quiros J, Morgan T et al.: Diagnosis of autoimmune pancreatitis vs neoplasms in children with pancreatic mass and biliary obstruction. Clin Gastroenterol Hepatol 2012; 10: 1051-1055.
14. Long J, Birken G, Migicovsky B: Autoimmune pancreatitis in a child presenting as a pancreatic mass. J Pediatr Surg 2015; 3: 111-113.
15. Bartholomew S, Zigman A, Sheppard B: Lymphoplasmacytic sclerosing pancreatitis presenting as a pancreatic head mass in a child: case report and management recommendations. J Pediatr Surg 2006; 41: e23-e25.
16. Zen Y, Grammatikopoulos T, Hadzic N: Autoimmune pancreatitis in children: insights into the diagnostic challenge. J Pediatr Gastroenterol Nutr 2013 May 2.
17. Oracz G, Cukrowska B, Kierkus J, Ryzko J: Autoimmune markers in children with chronic pancreatitis. Prz Gastroenterol 2014; 9: 142-146.
18. El-Matary W, Casson D, Hodges S et al.: Successful conservative management of idiopathic fibrosing pancreatitis in children. Eur J Pediatr 2006; 165: 560-565.