Sonia Demianiuk1, Maciej Pilch2, *Lidia Zawadzka-Głos2
An unusual presentation of an intraorbital abscess associated with an extensive dental caries and pulp gangrene in a 14-years old boy with asthma and obesity
Nietypowy obraz ropnia wewnątrzoczodołowego związanego z rozległą próchnicą zębów i rozpadem zgorzelinowym miazgi u 14-letniego chłopca z astmą i otyłością
1Student, member of Students’s Association Otorhino, working by the Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
2Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Associate Professor Lidia Zawadzka-Głos, MD, PhD
Streszczenie
Prezentujemy nietypowy przypadek czternastoletniego pacjenta, który został przyjęty do szpitala w trybie pilnym z obrzękiem prawego oczodołu oraz ograniczoną ruchomością gałki ocznej. Stwierdzona ciężka astma od 7. miesiąca życia oraz otyłość.
Badania radiologiczne wykazały obecność ropnia wewnątrz oczodołu. Stwierdzono również rozległą próchnicę oraz rozkład zgorzelinowy w 17 zębach. Potwierdzono jednostronne zapalenie zatok w tomografii komputerowej.
Leczenie wymagało interwencji chirurgia szczękowego, prowadząc do ekstrakcji 17 zębów. Przeprowadzono drenaż ropnia oraz zastosowano antybiotykoterapię wraz z podaniem glikokortykosteroidów ogólnoustrojowo, pozwalając na natychmiastową poprawę stanu zdrowia pacjenta, prowadząc do wyzdrowienia.
Celem prezentacji przypadku klinicznego jest zaznaczenie związku pomiędzy stanem uzębienia a stanem zapalnym tkanek oczodołu. Infekcja przeniesiona z zębów próchniczych może prowadzić u dzieci do jednostronnego zapalenia zatok, dając ostre powikłania w postaci ropnia wewnątrz oczodołu.
Zalecane jest przykładanie większej uwagi do dbania o higienę jamy ustnej oraz prowadzenia zdrowego trybu życia w celu uniknięcia poważnych powikłań – jest to szczególnie ważne w przypadku pacjentów cierpiących na astmę.
Summary
We present an unusual case of a 14-year-old patient who was admitted as an emergency to the hospital with oedema of right orbit with restricted eye movements. Severe asthma from the seventh month of age and obesity were reported.
Radiologic examination showed the existence of an intraorbital abscess. He also presented an extensive dental caries and pulp gangrene in seventeen teeth and unilateral sinusitis confirmed in the Computed Tomography scan.
Emergency treatment including an oral surgeon’s intervention, which is extraction of seventeen teeth, drainage of the abscess, antibiotics and glucocorticoids was introduced resulting in an immediate improvement of patient’s health status, leading to recovery.
The objective of this clinical presentation is to highlight associations between dental status and cellulitis. Infection from decayed teeth in children can lead to unilateral sinusitis, resulting in severe complications such as an intraorbital abscess.
It is strongly recommended to put more effort into oral hygiene and healthy lifestyle to avoid serious complications – especially in asthmatic patients.
Introduction
Odontogenic infection is the most common cause of unilateral sinusitis (1). Secondary to sinusitis, orbital cellulitis may occur (2), resulting in subperiosteal abscess (3). Extensive dental caries with pulp gangrene is rare in children and should be treated with particular care, as the complications might be even life-threatening (4). This case of a 14-year-old male study seems extraordinary as it required oral surgeon’s intervention and could have been connected with asthma (5, 6). The origins, presentation extent of involvement and treatment are discussed.
Case report
This study was carried out in accordance with the recommendations of ‘name of guidelines, name of committee’ with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki.
A fourteen-years-old boy was admitted to the hospital with dextral orbital complications (eyelids swelling, exophthalmos), including painful eye movements restriction to every direction. Buccal swelling and impaired breathing were reported. He complained of headache, nausea and vertigo. Examination showed extensive dental caries (fig. 1-3).

Fig. 1. Eyelids and buccal swelling

Fig. 2. Eyelids swelling

Fig. 3. Dental caries
Two days before admission to the hospital, the patient had early symptoms such as eyelids swelling and toothache. They were admitted to a stomatologist for a visit. Despite the antibiotic, the symptoms escalated.
Suffering from severe asthma from the seventh month of age, he was treated with Budesonide/Formoterol, Bilastine, Ciclesonide and additionally Salbutamol in a case of dyspnoea.
Spirometry was introduced during the examination in the hospital, combined with the bronchodilatory test, which was negative. During the investigation, it was mentioned that the patient underwent SARS-CoV-2 infection last year.
Bilateral Otitis Externa was present. The tongue was covered with white raid. Reported obesity. What’s more, the boy was allergic to Penicillin and Augmentin. Additionally, he underwent Adenotonsillectomy.
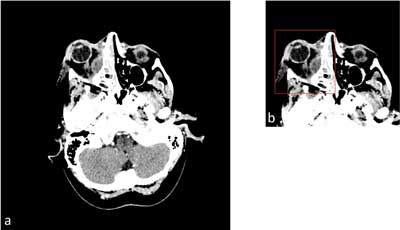
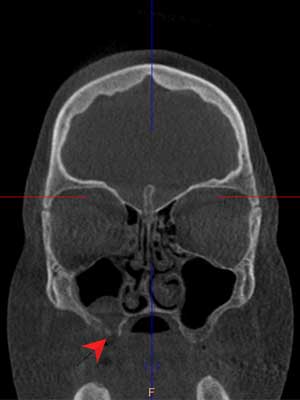
Contrast Enhanced Computed Tomography scanning revealed large intraorbital abscess of the right orbit lying in the extraconal space, below the glob, medially, so the inflammation spread to the lacrimal gland (fig. 4).
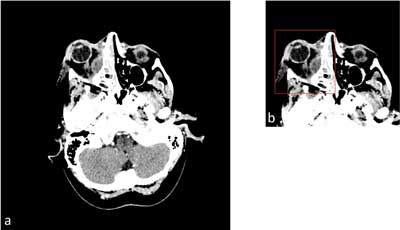
Fig. 4a, b. Exophthalmos and intraorbital abscess of the right orbit
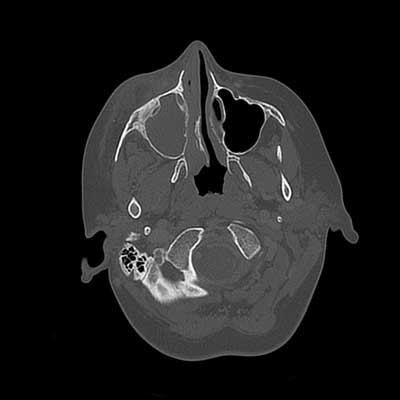
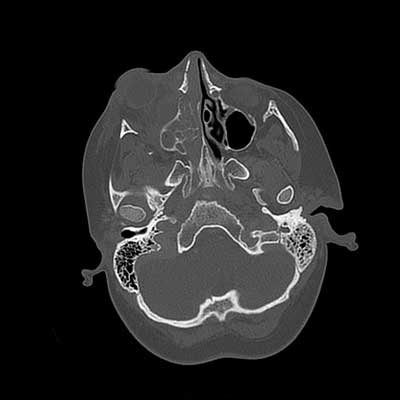
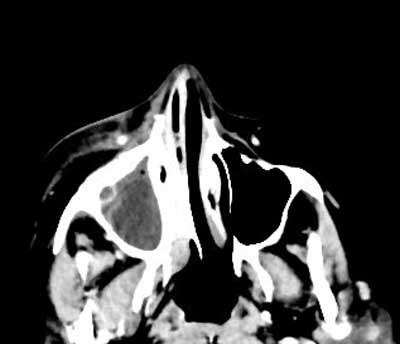
Unilateral right sinusitis was present, revealing the inflammation in ethomid, maxillary and frontal sinuses. The examination confirmed pulp gangrene of seventeen teeth. There were no focal changes in the cerebral area (fig. 5-8).
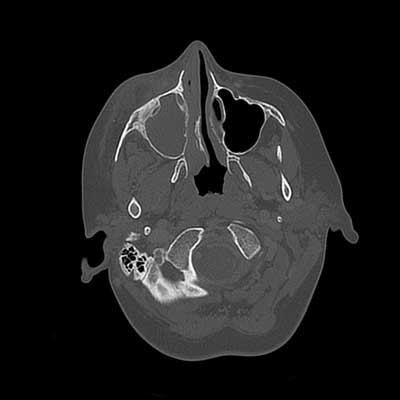
Fig. 5. Inflammation in the right maxillary sinus
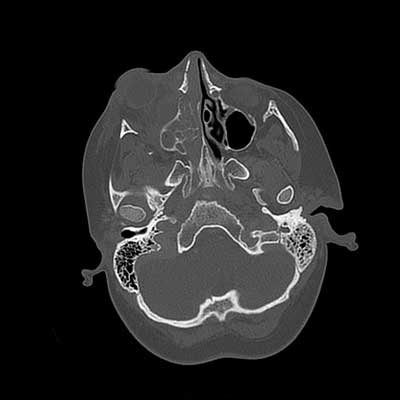
Fig. 6. Inflammation in the right ethmoid sinus and exophthalmos of the right orbit

Fig. 7a, b. Teeth with pulp gangrene
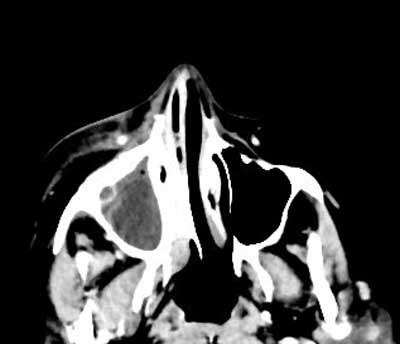
Fig. 8. Pus in the right maxillary sinus
Patient was qualified for surgical treatment including drainage of an abscess from an external approach with sodium chloride rinsing. Endoscopic sinus surgery of maxillary sinus was introduced to extract teeth with a pulp gangrene and reconstruction of an oroantral communication using periosteal-mucous flap was performed.
A systemic, empirical antibiotic therapy, used usually with familiar cases in clinic (7), was given (Ceftriaxone, Clindamycin) with Dexamethasone, analgesic drugs and intravenous hydration. Topical treatment of Ciprofloxacin in the ear canal and Xylometazoline to the nasal cavity were introduced.
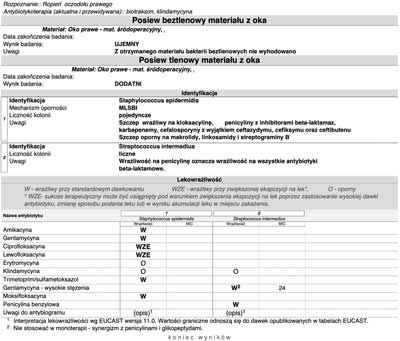
Culture from the drainage content grew resulting in Staphylococcus epidermidis and Staphylococcus intermedius clindamycin and erythromycin – resistant infection. Staphylococcus epidermidis was also found as macrolides, lincosamides, streptogramin B, ceftazidime, cefixime and ceftibuten resistant in MLSBI mechanism. Moreover Pseudomonas aeruginosa was present in the ear canal (fig. 9).
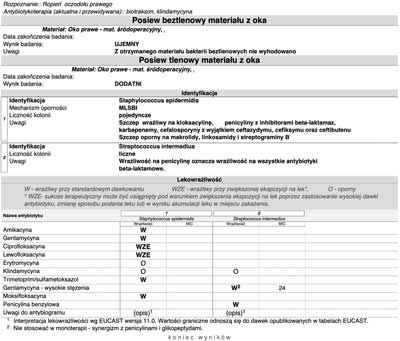
Fig. 9. Antibiogram
The treatment was successful and all symptoms resolved. However, the patient was further referred not only for dental and prosthetic treatment, but also required to remain under the supervision of a pulmonologist, allergologist and dietician.
During the follow up visit in April low sinusitis was revealed, which is normal after such a process and should just be observed. Computed Tomography scan showed an oroantral fistula that was created during the operation. The patient remaining under the care of a stomatologist should be referred for further treatment, including possible surgical closure of the fistula. There were no orbital abnormalities, no signs of recurrence, pain or rhinitis during the second follow up visit (fig. 10).
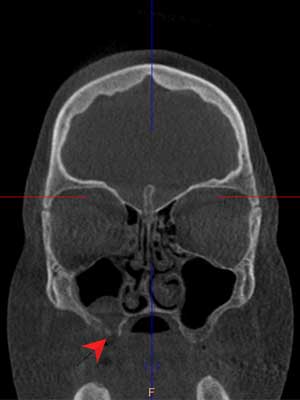
Fig. 10. Oroantral fistula and maxillary sinus
Discussion
In 90% of cases the cellulitis is caused by an infection spreading from the side of the sinuses (7). What’s more, there are other acute complications that may occur, such as visual loss (8) or life-threatening cavernous sinus thrombosis (9). Odontogenic sinusitis is frequently reported in literature, although it is more common in adults and may also result in extrasinus complications, from which those orbital signs appear most often (10).
One of the pathogens, which can cause life-threatening complications is Streptococcus intermedius – a saprophyte of the upper respiratory tract. Despite being a part of the normal microbiota, it is often associated with forming a deep tissues abscesses with the risk of complications in the region of head, neck and central nervous system (11).
According to the patient statement including severe asthma from the seventh month of age and obesity, which is a risk factor for severe asthma (12, 13), we can assume that massive dental caries was connected with long-term asthma treatment (5, 14, 15), lack of oral hygiene and missed stomatological check-up.
Dental control visits should have been introduced at an early stage, so it could have helped to avoid the acute complications. Special dentistric prophylaxis for asthmatic patients would be helpful in saving proper oral condition (16).
Conclusions
This case should serve to emphasize the impact of dental caries, which can lead to unilateral sinusitis, as a predisposing factor for orbital abscess. Lifestyle modification, including good dental care is crucial to avoid acute complications. Proper treatment and regular control visits should ensure fully-controlled dental status.
Piśmiennictwo
1. Matsumoto Y, Ikeda T, Yokoi H, Kohno N: Association between odontogenic infections and unilateral sinus opacification. Auris Nasus Larynx 2015; 42(4): 288-293.
2. Kinis V, Ozbay M, Bakir S et al.: Management of orbital complications of sinusitis in pediatric patients. J Craniofac Surg 2013; 24(5): 1706-1710.
3. Greenberg MF, Pollard ZF: Medical treatment of pediatric subperiosteal orbital abscess secondary to sinusitis. J AAPOS 1998; 2(6): 351-355.
4. Fayle SA, Welbury RR, Roberts JF; British Society of Paediatric Dentistry: British Society of Paediatric Dentistry: a policy document on management of caries in the primary dentition. Int J Paediatr Dent 2001; 11(2): 153-157.
5. Alavaikko S, Jaakkola MS, Tjäderhane L, Jaakkola JJ: Asthma and caries: a systematic review and meta-analysis. Am J Epidemiol 2011; 174(6): 631-641.
6. Agostini BA, Collares KF, Costa FDS et al.: The role of asthma in caries occurrence – meta-analysis and meta-regression. J Asthma 2019; 56(8): 841-852.
7. Zborowska-Skrobanek J, Misiuk-Hojło M: Zakażenia tkanek oczodołu – problem interdyscyplinarny okulistów, laryngologów i chirurgów szczękowo-twarzowych. Dent Med Probl 2007; 44(3): 373-376.
8. Tomaç S, Turgut S: Orbital cellulitis and irreversible visual loss owing to acute sinusitis. Ann Ophthalmol (Skokie) 2006; 38(2): 131-133.
9. Plewa MC, Tadi P, Gupta M: Cavernous Sinus Thrombosis. 2022 Aug 7. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 28846357.
10. Craig JR, Cheema AJ, Dunn RT et al.: Extrasinus Complications From Odontogenic Sinusitis: A Systematic Review. Otolaryngol Head Neck Surg 2022; 166(4): 623-632.
11. Jabłońska-Jesionowska M, Zawadzka-Głos L: Children’s Head and Neck Infections Caused by Streptococcus Intermedius in the Pediatric Otolaryngology Department of Warsaw Medical University. New Medicine 2021; 3: 81-86.
12. Stern J, Pier J, Litonjua AA: Asthma epidemiology and risk factors. Semin Immunopathol 2020; 42(1): 5-15.
13. Peters U, Dixon AE, Forno E: Obesity and asthma. J Allergy Clin Immunol 2018; 141(4): 1169-1179.
14. Chumpitaz-Cerrate V, Bellido-Meza JA, Chávez-Rimache L, Rodríguez-Vargas C: Impact of inhaler use on dental caries in asthma pediatrics patients: A case-control study. Arch Argent Pediatr 2020; 118(1): 38-46.
15. Dembowska E, Jaroń A, Skoczek-Szlosser K et al.: The Effect of Inhaled Corticosteroid Therapy on Periodontal Status in Patients with Asthma. Appl Sci 2022; 12(1): 240.
16. Sköld UM, Birkhed D, Xu JZ et al.: Risk factors for and prevention of caries and dental erosion in children and adolescents with asthma. J Dent Sci 2022; 17(3): 1387-1400.