Maja Stańczyk1, Ronald Lukashevich1-3, Aleksandra Gorzkowska1-3, Paulina Urbańska1-3, Piotr Laskowski1, Dominik Woźniak1-3, Zygmunt Stopa1, Piotr Regulski2, 4, *Robert Franczyk3
Computed tomography-assisted morphological assessment of the components of the temporomandibular joint – a pilot study
Morfologiczna ocena składowych stawu skroniowo-żuchwowego na podstawie tomografii komputerowej – badanie pilotażowe
1Department of Cranio-Maxillofacial Surgery, Oral Surgery and Implantology, Medical University of Warsaw, Poland
Head of Department: Paweł Zawadzki, post-doctoral degree
2Department of Dental and Maxillofacial Radiology, Medical University of Warsaw, Poland
Head of Department: Professor Kazimierz Szopiński, MD, PhD
3Department of Descriptive and Clinical Anatomy, Center of Biostructure Research, Medical University of Warsaw, Poland
Head of Department: Professor Bogdan Ciszek, MD, PhD
4Interdisciplinary Center for Mathematical and Computational Modelling, University of Warsaw, Poland
Head of Center: Marek Michalewicz, PhD
Streszczenie
Wstęp. Zaburzenia funkcji stawów skroniowo-żuchwowych stanowią coraz częstszy problem diagnostyczno-terapeutyczny, jednak uniwersalne parametry analizy radiologicznej nie zostały opracowane.
Cel pracy. Porównanie wartości wybranych parametrów radiologicznych stawów skroniowo-żuchwowych u pacjentów bez objawów artropatii oraz z dolegliwościami ze strony układu stomatognatycznego.
Materiał i metody. Retrospektywna analiza zapisów tomografii komputerowej pacjentów Kliniki Chirurgii Czaszkowo-Szczękowo-Twarzowej, Chirurgii Jamy Ustnej i Implantologii WUM oraz Zakładu Radiologii Stomatologicznej i Szczękowo-Twarzowej WUM. Wszystkie badania były elementem standardowego procesu diagnostycznego dolegliwości chorych. Wyodrębniono dwie grupy pacjentów: 1. bez dolegliwości ze strony układu stomatognatycznego, 2. z zaburzeniami funkcji stawów skroniowo-żuchwowych. Oceniano kształt głów żuchwy. Porównano parametry: odległość bocznych punktów głów żuchwy (GL-GP), wymiar boczno-przyśrodkowy i przednio-tylny głów żuchwy, kąt nachylenia osi poziomej głów żuchwy do osi poprowadzonej przez skrajnie tylne punkty głów żuchwy, odległości między głową żuchwy a dołem żuchwowym.
Wyniki. Grupa 1 liczyła 40 osób (13 kobiet, 27 mężczyzn), grupa 2 – 16 osób (14 kobiet, 2 mężczyzn). Najczęstszym typem głowy żuchwy w grupie 1 był wypukły (14 osób), a w grupie 2 – płaski (8 osób). Największe różnice między grupami uzyskano dla średnich wartości pomiarów: GL-GP (120,35 mm w grupie 1; 115,4 mm w grupie 2), wymiarze boczno-przyśrodkowym i przednio-tylnym głowy żuchwy (19,7 vs. 18,14 mm; 8,03 vs. 7,04 mm, odpowiednio dla grup 1 i 2).
Wnioski. Obrazowanie z wykorzystaniem tomografii komputerowej pozwoliło na dokładną analizę wymiarów poszczególnych składowych stawu skroniowo-żuchwowego (ssż). Pomiary wybranych struktur anatomicznych ssż omówionych w niniejszej pracy powinny być elementem diagnostyki pacjentów z dysfunkcją narządu żucia.
Summary
Introduction. Temporomandibular joint (TMJ) disorders are a common diagnostic problem. No universal radiological parameter of the analysis was introduced.
Aim. Comparison of values of selected radiological parameters between asymptomatic patients and those with the TMJ arthropathy.
Material and methods. Retrospective analysis of CT scans of patients of the Department of Dental and Maxillofacial Radiology and the Department of Cranio-Maxillofacial Surgery, Oral Surgery and Implantology, Medical University of Warsaw. Patients were divided into two groups: 1. without TMJ disorders, 2. with TMJ dysfunction symptoms. Following parameters of heads of mandible were analyzed bilaterally: shape, anteroposterior and lateromedial dimensions, the distance between lateral points of both heads (HL-HR), distance between a head and the mandibular fossa. The angle between the horizontal axis of the head of mandible and the line drawn by posterior points of heads of mandible was measured.
Results. The most common type of the head of mandible in group 1 (40 patients; 13 women, 27 men) was convex (14 patients), in group 2 (16 patients; 14 women, 2 men) – plane (8 patients). Significant differences between groups were obtained for: GL-GP (group 1 – 120.35 mm, group 2 – 115.4 mm), dimensions of heads of mandible: lateromedial – 19.7 mm, 18.14 mm, anteroposterior – 8.03 mm, 7.04 mm for group 1 and 2, respectively.
Conclusions. Computed tomography allowed for an accurate analysis of the TMJ components. Measurements of structures discussed in this work should be a part of the diagnosis of patients with TMJ dysfunction.
Introduction
Temporomandibular symptoms have become an increasingly common diagnostic and therapeutic problem in everyday medical practice. Arthropathies affect 20-30% of the population at different ages, including 3-7% of patients requiring treatment (1-3). Although the disorders are usually diagnosed in women 20-40 years of age, they are also found in children and adolescents (4). Stomatognathic dysfunctions are an aetiologically and symptomatically heterogeneous group, and they may involve both temporomandibular joints and masticatory muscles (3, 5, 6). Artropathies are manifested by pain (ear, the parotid-masticatory area, head), limited mandibular mobility, and acoustic symptoms (i.e. crackling, crepitation). Chronic pain in temporomandibular disorder (TMD) may lead to depression and reduced quality of life (7). The variety of TMD symptoms may pose a significant diagnostic problem (5, 8, 9). In addition to medical history and physical examination, diagnostic imaging also plays an important role (10, 11). Panoramic radiography is a basic plain x-ray showing some of the pathological processes that may occur in the temporomandibular bony structures (2, 12). However, it allows to obtain a cross-sectional view of the mandibular head on a single film, which prevents overall assessment of temporomandibular structures. Furthermore, the dimensions of anatomical structures may be distorted. Therefore, condylar processes and the articular surface of the temporal bone are assessed based on computed tomography (including cone beam computed tomography – CBCT) and magnetic resonance imaging (MRI). CT allows for the assessment of degenerative lesions of temporomandibular bones, such as deformity, flattening and erosion of articular surfaces, subchondral densities and the presence of osteophytes and loose intra-articular bodies (7, 10). When assessing articular head surfaces, their anatomical variations (including the flat type), which make their differentiation with the initial symptoms of TMD difficult, should be considered (11). Significantly reduced effective dose of radiation received by the patient is an advantage of CBCT compared to conventional CT. Worse visualisation of soft tissues compared to MRI, which allows for a precise assessment of soft tissues, particularly articular disc location and displacement, its deformity and perforation, as well as articular effusion and adhesions, is a limitation of CT imaging in the diagnosis of TM diseases (5, 6, 13, 14). MRI is also the best technique to trace the dynamics of arthropathy development (6, 14). Despite its multiple advantages, MRI is not a tool used in the first stage of diagnosis of temporomandibular pain. Therefore, it is important to improve the analysis of CT and CBCT images. There is currently no universal parameter for the diagnosis of early-stage temporomandibular arthropathy or differentiation between pathological processes and anatomical variations (15, 16).
Aim
The aim of the study was to compare selected TM radiographic parameters in non-arthropathic patients and those presenting with stomatognathic symptoms.
Material and methods
We performed a retrospective analysis of CT records of patients diagnosed in the Department of Cranio-Maxillofacial Surgery, Oral Surgery and Implantology, and the Department of Dental and Maxillofacial Radiology of the Medical University of Warsaw. All scans were performed as part of standard diagnostic process. Patients were classified into two groups:
1. group 1 – patients with no stomatognathic symptoms,
2. group 2 – patients with temporomandibular dysfunction.
Inclusion criteria:
– age over 18 years,
– diagnosis in the Department of Cranio-Maxillofacial Surgery, Oral Surgery and Implantology, or the Department of Dental and Maxillofacial Radiology of the Medical University of Warsaw,
– craniofacial CT,
– group 2 patients – additionally: known temporomandibular dysfunction (medical history or physical examination findings of facial muscle pain, limited or abnormal joint motion, signs of articular disc displacement that are not a consequence of diseases included in the exclusion criteria).
Exclusion criteria:
– facial bone fractures,
– cysts, tumours or fractures within the temporomandibular joints,
– CT failure to fully show the temporomandibular joints.
Based on a CT scan, we assessed the shape of mandibular heads (angular, rounded, flattened, convex) and measured the following parameters in all patients:
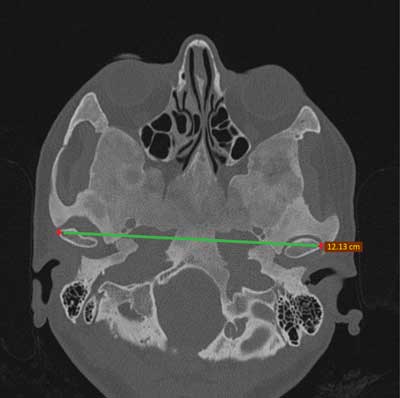
– the distance between lateral points of mandibular heads (HL-HR) (fig. 1),
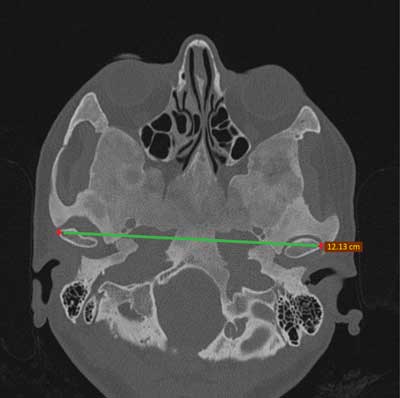
Fig. 1. The distance between lateral points of mandibular heads (HL-HR)
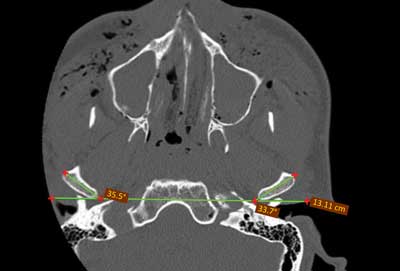
– the largest lateromedial (l-m) and anteroposterior (a-p) dimension of mandibular heads (fig. 2),

Fig. 2. The largest lateromedial (l-m) and anteroposterior (a-p) dimension of mandibular heads
– the inclination angle (α) of the horizontal axis of mandibular heads to an axis running through the most posterior points of both mandibular heads (fig. 3),
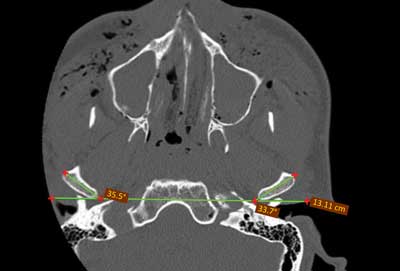
Fig. 3. The inclination angle (α) of the horizontal axis of mandibular heads to an axis running through the most posterior points of both mandibular heads
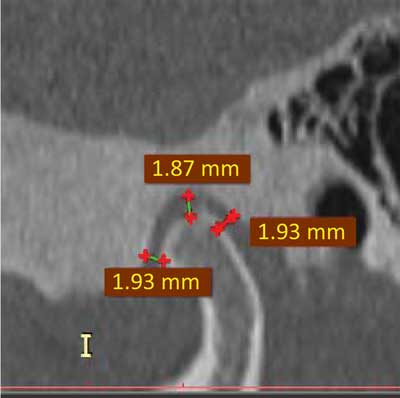
– distances between mandibular heads and the most anterior (s1), medial (s2) and posterior (s3) point of the mandibular fossa assessed in a sagittal plane (fig. 4).
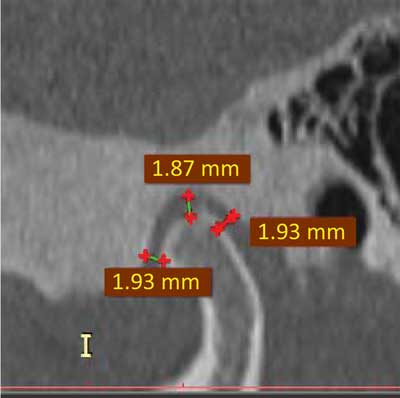
Fig. 4. Distances between mandibular heads and the most anterior (s1), medial (s2) and posterior (s3) point of the mandibular fossa assessed in a sagittal plane
In the first stage of the study, we compared the above mentioned left- and right-sided parameters in group 1 to assess statistically significant differences (anatomical variations) in patients with no symptoms of temporomandibular arthropathy. We then performed an intergroup comparison of these parameters.
The study was approved by the Bioethics Committee of the Medical University of Warsaw (AUBE/207/17).
Results
Group 1 included 40 patients (13 women and 27 men) aged 21-70 years, group 2 included 16 patients (14 women, 2 men) aged 22-64 years.
The most common types of mandibular heads (tab. 1) were the convex type in group 1 (n = 14) and the flattened type in group 2 (n = 8). No significant differences were found in the analysed parameters between the left and the right side in group 1 (tab. 2).
Tab. 1. Types of the head of mandible in study groups
| | Group 1 | Group 2 |
| Type of head of mandible | Left side | Right side | Left side | Right side |
| angular | 6 | 5 | 2 | 2 |
| rounded | 5 | 8 | 2 | 2 |
| flattened | 14 | 12 | 6 | 8 |
| convex | 14 | 12 | 6 | 4 |
Tab. 2. Values of analysed parameters in group 1 (patients no stomatognathic symptoms)
| Parameter | Left side (avg. ± SD) | Right side (avg. ± SD) |
| l-m (mm) | 19.14 ± 1.71 | 19.69 ± 2.03 |
| a-p (mm) | 8.03 ± 1.21 | 7.97 ± 1.35 |
| angle α (°) | 27.78 ± 5.34 | 26.97 ± 5.35 |
| s1 (mm) | 2.85 ± 1.11 | 2.94 ± 1.55 |
| s2 (mm) | 1.7725 ± 0.67 | 1.96 ± 0.80 |
| s3 (mm) | 2.94 ± 1.56 | 3.07 ± 1.84 |
avg. – average; SD – standard deviation; l-m – lateromedial dimension of the head of mandible; a-p – anteroposterior dimension of the head of mandible; inclination angle (α) – between the axis of the head of mandible and the horizontal axis; s1-3 – the distance between the head of mandible and the most anterior (s1), middle (s2) posterior (s3) point of the mandibular fossa
A comparison between group 1 and 2 showed differences in the distance between the lateral points of mandibular heads (HL-HR): 120.35 ± 4.36 mm in group 1 vs. 115.4 ± 5.8 mm in group 2; as well as in the lateromedial dimensions of the right mandibular head (19.69 ± 2.03 mm vs. 18.14 ± 1.96 mm), and anteroposterior dimensions of the left mandibular head (8.02 ± 1.21 mm vs. 7.04 ± 1.14 mm) (tab. 3, fig. 5).
Tab. 3. Values of analysed parameters in study groups (1 – patients with no stomatognathic symptoms, 2 – patients with temporomandibular dysfunction)
| | Group 1 | Group 2 |
| Parameter | Left side (avg. ± SD) | Right side (avg. ± SD) | Left side (avg. ± SD) | Right side (avg. ± SD) |
| l-m (mm) | 19.14 ± 1.71 | 19.69 ± 2.03 | 17.72 ± 2.51 | 18.14 ± 1.96 |
| a-p (mm) | 8.02 ± 1.21 | 7.97 ± 1.35 | 7.04 ± 1.14 | 7.62 ± 1.01 |
| angle α (°) | 27.78 ± 5.34 | 26.97 ± 5.35 | 27.90 ± 5.88 | 28.32 ± 6.61 |
| s1 (mm) | 2.85 ± 1.11 | 2.94 ± 1.55 | 2.27 ± 1.35 | 2.49 ± 2.02 |
| s2 (mm) | 1.77 ± 0.67 | 1.96 ± 0.80 | 2.05 ± 0.90 | 2.11 ± 0.67 |
| s3 (mm) | 2.94 ± 1.56 | 3.07 ± 1.84 | 2.63 ± 0.95 | 3.09 ± 1.51 |
avg. – average; SD – standard deviation; l-m – lateromedial dimension of the head of mandible; a-p – anteroposterior dimension of the head of mandible; inclination angle (α) – between the axis of the head of mandible and the horizontal axis; s1-3 – the distance between the head of mandible and the most anterior (s1), middle (s2) posterior (s3) point of the mandibular fossa
Fig. 5. Dimentions of heads of mandible in study groups (avg. values)
a-p – anteroposterior dimension; l-m – lateromedial dimension
Discussion
Improvement of diagnostic methods used in temporomandibular dysfunction has gained importance due to the increasing number of patients presenting with this pathology (1-3). Since computed tomography in one of the techniques used in the primary diagnostic process in temporomandibular disorders, it is extremely important to develop additional methods for the assessment of such CT imaging findings to detect pathology already at its early stages.
Hatcher and Lotzmann described stages of TMJ degenerative lesions based on panoramic radiographs (10). According to the authors, initial cartilaginous lesions are imperceptible. At further stages, deformation of mandibular head surfaces occurs, and may be accompanied by detectable bone defects. Careful analysis and differentiation with normal anatomical variations of mandibular heads, the flattened type in particular, are necessary in the initial detectable stage of arthropathy (11). Such an analysis will not be possible in the absence of previous patient’s TMJ radiographs for comparison.
Devireddy et al. proposed parameters for the assessment of the efficacy of restoring proper topographic relationships after treating fractures of condylar processes of mandible (16). However, comparison with our group of patients is unreliable due to the small sample size (n = 10) and a different aim of the assessed measurements in the cited study.
Inter-group differences were found for the size of mandibular heads (anteroposterior and lateromedial), with reduced values in the study group. It should be noted that these changes were unilateral. For advanced lesions, bilateral measurements should be compared with percentile chart standards, which are currently not available. This confirms the need for further research and measurements in patients with no TMJ symptoms to obtain reference values for the measurements in patients with arthropathy.
Small sample size was the main limitation of our research. The aim of this study was to assess the possibility to measure TMJ components. The study will be continued in a larger patient population, including patients with functional disorders. To conclude, CT imaging allows for differential diagnosis of pain in the TMJ region and a detailed analysis of joint components. As in the case of panoramic radiograph, altered size of mandibular heads is the first sign of TMJ dysfunction. The study will be continued to specify reference parameters and increase statistical power of the analysis.
Conclusions
CT imaging allowed for detailed analysis of the dimensions of individual components of the temporomandibular joint. Measurement of selected anatomical TMJ structures discussed in this paper should be incorporated in the diagnosis of patients with masticatory dysfunction. Continuation of this research will enable collection of reliable data on both normal TMJ morphology and arthropathic changes.
Piśmiennictwo
1. Aiken A, Bouloux G, Hudgins P: MR Imaging of the Temporomandibular Joint. Magn Reson Imaging Clin N Am 2012; 20(3): 397-412.
2. Gauer RL, Semidey MJ: Diagnosis and treatment of temporomandibular disorders. Am Fam Physician 2015; 91(6): 378-386.
3. Kurpiel P, Kostrzewa-Janicka J: Dysfunkcja układu ruchowego narządu żucia – etiologia i klasyfikacja schorzeń. Przegląd piśmiennictwa. Nowa Stomatol 2014; 2: 95-99.
4. Nilsson IM, List T, Drangsholt M: Prevalence of temporomandibular pain and subsequent dental treatment in Swedish adolescents. J Orofac Pain 2005; 19(2): 144-150.
5. Manfredini D, Lombardo L, Siciliani G: Temporomandibular disorders and dental occlusion. A systematic review of association studies: end of an era? J Oral Rehabil 2017; 44(11): 908-923.
6. List T, Jensen RH: Temporomandibular disorders: Old ideas and new concepts. Cephalalgia 2017; 37(7): 692-704.
7. Limchaichana N, Nilsson H, Ekberg EC et al.: Clinical diagnoses and MRI findings in patients with TMD pain. J Oral Rehabil 2007; 34(4): 237-245.
8. Dworkin SF, Le Resche L: Research diagnostics criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique. J Craniomandib Disord 1992; 6: 301-355.
9. Von Korff M, Dworkin SF, Le Resche L et al.: An epidemiologic comparison of pain complaints. Pain 1988; 32: 173-183.
10. Hatcher DC, Lotzmann U: Temporomandibular joint imaging as a diagnostic aid. J Gnathol 1992; 11: 45-55.
11. Kostrzewa-Janicka J, Anulewicz A, Mierzwińska-Nastalska E: Aspekty budowy makroskopowej i mikroskopowej stawów skroniowo-żuchwowych na podstawie piśmiennictwa. Protet Stomatol 2007; LVII(2): 97-104.
12. Boeddinghaus R, Whyte A: Trends in maxillofacial imaging. Clin Radiol 2018; 73(1): 4-18.
13. Al-Salehl MAQ, Alsufyani NA, Saltaji H et al.: MRI and CBCT image registration of temporomandibular joint: a systematic review. Otolaryngol Head Neck Surg 2016; 45: 30.
14. Alarabawy RA, El Ahwal HM, El Sergany MAES, Mehrez WW: Magnetic resonance imaging evaluation of temporo-mandibular joint disorders, criterial analysis and significance in comparison with arthroscopy. Egypt J Radiol Nucl Med 2016; 47: 467-475.
15. Shahidi S, Vojdani M, Paknahad M: Correlation between articular eminence steepness measured with cone-beam computed tomography and clinical dysfunction index in patients with temporomandibular joint dysfunction. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 116(1): 91-97.
16. Devireddy SK, Kumar RVK, Gali R et al.: Three-dimensional assessment of unilateral subcondylar fracture using computed tomography after open reduction. Indian J Plast Surg 2014; 47(2): 203-209.