Agata Wasilewska, *Lidia Zawadzka-Głos
Abscess and hematoma of the septum – old diagnosis, contemporary treatment options
Krwiak i ropień przegrody nosa – znane rozpoznanie, współczesne metody leczenia
Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Associate Professor Lidia Zawadzka-Głos, MD, PhD
Streszczenie
Wprowadzenie. Krwiak przegrody nosa (KPN) jest nagromadzeniem krwi lub ropy (wtedy kwalifikujemy go jako ropień (RPN)) w przestrzeni pomiędzy chrząstką przegrody a płatem śluzówkowo-ochrzęstnowym. Nieleczony prowadzi do deformacji nosa i twarzy oraz opóźnionego wzrostu twarzoczaszki, a nawet do powikłań wewnątrzczaszkowych.
Celem opracowania jest zaprezentowanie i porównanie sposobów postepowania z ropniami i krwiakami przegrody u dzieci w oparciu o literaturę i doświadczenie Kliniki. Proponujemy wytyczne jak leczyć schorzenie.
Materiał i metody. Poddano analizie przypadki 20 pacjentów z ropniem lub krwiakiem przegrody leczonych w Klinice Laryngologii Dziecięcej WUM w okresie od 1 stycznia 2017 do 1 stycznia 2021.
Wyniki. Pacjenci byli w wieku od 8 miesięcy do 18 roku życia. Dziewięcioro miało ropień, a jedenaścioro krwiak przegrody. Wszystkie przypadki ropnia i jeden przypadek nawrotowego krwiaka współistniały z destrukcją chrząstki przegrody. Najczęstszym patogenem w przypadku ropnia był S. aureus (w 1 przypadku MRSA). Wszyscy pacjenci mieli drenaż ropnia w znieczuleniu ogólnym, część rekonstrukcję z użyciem chrząstki homogennej lub autogennej.
Wnioski. Leczenie opiera się na drenażu ropnia lub krwiaka, przepłukaniu jego jamy, umieszczeniu w jamie sączka z teflonu i założeniu tamponady przedniej zapobiegającej jego nawrotowi. Kluczowa jest wczesna rekonstrukcja chrząstki przegrody zniszczonej przez ropień.
Summary
Introduction. Hematoma of the nasal septum is accumulation of the blood or pus in a space between septum and its overlying mucoperichondrium or mucoperiosteum layer. If left untreated, may lead to nose and facial deformity, and delayed facial growth and even to intracranial complications.
Aim of the study is to present and compare different techniques of treatment. We present our guidelines how to treat the condition.
Material and methods. Cases of 20 patients with septal hematoma or abscess hospitalized at the Pediatric Laryngology Clinic between January 1, 2015 and January 1, 2021 were analyzed.
Results. Patients were between 8 months and 18 years of age. Nine present septal abscesses and eleven hematomas. All cases of abscess coexisted with destruction of the septal cartilage as well as one case of recurrent septal hematoma. The most common pathogen was S.aureus, in one case MRSA and that patient neded re-drainage of the abscess. All patients had an abscess/hematoma drained under general anesthesia. Some had septum reconstructed with homologous donor cartilage implants, autologous reconstruction with the auricle cartilage, or complex homologous donor cartilage implant reconstruction.
Conclusion. Treatment is surgical drainage of the hematoma/abscess and inserting suction of teflon strip and anterior nasal package. Crucial is quite early reconstruction of the septum when already damaged by the abscess.
Introduction
Nasal septal hematomas and abscesses are not a common condition in children and are most frequently associated with facial injury. The literature states that they are the result of 2% of nasal injuries and 15% coexist with a fracture of the nasal bones (1). During the injury, there is a interruption of the blood vessels of the mucoperichondrium and accumulation of blood in the space between the septal cartilage and the perichondrium with the formation of the usual bilateral hematoma (1-4).
This occurs in the first hours after the injury, although blood accumulations after 2 days or more of the iatrogenic injury have been observed. Common symptoms include: impaired nasal patency, difficulty in breathing through the nose, change in shape-widening of the nose in the frontal view. Anterior rinoscopy reveals a bluish and red fluctuant swelling of the nasal septum-usually bilateral (fig. 1). In palpation with a cotton stick seems resilient. Hematoma is very clearly visible in a computed tomography with contrast (fig. 2a-e). Due to greater flexibility of the mucoperichondrium in children than in adults, they are less likely to have hematoma of the nasal septum (2).

Fig. 1. Picture of the septal hematoma in examination
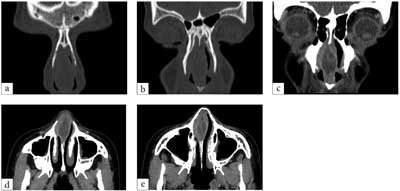
Fig. 2a-e. The image of the abscess in the CT study of the paranasal sinuses without (a, b) and with contrast (3 scans in the frontal plane, the next two in the horizontal)
It should be borne in mind that after injury, hematomas of the lateral wall of the nose of the cartilage area or the back of the nose may occur (2).
The hematoma of the septum is the blood-filled space between the cartilage of the nasal septum and the overlying mucoperichondrium. It is prone to bacterial infection mainly staphylococcal and streptococcal and easily progresses into an abscess. If not drained immediately, the cartilage may undergo necrosis as it is deprived of its nutrition and may undergo its lysis intensified by catechin D-remodeling cartilage enzyme (1, 2). Destruction occurs very quickly, even within days. With an abscess, general fever, pain, redness, tenderness of the nasal tip usually appear. Elevated white blood count and CRP are common. Life-threatening complications in the form of cavernous sinus thrombosis or brain abscesses are rare and associated with late diagnosis and delay in adequate treatment (1).
Other not connected with trauma causes of the nasal septal abscess are dental infections, bacterial sinusitis, furunculus of nasal atrium.
In children, the process of ossification of the nasal septum proceeds gradually with age. Younger children have a larger area of the cartilagous septum and due to constant development of the nose greater incidence of shape of the nose disturbance.
If left untreated in childhood, the abscess of the septum with significant destruction of septal cartilage leads to inhibition of the growth also of the lateral cartilages, bony piramid and maxilla. The younger the child with abscess, the greater the distortion of the structures of the nose and middle face during the growth of the child. Total destruction of the cartilaginous septum will result in an underdeveloped and overrotated saddle nose deformity with columellar retraction and retroposition of the midface (fig. 3).

Fig. 3a-c. Views of a patient with underdeveloped nose due to septal abscess. Patient has saddle nose deformity and broad bony piramid. Before treatment
Septal hematomas can be side-effects of septoplasty or other medical procedures, the literature documents cases where the traumatic factor has not been reported (6).
The procedure of choice is surgical drainage of a hematoma or abscess with a wide incision, in children most often under general anesthesia. Next, we clean the cavity of the hematoma from blood clot or purulent contents, the bacterial swab is collected. We control the integrity of the septum. When loss of cartilage is present, reconstruction with autogous or homogous cartilage has to be done, we insert drain of the teflon plate sutured to the mucosa of the septum, anterior packing both sides is inserted. After two days, we remove the teflon drain, we keep the packing for another two days. Empirical iv broad-spectrum antibiotic therapy is used (1-6).
Aim
Aim of the study is to present and compare different techniques of treatment of septal hematoma and abscess basing on literature and experience of Our Clinic.
We present our guidelines how to treat the condition.
Material and methods
Cases of patients hospitalized at the Pediatric Laryngology Clinic between January 1, 2015 and January 1, 2021 were analyzed.
Patients after nose injury are usually referred for ENT consultations in the 5th day after to assess possible fracture and displacement of nasal bones and qualify patients for reposition of the nasal bones or drainage of the hematoma.
Results
During this period, 20 patients with septal hematoma or an abscess were hospitalized. 2 patients with lateral nasal wall hematoma also requiring drainage were not included into the study. Among the patients were 4 girls and 16 boys. Patients were between 8 months and 18 years of age.
Among all patients in 9 cases septal abscesses and 11 hematomas were found. In 5 cases, a fracture of the nasal bones requiring repositioning occurred simultaneously.
In 15 patients, an abscess or hematoma was present unilaterally – in 9 on the left and 6 on the right side. In five patients on both sides and among this group in 4 coexisted with perforation of the septal cartilage.
All cases of abscess coexisted with destruction of the septal cartilage as well as one case of recurrent septal hematoma.
The size of the perforation of the nasal septum varies from 5 x 10 mm, 10 x 20 mm up to only residual thin cartilage fragment and almost complete destruction. In almost every case, the perforation affected third area of Cottle – attics and the valve field. Bacterial swab was collected in patients with purulent content in the mucoperichondrial space.
The most common pathogen was S. aureus, in 1 case MRSA and that patient neded re-drainage of the abscess.
All patients received intravenous antibiotic therapy: 2nd generation cefalosporin in combination with clindamycin, less commonly amoxicillin with clavulonic acid. Of course, antibiotic therapy was corrected due to antibiogram when received.
All patients had an abscess/hematoma drained under general anesthesia along with a reposition of the nasal bones when needed. Five patients had no other surgery. Three patients had septum reconstructed with homologous donor cartilage implants. One patient underwent an autologous reconstruction with the auricle cartilage 12 days after the drainage. In one patient, a complex homologous donor cartilage implant reconstruction was done 4 months after drainage during open acces septorinoplasty.
In all but one patient, the hematoma/abscess was due to injury, in 1 case it was iatrogenic after septoplasty. In all cases, good nasal function and aesthetics were achieved.
Discussion
Hematomas and abscesses of the nasal septum if left untreated lead to inhibition of the growth of the nose and maxilla. Total destruction of the cartilaginous septum results in an underdeveloped and overrotated saddle nose deformity with columellar retraction and retroposition of the midface with other consequences: nasal obstruction, breathing disorders, psychosocial problems. Fortunately, the rarely seen nasal deformity is a kind of stigmatization and has negative association. What is necessary to avoid complications is to examine every patient after nasal injury, even if there was no fracture of the nasal bones and prompt drainage of the hematoma with reconstruction of cartilage loss.
The normal nasal septum has 2 major growing centers, which are thicker than the surrounding cartilage. These include the sphenodorsal zone, which regulates the length and height of the nose, and the sphenospinal zone, which stimulates the development of the anterior nasal spine and the maxilla. Smaller defects in the thinner part do not seem to interfere with nasal growth. Nevertheless, reconstruction of small defects should be considered to avoid the septal. Damage in other areas may favor baffler perforations, but it’s not as crucial (1).
Literature presents numerous treatment options concearning septal abscesses.
In 1810 Cloquet first described the treatment of the septal abscess by incision and drainage which, however, not prevented nasal deformity and impaired nose function (5).
Drainage was gold standard until the mid-1960s when the first reconstruction of the septum with homologous cartilage was performed at the time of drainage, in acute inflammation. Homologous cartilage stayed intact and prevented the distant effects of the abscess by stabilizing the pyramid of the nose (1, 7, 8) (fig. 4).

Fig. 4. An example of a homogeneous costal cartilage implant used in the treatment of nasal septum perforation
In contrast, Grymer and Bosch (9) studied identical twin boys, one of whom developed a septal abscess that was reconstructed with homologous cartilage. During follow-up, he developed the expected longterm adverse sequelae of the nose and maxilla.
Cottle et al. propose putting reconstruction off for 8 to 12 weeks to ensure the success of the grafts (10, 11).
It seems that a favorable option is the use of autogenous cartilage. Such cartilage, in addition to the support function, has the ability to grow (1), and has a limited risk of resorption, infection and extrusion. According to studies, chondrocytes from perichondrium do not migrate to homogeneous irradiated cartilage, but migrate to autogenous. Delayed reconstruction with autologous osteochondral grafts harvested from the rib provides good reconstructive possibilities. This is especially good donor site for large osteocartilaginous reconstructions of the dorsum and columella. For small reconstructions, the auricular cartilage is used (5).
Example of a promising option is an autogenic implant fixed on a polydioxanone plate (1).
In order to minimise the number of procedures, a simultaneous cartilage implantation into the abscess cavity during drainage is optimal (12).
Conclusions
Septal hematomas and abscesses are still medical challenge. They require prompt drainage and inspection and may necessitate reconstruction of the nasal septum with homogenous or autogenous cartilage. Autogenous cartilage is the material of choice, but type of reconstruction depends on the experience and capabilities of the resort. Crucial is the long-term follow up and possibility to perform septorinoplasty in case of functional and/or aesthetic abnormalitie (13, 14, 15).
Piśmiennictwo
1. Menger DJ, Tabink IC, Trenitè GJ: Nasal septal abscess in children: reconstruction with autologous cartilage grafts on polydioxanone plate. Arch Otolaryngol Head Neck Surg 2008; 134(8): 842-847.
2. Gryczyńska D (red.): Otolaryngologia dziecięca. Wyd. I. Wydawnictwo alfa-medica press, Bielsko-Biała 2007: 33-241.
3. Chandran A, Sakthivel P, Singh CA: A Swollen Nose – Nasal Septal Hematoma. Indian J Pediatr 2020; 87(1): 88.
4. Alvarez H, Osorio J, De Diego JI et al.: Sequelae after nasal septum injuries in children. Auris Nasus Larynx 2000; 27(4): 339-342.
5. Cervera Escario J, Calderón Nájera R, Enríquez de Salamanca J, Bartolomè Benito M: Hematoma y absceso de tabique nasal postraumático en niño [Post-traumatic haematoma and abscess in the nasal septa of children]. Acta Otorrinolaringol Esp 2008; 59(3): 139-141.
6. Huang YC, Hung PL, Lin HC: Nasal septal abscess in an immunocompetent child. Pediatr Neonatol 2012; 53(3): 213-215.
7. Huizing EH: Long term results of reconstruction of the septum in the acute phase of a septal abscess in children. Rhinology 1984; 22: 55-63.
8. Pirsig W: Historical notes and actual observations on the nasal septal abscess especially in children. Int J Pediatr Otorhinolaryngol 1984; 8: 43-54.
9. Grymer LF, Bosch C: The nasal septum and the development of the midface. A longitudinal study of a pair of monozygotic twins. Rhinology 1997; 35: 6-10.
10. Hellmich S: Reconstruction of the destroyed septal infrastructure. Head Neck Surg 1989; 100: 92-94.
11. Cottle MH, Quilty TJ, Buckingham RA: Nasal implants in children and in adults: with preliminary note on the use of ox cartilage. Ann Otol Rhinol Laryngol 1953; 62: 169-175.
12. Bláhová O: Late results of nasal septum injury in children. Int J Pediatr Otorhinolaryngol 1985; 10: 137-141.