*Tomasz Derkowski1, Sylweriusz Kosinski2, Tomasz Sanak3, Paweł Podsiadlo1, 4, Daniel Celinski1, 5, Robert Galazkowski1, 5, Tomasz Darocha1, 6
Post-traumatic hypothermia in the pre-hospital period – diagnosis and treatment
Hipotermia pourazowa w okresie przedszpitalnym – rozpoznanie i leczenie
1Polish Air Medical Rescue, Warsaw, Poland
2Department of Emergency Medical Services, Collegium Medicum Jagiellonian University, Cracow, Poland
3Department of Disaster and Emergency Medicine, Collegium Medicum Jagiellonian University, Cracow, Poland
4Polish Society for Mountain Medicine and Rescue, Szczyrk, Poland
5Department of Emergency Medical Services, Medical University of Warsaw, Poland
6Department of Anaesthesiology and Intensive Therapy, Medical University of Silesia, Katowice, Poland
Streszczenie
Konsekwencje hipotermii w okresie pourazowym są znane od ponad czterech dekad, ale świadomość problemu jest nadal niska. Hipotermia pourazowa jest czynnikiem ryzyka groźnych powikłań i zgonu u chorych z ciężkimi obrażeniami ciała. Postępowanie medyczne w okresie przedszpitalnym powinno być ukierunkowane na jak najszybsze przerwanie ekspozycji na niekorzystne warunki środowiska, zahamowanie utraty ciepła poprzez adekwatną izolację termiczną, tamowanie krwotoków, unikanie masywnych przetoczeń płynów i jak najszybszy transport do szpitala w odpowiednio przygotowanym środku transportu. Niezwykle istotne są świadomość problemu, prewencja i odpowiednia koordynacja działań na każdym etapie leczenia.
Summary
Implications of post-traumatic hypothermia are known for over four decades however general awareness of such occurrence is still low.
Post-traumatic hypothermia is a risk factor for severe complications and death of patients with serious injuries. Medical treatment in perioperative period should be directed towards the prompt cessation of patient exposure to adverse weather conditions, inhibition of heat loss by appropriate thermal insulation, haemorrhage control, avoidance of excessive administration of fluids and quick transfer to a hospital in appropriately prepared means of transport.
Hypothermia awareness, preventative tasks and coordination of action at each stage of the rescue is crucial.

Introduction
In accordance with the ATLS committee, post-traumatic hypothermia can be diagnosed at the central temperature below 36°C (1). Further stages and post-traumatic hypothermia classification is shown in the table 1 (2, 3). Certain scientific literature acknowledges hypothermia at 35°C, however in Poland the ATLS definition is considered correct due to the impact of post-traumatic period as well as prevention role in hypothermia.
Tab. 1. Post-traumatic hypothermia classification
| Classification | Temperature range |
| Mild | 36-34°C |
| Moderate | 34-32°C |
| Severe | < 32°C |
The “post-traumatic hypothermia” term have been introduced in the 80’s of 20th century (3-5). Commonly, and alongside with acidosis and coagulopathy, have been known as “deadly triad”. However, nowadays, hypothermia is being recognized as a standalone factor in severe injury complications. Indeed, the knowledge around this matter is confined among certain medical personnel groups only (6).
Review
Pathophysiology
Both hypothermia types – due to cold exposure (also known as accidental) as well as post-traumatic – results from negative thermal balance, i.e. higher heat loss than its production. Ways of heat loss and its meaning in post-traumatic hypothermia have been described in table 2.
Tab. 2. Major means of heat loss in human body
| Means of heat loss | Description and meaning |
| Conduction | Heat transfer via direct contact, such as body adherence to lower temperature surface – concrete (fig. 1), ground, spinal board. Major heat loss is caused by body immersion in water. Wet clothes speed up the heat loss. |
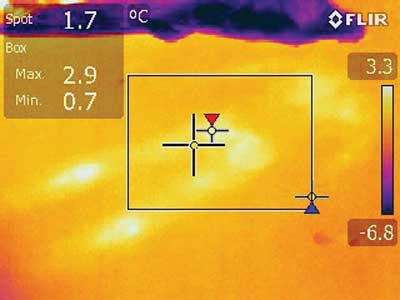
Fig. 1. Thermal trace of the human in thermography (so called “symptom of the Turin Shroud”). The picture of the concrete where the injured patient has been laid. It shows the role of conduction in heat loss of the organism. Own archive by Tomasz Sanak
| Convection | Heat transfer from the body surface to the surrounding air. Convectional heat loss is further escalated by the air movement, such as wind, draught or open window in the ambulance. |
| Radiation | Energy transfer in form of radiation within the infrared band. The energy is being emitted by warmer objects and absorbed by colder ones. The lower surface temperature, the lower amount of heat is being transferred. Usually the radiation is one of ways of the heat loss, however in case of insulation or radiators, radiation can allow to create the heat gain. |
| Vaporization | Loss of the heat that allows needed for vaporization of the moisture from the skin surface. In hypothermia such process takes place under sealed, moisture-proof clothes and covers. |
| Breathing | Approximately 10% of the whole heat loss takes place via airways (convection and moisture vaporization from mucous membrane). |
Epidemiology: causes and risk factors
Among patients with body injuries as admitted to ER’s, the hypothermia occurs from 1.5% to over 60% (7-11). Such huge discrepancy comes from both, various criteria as used while diagnosis as well as scientific research methodology. The main issue seems to be not so much the set temperature threshold, but the frequency and the means of its measurement. It turns out that the core temperature (Ct) measurement, even though it should be the case, in fact it is not the routine task with patients suffering from serious injury. In German register of multi-organ injuries (DGU) the Ct measurement has been documented at less than 40% of patients (12). It turns out that the most serious risk factor for post-traumatic hypothermia is the nature and severity of the injury along with the existing shock (9, 13-16). Metabolic transition is being carried out much slower due to the limited flow of the blood within tissues. This results in limited production of the heat. The tissue hypoxia is also a natural inhibitor of muscular shiver that, in normal circumstances, provides very effective way for thermogenesis. Should you add intensified loss of the heat to the impaired heat production, it will result in a very rapid loss of the core temperature. Table 3 summarizes post--traumatic hypothermia risk factors.
Tab. 3. Post-traumatic hypothermia risk factors (according to 9, 13-19)
• Nature and severity of the injury (penetrating trauma, Injury Severity Score > 15)
• Volume and temperature of the intravenous fluid administration
• Temperature inside the transporting unit
• Age > 65 years
• Neurological impairment (GCS < 8)
• Immobilisation (i.e. inside a vehicle)
• Head injury
• Alcohol intoxication
• Extended time between the sustained injury and the arrival at the hospital
• Endotracheal intubation
• Cold time of the year |
Powyżej zamieściliśmy fragment artykułu, do którego możesz uzyskać pełny dostęp.
Mam kod dostępu
- Aby uzyskać płatny dostęp do pełnej treści powyższego artykułu albo wszystkich artykułów (w zależności od wybranej opcji), należy wprowadzić kod.
- Wprowadzając kod, akceptują Państwo treść Regulaminu oraz potwierdzają zapoznanie się z nim.
- Aby kupić kod proszę skorzystać z jednej z poniższych opcji.
Opcja #1
24 zł
Wybieram
- dostęp do tego artykułu
- dostęp na 7 dni
uzyskany kod musi być wprowadzony na stronie artykułu, do którego został wykupiony
Opcja #2
59 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 30 dni
- najpopularniejsza opcja
Opcja #3
119 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 90 dni
- oszczędzasz 28 zł
Piśmiennictwo
1. American College of Surgeons: Advanced Trauma Life Support. 7th ed. American College of Surgeons, Chicago 2004: 240-241.
2. Kortbeek JB, Al Turki SA, Ali J et al.: Advanced trauma life support, the evidence for change. J Trauma 2008; 64(6): 1638-1650.
3. Jurkovich GJ, Greiser WB, Luterman A et al.: Hypothermia in trauma victims: an ominous predictor of survival. J Trauma 1987; 27(9): 1019-1024.
4. Yates DW, Little RA: Accidental hypothermia. Resuscitation 1979; 7(1): 59-67.
5. Luna GK, Maier RV, Pavlin EG et al.: Incidence and effect of hypothermia in seriously injured. J Trauma 1987; 27(9): 1014-1018.
6. Podsiadło P: Praca doktorska „Ocena skuteczności platformy e-learningowej jako formy edukacji personelu systemu ratownictwa medycznego w zakresie hipotermii”. Lublin 2017.
7. Perlman R, Callum J, Laflamme C et al.: A recommended early goal-directed management guideline for the prevention of hypothermia-related transfusion, morbidity, and mortality in severely injured trauma patients. Crit Care 2016; 20(1): 107.
8. Rutherford EJ, Fusco MA, Nunn CR et al.: Hypothermia in critically ill trauma patients. Injury 1998; 29(8): 605-608.
9. Martin RS, Kilgo PD, Miller PR et al.: Injury-associated hypothermia: an analysis of the 2004 national trauma databank. Shock 2005; 24(2): 114-118.
10. Shafi S, Elliott AC, Gentilello L: Is hypothermia simply a marker of shock and injury severity or an independent risk factor for mortality in trauma patients? Analysis of a large national trauma registry. J Trauma 2005; 59(5): 1081-1085.
11. Wang HE, Callaway CW, Peitzman AB et al.: Admission hypothermia and outcome after major trauma. Crit Care Med 2005; 33(6): 1296-1301.
12. Weuster M, Brück A, Lippross S et al.: Epidemiology of accidental hypothermia in polytrauma patients: An analysis of 15,230 patients of the TraumaRegister DGU. J Trauma Acute Care Surg 2016; 81(5): 905-912.
13. Arthurs Z, Cuadrado D, Beekley A et al.: The impact of hypothermia on trauma care at the 31st combat support hospital. Am J Surg 2006; 191(5): 610-614.
14. Lapostolle, Sebbah JL, Couvreur J et al.: Risk factors for onset of hypothermia in trauma victims: the HypoTraum study. Crit Care 2012; 16(4): R142.
15. Ireland S, Endacott R, Cameron P et al.: The incidence and significance of accidental hypothermia in major trauma – a prospective observational study. Resuscitation 2011; 82(3): 300-306.
16. Trentzsch H, Huber-Wagner S, Hildebrand F et al.: Hypothermia for prediction of death in severely injured blunt trauma patients. Shock 2012; 37(2): 131-139.
17. Søreide K: Clinical and translational aspects of hypothermia in major trauma patients: from pathophysiology to prevention, prognosis and potential preservation. Injury 2014; 45(4): 647-654.
18. Eidstuen SC, Uleberg O, Vangberg G: When do trauma patients lose temperature? A prospective observational study. Acta Anaestesiol Scand 2018; 62(3): 384-393.
19. Bennett BL, Holcomb JB: Battlefield Trauma-Induced Hypothermia: Transitioning the Preferred Method of Casualty Rewarming. Wilderness Environ Med 2017; 28(2S): S82-S89.
20. Gregory JS, Flancbaum L, Townsend MC et al.: Incidence and timing of hypothermia in trauma patients undergoing operations. J Trauma 1991; 31(6): 795-798.
21. Bernabei AF, Levison MA, Bender JS: The effects of hypothermia and injury severity on blood loss during trauma laparotomy. J Trauma 1992; 33(6): 835-839.
22. Kurz A, Sessler DI, Christensen R et al.: Heat balance and distribution during the core-temperature plateau in anesthetized humans. Anesthesiology 1995; 83(3): 491-499.
23. Arlt M, Philipp A, Voelkel S et al.: Extracorporeal membrane oxygenation in severe trauma patients with bleeding shock. Resuscitation 2010; 81(7): 804-809.
24. Hildebrand F, Probst C, Frink M et al.: Importance of hypothermia in multiple trauma patients. Unfallchirurg 2009; 112(11): 959-964.
25. Mommsen P, Zeckey C, Frink M et al.: Accidental hypothermia in multiple trauma patients. Zentralbl Chir 2012; 137(3): 264-269.
26. Mommsen P, Andruszkow H, Frömke C et al.: Effects of accidental hypothermia on posttraumatic complications and outcome in multiple trauma patients. Injury 2013; 44(1): 86-90.
27. Balvers K, Van der Horst M, Graumans M et al.: Hypothermia as a predictor for mortality in trauma patients at admittance to the Intensive Care Unit. J Emerg Trauma Shock 2016; 9(3): 97-102.
28. Sundberg J, Estrada C, Jenkins C et al.: Hypothermia is associated with poor outcome in pediatric trauma patients. Am J Emerg Med 2011; 29(9): 1019-1022.
29. Shafi S, Elliott AC, Gentilello L: Is hypothermia simply a marker of shock and injury severity or an independent risk factor for mortality in trauma patients? Analysis of a large national trauma registry. J Trauma 2005; 59(5): 1081-1085.
30. Beilman GJ, Blondet JJ, Nelson TR et al.: Early hypothermia in severely injured trauma patients is a significant risk factor for multiple organ dysfunction syndrome but not mortality. Ann Surg 2009; 249(5): 845-850.
31. Waibel BH, Schlitzkus LL, Newell MA et al.: Impact of hypothermia (below 36 degrees C) in the rural trauma patient. J Am Coll Surg 2009; 209(5): 580-588.
32. Waibel BH: Hypothermia in trauma patients: predicting the big chill. Crit Care 2012; 16(5): 155.
33. Webster B, Mellor A, Smith D: Anaesthetic priorities in pre-hospital trauma care. Anaesth Intens Care Med 2011; 12(9): 377-379.
34. Hess JR, Brohi K, Dutton RP et al.: The coagulopathy of trauma: a review of mechanisms. J Trauma 2008; 65(4): 748-754.
35. Davenport R: Pathogenesis of acute traumatic coagulopathy. Transfusion 2013; 53 (suppl. 1): 23S-27S.
36. Lundgren P, Henriksson O, Naredi P et al.: The effect of active warming in prehospital trauma care during road and air ambulance transportation-a clinical randomized trial. Scand J Trauma Resusc Emerg Med 2011; 19: 59.
37. Alèx J, Karlsson S, Saveman BI: Patient’s experiences of cold exposure during ambulance care. Scand J Trauma Resusc Emerg Med 2013; 21: 44.
38. Lee SH, Kim HK, Park SC et al.: The effect of infusion rate and catheter length on the temperature of warming fluid Korean. J Anesthesiol 2010; 58(1): 31-37.
39. Cannon JW: Hemorrhagic shock. N Engl J Med 2018; 378(4): 370-379.
40. Darocha T, Kosinski S, Jarosz A et al.: The chain of survival in hypothermic circulatory arrest: encouraging preliminary results when using early identification, risk stratification and extracorporeal rewarming. Scand J Trauma Resusc Emerg Med 2016; 24: 85.
