© Borgis - New Medicine 2/2003, s. 4-11
Lidia Zawadzka-Głos, Mieczysław Chmielik, Anna Gabryszewska, Beata Zając, Małgorzata Badełek-Izdebska
Analysis of indications for bronchoscopy in the Department of Paediatric Otolaryngology in Warsaw from 1998 to 2003
Department of Paediatric Otorhinolaryngology, Medical University of Warsaw, Poland
Head: Prof. Mieczysław Chmielik M.D.
Summary
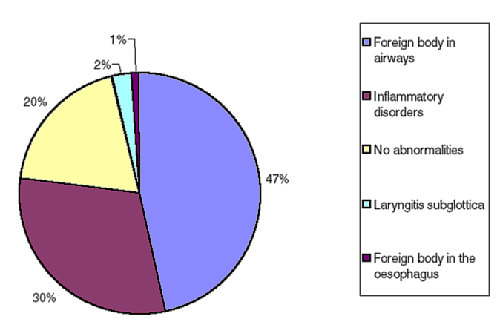
Bronchoscopy is an important method of diagnosis for respiratory tract diseases in children. From January 1998 to June 2003 a total of 290 bronchoscopies were performed on 219 children. The main indications for bronchoscopy were: suspected foreign body aspiration, dyspnoea, stridor, respiratory failure, atelectasis, or bronchopneumonia. The most frequent diagnoses included inflammatory changes without any other pathology of the respiratory tract, inhalation of foreign body, malacia disorders or papillomatosis of the lower respiratory tract, or stenoses and anomalies of the larynx. Bronchoscopy was performed in 81% of cases due to emergency indications.
INTRODUCTION
Bronchoscopy was introduced to clinical practice in 1897 by Killian. Besides physical and radiological examinations and laboratory tests, it is an important method of diagnosis for respiratory tract diseases in children. In addition to giving a direct view of the respiratory passages, bronchoscopy allows treatment of lesions localized in the lower air passages, to take a tissue sample for histopatology or a sample of secretion for microbiological investigation. It is used in such emergency cases as dyspnoea, respiratory failure, atelectasis, and aspiration of a foreign body. It is also used for repeated examinations to monitor long-standing disorders (e.g. tracheobronchomalacia). The dynamics of increase of the signs often indicate bronchoscopy. The safety of bronchoscopy has markedly increased due to ventilating bronchoscopes, which allow the anaesthetist to ventilate the patient with respiratory and anaesthetic gases during an operation. Bronchoscopies may be performed in the smallest, even premature children, and modern optical equipment has improved the quality of the image and consequently increased the diagnostic value.
METHODS
The aim of this retrospective analysis was to examine the indications, diagnostic yield and associated therapeutic procedures in bronchoscopies performed in the Department of Paediatric Otolaryngology in Warsaw from January 1998 to June 2003. The paper analyses the age and sex of patients, and the number of therapeutic and diagnostic bronchoscopies. Primary recognition and diagnosis as a result of bronchoscopy were compared. Special attention was paid to patients under one month of age, with tracheostomy, or patients suspected of having a foreign body in the air passages. The bronchoscopies were carried out under general anaesthesia in an operating theatre, with co-operation with anaesthetist. All children were hospitalized. A rigid Storz bronchoscope of diameter between 2.5 and 6.0 mm, which enabled ventilation of the patient, was used. Rod lens Hopkin´s telescopes were used to improve the view of the respiratory tract, which was recorded on video. Microsurgery tools, argon plasma coagulation or a laser were used in appropriate cases.
MATERIALS AND RESULTS
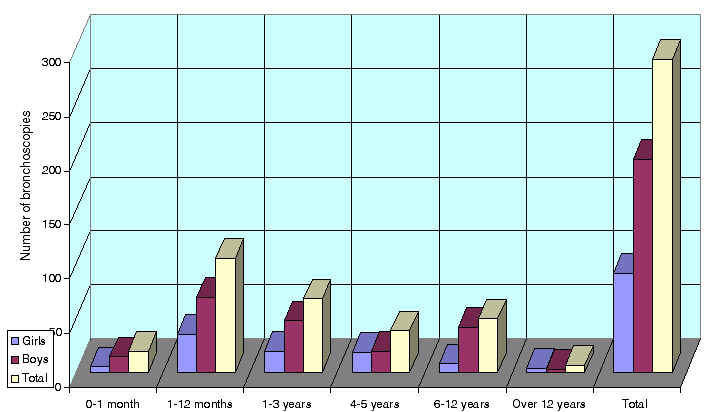
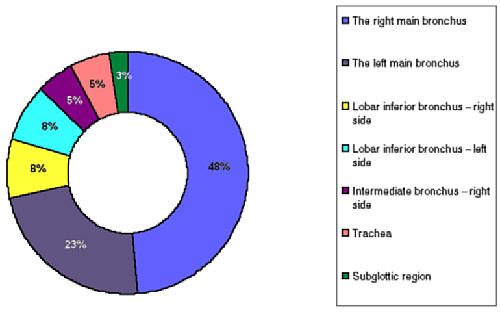
From January 1998 to June 2003 290 bronchoscopies were performed on a total of 219 children. There were 140 boys (63.9%) and 79 girls (36.1%). The mean age was 2.91 years. The youngest child was 4 days of age and the oldest was 18 years old. Twenty children (6.9%) were under 1 month and 126 (43.5%) under 1 year of age. The age distribution is shown in Table 1 and in Figure 1. Bronchoscopy was carried out once on 192 children (87.7%), among them on 67 girls and 125 boys, twice on 17 children, three times on 6 children, and four times or more on 4 children, among whom were on 12 girls and 15 boys. Thirty-two bronchoscopies were performed on one of the patients with severe papillomatosis of the larynx, trachea and lower respiratory tract and with co-existing cystic diseases of the lungs. The analysis of single and multiple bronchoscopies in relation to number of patients is shown in Table 2.
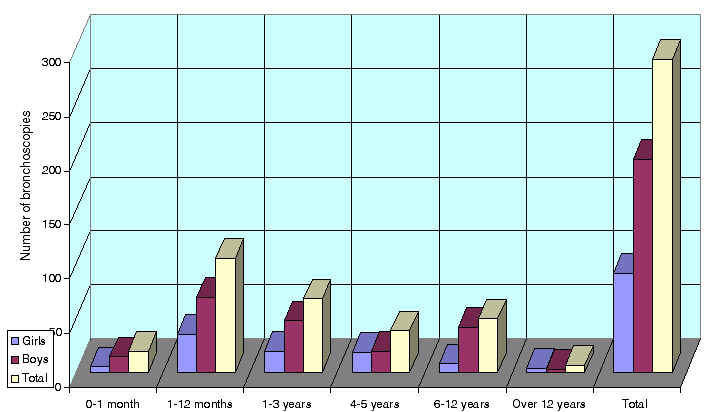
Fig. 1. Age distribution.
Table 1. Age distribution of children.
| Age
| Number of bronchoscopies | | | Percentage of total bronchoscopies |
| Girls | Boys | Total |
| 0-1 months | 5 | 15 | 20 | 6.9% |
| 1-12 months | 36 | 70 | 106 | 36.6% |
| 1-3 years | 20 | 48 | 68 | 23.5% |
| 4-5 years | 19 | 20 | 39 | 13.4% |
| 6-12 years | 8 | 42 | 50 | 17.2% |
| Over 12 years | 4 | 3 | 7 | 2.4% |
| Total | 92 | 198 | 290 | 100% |
Table 2. Number of bronchoscopies per patient
| Number of bronchoscopies per patient | Number of children |
| 1 | 192 |
| 2 | 17 |
| 3 | 6 |
| 4 | 2 |
| 6 | 1 |
| 32 | 1 |
| Total | 219 |
Bronchoscopies were carried out not only for patients hospitalized in the ENT Department, but also in children from other hospital departments, including surgical, endocrynological, nephrological, oncological, cardiological and neonatal. Fifty-seven procedures (19.6% of total) were performed in children from other wards, 32 (11%) from the Intensive Care Unit. The data are shown in Table 3.
Table 3.
| Department | Number of bronchoscopies |
| Intensive Care Unit | 32 |
| Surgical | 10 |
| Endocrynological | 6 |
| Neonate´s Department | 6 |
| Nephrological | 1 |
| Oncological | 1 |
| Cardiological | 1 |
| Total | 57 |
Bronchoscopies had not only a diagnostic but also a therapeutic value. Therapeutic procedures were performed on 99 cases (34.1%), including removal of the foreign body in 38 cases, papillomatosis of the lower respiratory tract in 35 cases, dilation of laryngeal stenosis using argon plasma coagulation in 13 cases, removal of thick mucus from the bronchial tree in 6 cases, and in 2 cases bronchoscopy was used to place a separator in the lumen of the larynx; for laserotherapy of haeman- gioma in 1 case, to remove a mucus plug from the main bronchus in 2 cases, to remove suppurating granulation tissue from the left main bronchus in 1 case, and to remove granulation tissue from the trachea. In 3 children with increasing dyspnoea, respiratory failure and difficulties in intubation, bronchoscopy was performed to insert a guide which enabled insertion of the intubation tube. These children were found to have laryngeal stenosis and required tracheotomy.
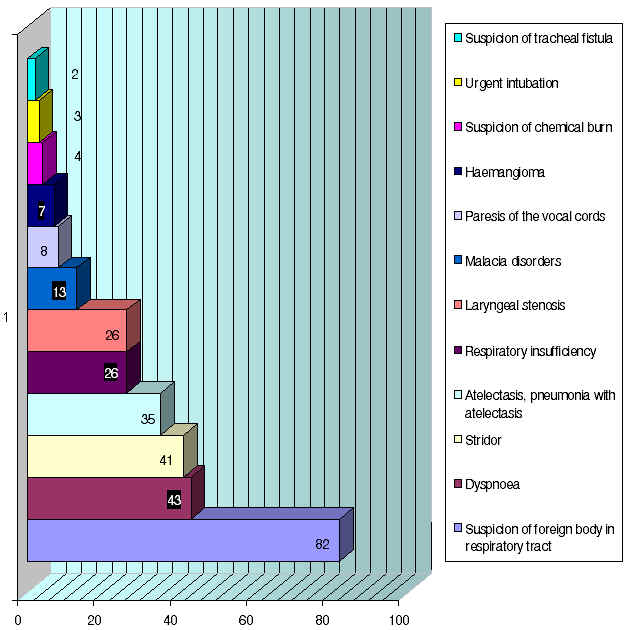
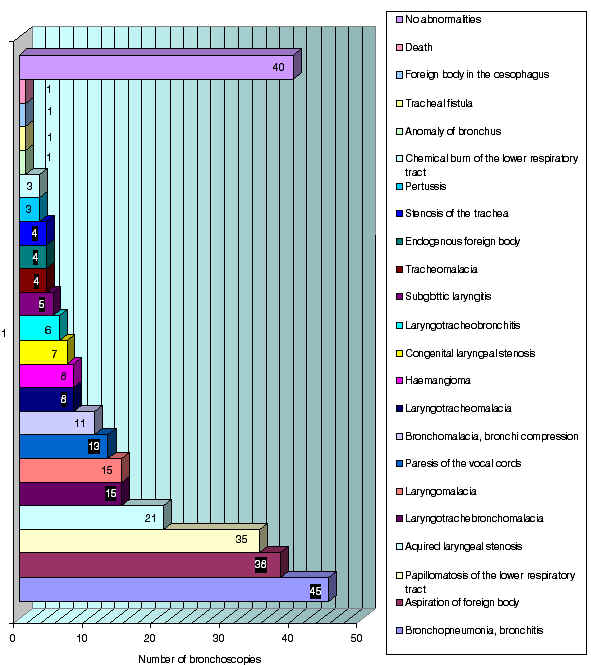
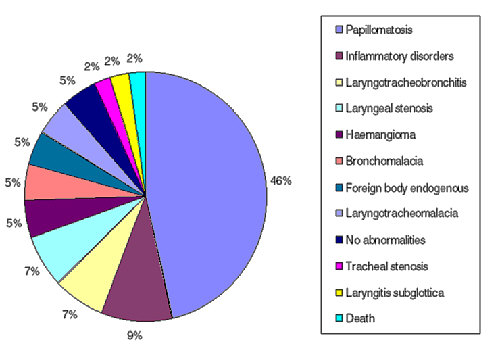
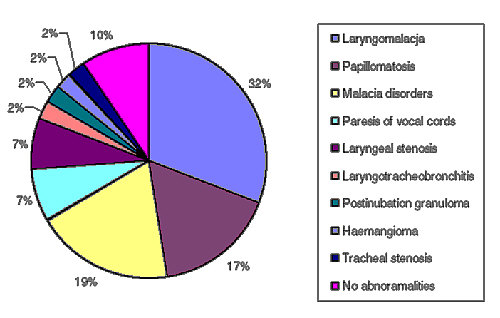
In 55 cases (18.9%), bronchoscopies were performed according to a fixed schedule. The aim of these bronchoscopies was to monitor the course of disease for patients diagnosed earlier: laryngeal stenosis – 26 cases, malacia disorders of the larynx, trachea or bronchi – 13 cases, paresis of the vocal cords – 8 cases, haeman-gioma of the larynx – 7 cases, and 1 child with papillomatosis and tracheostomy. Another 235 (81.0%) bronchoscopies were performed for urgent indications. The primary diagnoses before bronchoscopy are listed in Table 4 and in Figure 2. The final diagnosis was based on endoscopic examination of the respiratory tract, the course of the disease, and other examinations (radiological, microbiological). In one case arrhythmia and circulatory and respiratory failure occurred during bronchoscopy, leading to death. The results are shown in Table 5 and Figure 3.
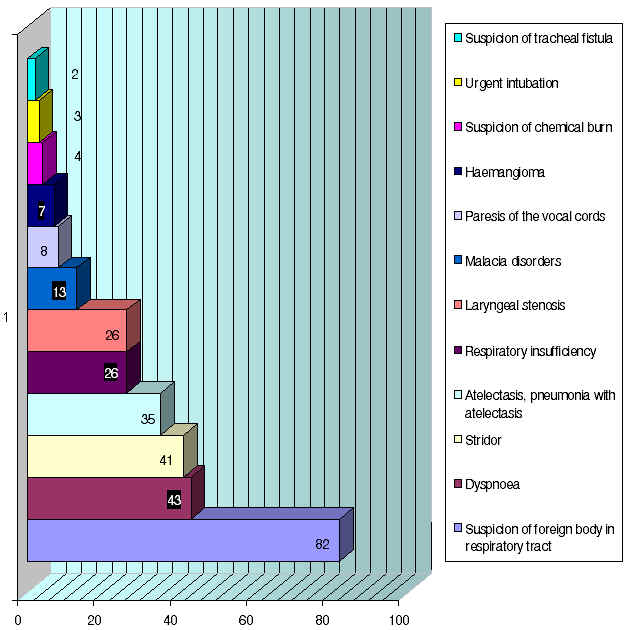
Fig. 2. Preliminary diagnosis.
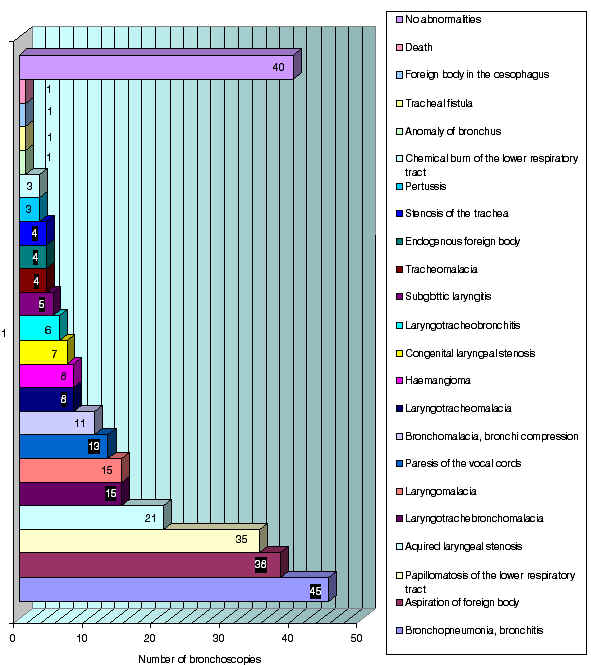
Fig. 3. Final diagnosis.
Table 4. Primary diagnosis before bronchoscopy
| Primary diagnosis | Number of bronchoscopies |
| Suspicion of foreign body in respiratory tract | 82 |
| Dyspnoea | 43 |
| Stridor | 41 |
| Atelectasis, pneumonia with atelectasis | 35 |
| Respiratory insufficiency | 26 |
| Laryngeal stenosis | 26 |
| Malacia disorders | 13 |
| Paresis of the vocal cords | 8 |
| Haemangioma | 7 |
| Suspicion of chemical burn | 4 |
| Urgent intubation | 3 |
| Suspicion of tracheal fistula | 2 |
Table 5. Diagnoses after endoscopy and additional examinations
|
Diagnosis
| Number of cases |
| Bronchopneumonia, bronchitis | 45 |
| Aspiration of foreign body | 38 |
| Papillomatosis of the lower respiratory tract | 35 |
| Acquired laryngeal stenosis | 21 |
| Laryngotrachebronchomalacia | 15 |
| Laryngomalacia | 15 |
| Paresis of the vocal cords | 13 |
| Bronchomalacia, bronchi compression | 11 |
| Laryngotracheomalacia | 8 |
| Haemangioma | 8 |
| Congenital laryngeal stenosis | 7 |
| Laryngotracheobronchitis | 6 |
| Subglottic laryngitis | 5 |
| Tracheomalacia | 4 |
| Endogenous foreign body | 4 |
| Stenosis of the trachea | 4 |
| Pertussis | 3 |
| Chemical burn of the lower respiratory tract | 3 |
| Anomaly of bronchus | 1 |
| Tracheal fistula | 1 |
| Foreign body in the oesophagus | 1 |
| Death | 1 |
| No abnormalities | 40 |
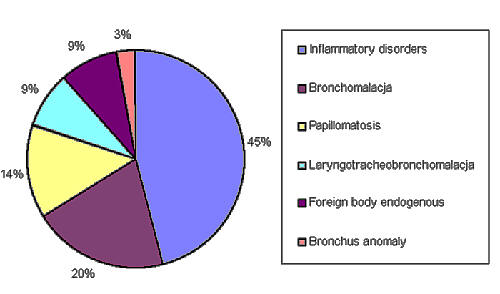
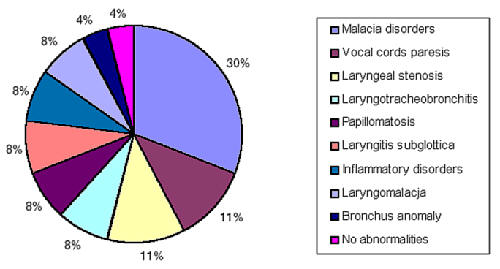
The most frequent, indications for bronchoscopy are shown in Figures 4-8.
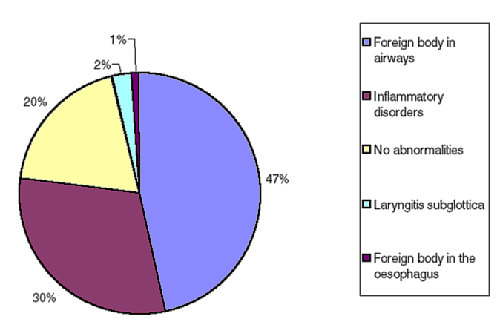
Fig. 4. Suspicion of foreign body in airways.
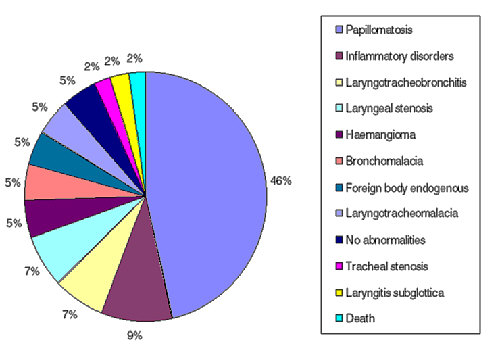
Fig. 5. Dyspnoea.
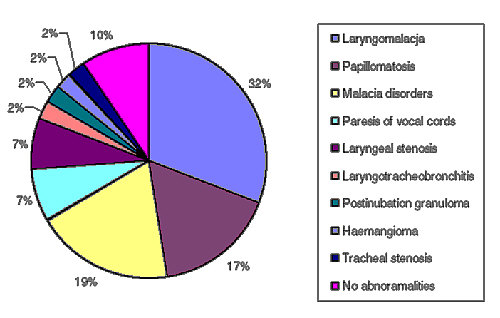
Fig. 6. Stridor.
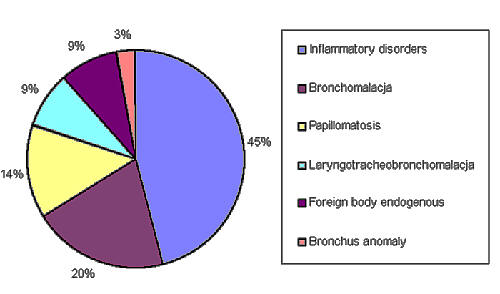
Fig. 7. Atelectasis, pneumonia.
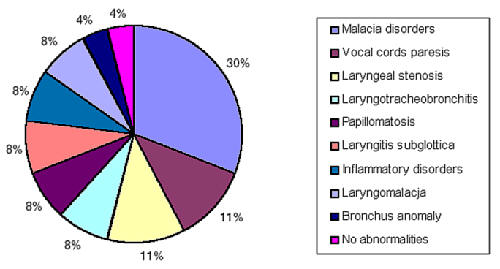
Fig. 8. Respiratory failure.
Bronchoscopies for patients suspected of having a foreign body in the respiratory tract.
Eighty-two (28.3%) bronchoscopies were performed due to suspicion of a foreign body in the respiratory tract. A choking episode or aspiration of a foreign body was described in the history of 57 cases (69.5%). In the other 25 cases (30.5%) the suspicion was based on signs and symptoms and physical and radiological examination. Among the 57 patients after aspiration of a foreign body, in 38 (66.6%) cases the diagnosis was confirmed and the foreign body removed. In one case endoscopy revealed compression of the trachea and the foreign body was removed on esophagoscopy. Numerous foreign bodies were found in 4 children. The most frequent location was the right main bronchus, but foreign bodies were found at different levels in the air passages. This is illustrated in Table 6 and Figure 9.
Table 6. Location of foreign bodies.
| Location of foreign body | Number of cases |
| Single foreign body | Numerous foreign bodies |
| Right main bronchus | 17 | 1 - two fragments
1 - three fragments |
| Left main bronchus | 8 | 1 - three fragments |
| Lobar inferior bronchus - right side | 3 | |
| Lobar inferior bronchus - left side | 2 | 1 - two fragments |
| Intermediate bronchus - right side | 2 | |
| Trachea | 2 | |
| Subglottic region | 1 | |
| Total | 35 | 4 |
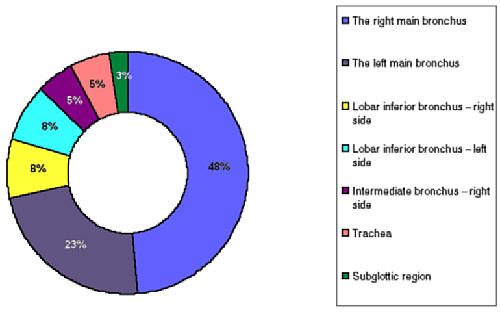
Fig. 9. Localization of foreign body.
The most frequent foreign body was a peanut, in 22 cases. In 4 cases fragments of carrot were removed, in 2 cases a pencil cap, and in single cases: a currant, drawn-pin, sunflower, seed of corn, fruit stalk, half of wooden bead, bread, piece of apple, clips for bedclothes, and a metal screw.
In 18 cases (31.6%), among the 57 cases after a choking episode bronchoscopy was negative. In three cases the child spontaneously expectorated the foreign body before bronchoscopy, and a controlled procedure didn´t reveal other foreign bodies or lesions. In 7 cases (12.3%) inflammation of the air tract and in 1 case a lesion of the bronchial mucous was found. In 25 children without the aspiration episode in anamnesi foreign bodies were not found, and in 18 (72%) of them the bronchitis or pneumonia were recognised.
Sixty-six (22.7%) laryngotracheobronchoscopies were performed in 43 patients (19.6%) with tracheostomy. Laryngeal stenosis was found in 23 children, – haemangioma of the larynx in 5, paresis of the vocal cords in 7, tracho- and/or bronchomalacia in 4, papillomatosis of the larynx and trachea in 2, trauma of vocal cords in 1 case, and no abnormalities were found in a child with Pierre-Robbin syndrome. In 11 cases bronchoscopies were made for emergency indications, in 6 cases because of atelectasis or emphysema of the lung (bronchomalacia was found in 4 children and pneumonia in 2 children), and in at least 5 cases due to increasing dyspnoea (papillomatosis of the lower respiratory tract – 2 children, foreign body endogenous in the trachea in 1 child, compression of the main bronchus in 1 child, and no abnormalities in a child with cyanotic congenital heart disease). Five children (1.7%) underwent inferior bronchoscopy. In 20 cases different procedures were performed during bronchoscopy: dilation of laryngeal stenosis – 13, papillomatosis – 3, inserting a laryngeal separator – 2, laser surgery of haemangioma – 1, and removal of foreign body (granulation tissue) from the trachea – 1. After endoscopic examination a decision to perform tracheostomy was taken in 11 children (5%).
Twenty bronchoscopies were performed in 17 children under 1 month of age (4 girls and 13 boys). Eleven patients were hospitalized in the Intensive Care Unit, 4 in the Neonatal Department, 2 in the ENT Department and 1 in the Cardiological Ward. Indications for bronchoscopy in this group of patients included: atelectasis –7 cases, respiratory failure – 5 cases, dyspnoea – 1 case, stridor – 6 cases, and suspicion of tracheal fistula – 1 case. The most frequent recognition was tracheobronchmacia in 9 cases. Laryngomalacia was found in 3 cases, pneumonia in 3 cases and paresis of the vocal cords in 2 case. Laryngeal stenosis was found in 1 case, anomaly of the bronchi in 1, and no abnormalities in 1 case.
SUMMARY
The largest age group in our material was represented by children under 1 year of age. Symptoms of respiratory tract disease occurring in this period of life may lead to suspicion of a congenital anomaly. Bronchoscopy may be an important or decisive factor in a correct diagnosis. The ability to make a direct assessment of structure, patency and status of the lower respiratory tract facilitates final diagnosis. The most frequent indication for bronchoscopy (in 82 cases) was suspicion of a foreign body in the air passages. Rigid bronchoscopy is the main diagnostic and therapeutic method in these cases. Other indications included: dyspnoea, stridor, atelectasis, pneumonia, and respiratory failure. Inflammatory lesions, aspiration of a foreign body, malacia disorders, stenoses and anomalies of the larynx were the most frequent findings during bronchoscopy.
CONCLUSIONS
1. Bronchoscopy is valuable as both a diagnostic and therapeutic method of examining the respiratory tract.
2. The largest age group is represented by children under 1 year of age (43.5%).
3. Suspicion of a foreign body in the air passages was the most common indication for bronchoscopy (28.3%)
4. Bronchoscopies were carried out for urgent indications in 81.0% of cases.
Piśmiennictwo
1. Cotton R.T., Meyer Ch.M.: Practical Pediatric Otolaryngology. Philadelphia 1999. 2. Hoeve L.J., Rombout J.: Pediatric laryngobronchoscopy. 1332 procedures stored in a data base. Int J Pediatr Otorhinolaryngol 1992 Jul; 24(1):73-82. 3. Bush A.: Bronchoscopy in paediatric intensive care. Paediatr Respir Rev 2003 Mar; 4(1):67-73. 4. Lindahl H., Rintala R., Malinen L., et al.: Bronchoscopy during the first month of life. J Pediatr Surg 1992 May; 27(5):548-50. 5. Ungkanont K. et al.: A retrospective analysis of airway endoscopy in patients less than 1-month old. Laryngoscope 1998 Nov; 108(11 Pt 1):1724-8. 6. Puhakka H. et al.: Pediatric bronchoscopy. A report of methodology and results. Clin Pediatr (Phila) 1989 Jun; 28(6):253-7. 7. Doolittle A.M., Mair E.A.:Tracheal bronchus: classification, endoscopic analysis, and airway management. Otolaryngol Head Neck Surg 2002 Mar; 126(3):240-3. 8. Indications for flexible fiberoptic bronchoscopy in pediatric patients. Am J Dis Child 1983 Jun; 137(6):595--7. 9. Finder J.D.: Primary bronchomalacia in infants and children. J Pediatr 1997 Jan; 130(1):59-66. 10. Cohen S. et al.: Use of rigid and flexible bronchoscopy among pediatric otolaryngologists. Arch Otolaryngol Head Neck Surg 2001 May; 127(5):505-9.