© Borgis - New Medicine 3/2003, s. 40-42
Andrzej Walczak1, Janusz Zaslonka1, Alicja Iwaszkiewicz1, Ryszard Jaszewski1, Marzenna Zielinska2, Radoslaw Zwolinski1, Slawomir Jander1, Leszek Markuszewski1, Stanislaw Ostrowski1
The effect of body surface area on the risk of early postoperative death in patients over 65 years who underwent surgical myocardial revascularization
1 Department of Cardiovascular Surgery, Institute of Cardiology, Medical University of Lodz, Poland
Head: prof. Janusz Zaslonka, MD, PhD
2 Department of Cardiology, Institute of Cardiology, Medical University of Lodz, Poland
Head: prof. Halina Bolinska-Soltysiak, MD, PhD
Summary
Background: The aim of the study was to analyze the effect of body surface area (BSA) on the incidence of death in the early postoperative period in a group of patients over 65 years of age who underwent coronary artery by-pass grafting (CABG).
Material and methods: The analysis concerned 276 patients over 65 years of age who underwent CABG between 1999 and 2000. The mean age of the patients was 69.14 ± 3.42 years. The analyzed group consisted of 193 men (69.93%) with a mean age of 68 ± 3.26 years and 83 women (30.07%) with a mean age of 69 ± 3.79. The patients were exposed to many risk factors – 97% of the patients were in the group of moderate or high risk group according to EuroSCORE.
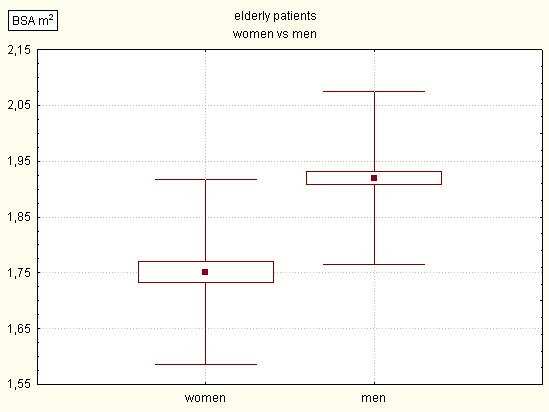
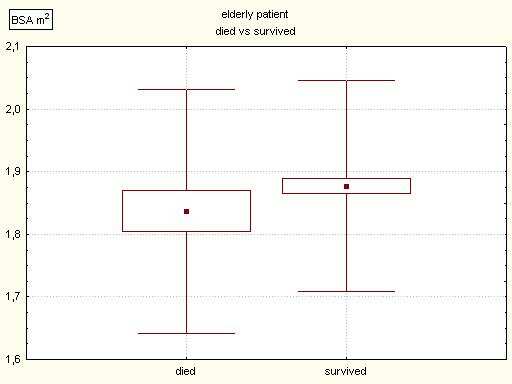
Results: In the study group mean BSA was 1.869 ± 0.176. It was significantly lower in women than in men (1.751 ± 0.166 vs. 1.920 ± 0.154). No statistically significant difference in mean BSA between those who died and those who survived was observed (1.837 ± 0.195 vs. 1.874 ± 0.172, ns). The significant effect of BSA on mortality was found in either the women or men (1.746 ± 0.183 vs. 1.753 ± 0.164 in women and 1.891 ± 0.185 vs. 1.924 ± 0.150 in men).
Conclusions: In the group of elderly patients early postoperative mortality was higher and BSA was lower in women than in men. However, there was no difference in BSA between those who died and those who survived, either in men or in women.
Background
In Cleveland (USA) in 1967, Favoloro performed coronary artery by-pass grafting (CABG) for the first time. In Poland CABG was done for the first time by Moll, in the Department of Cardiac Surgery in Lodz, in 1970. Currently, CABG procedures are the most frequently performed cardiac operations. In Poland in 2002, there were over 13 000 such operations. The age of patients undergoing CABG is increasing because of the increasing prevalence of ischaemic heart disease in an older age population. Many authors emphasize a poorer early outcome of CABG in women, suggesting that this may result from smaller body diameters and in consequence a smaller size of coronary vessels. In our study, we decided to analyze the effect of body surface area (BSA) on early mortality in patients over 65 who underwent myocardial revascularization under cardiopulmonary by-pass (CPB).
Material and methods
A group of 276 patients, aged 65 or older, were operated on due to coronary artery disease, in the Department of Cardiac Surgery, Institute of Cardiology, Medical University of Lodz, between 1999 and 2000. The patients´ mean age was 69.14 ± 3.14 years. The group consisted of 193 men (69.93%) with a mean age of 68 ±3.26 years and 83 women (30.07%) with a mean age of 69 ±3.79.
All CABG procedures were performed through median sternotomy, under CPB with typical cannulation of the ascending aorta and right atrium. St. Thomas Hospital cold crystalloid cardioplegic solution was used as myocardial protection. The left internal thoracic artery was used as a routine graft to the left anterior descending artery, where necessary.
In the analyzed group, 73.55% of patients were in the III or IV functional class of the Canadian Cardiovascular Society (CCS). The patients were also exposed to many risk factors – 97% of the operated patients were in the group of moderate or high risk group according to the EuroSCORE classification.
Body surface area, which is a derivative of a patient´s height and weight, is calculated by the following formula:
BSA = 7.184 x 10-3 x m 0.425 x h 0.725
BSA – body surface area in square metres, m – body weight in kilograms, h – body height in metres.
A death was considered as „early” when it occurred during the operation or within the first 30 postoperative days.
The distribution of normality was assessed using the Shapiro-Wilk normality test W. The statistical assessment of differences between mean values in two groups was made using test Student´s T-test. The analysis of dependence was performed using the chi-squared test.
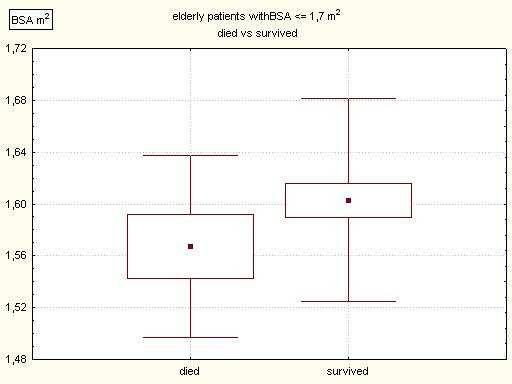
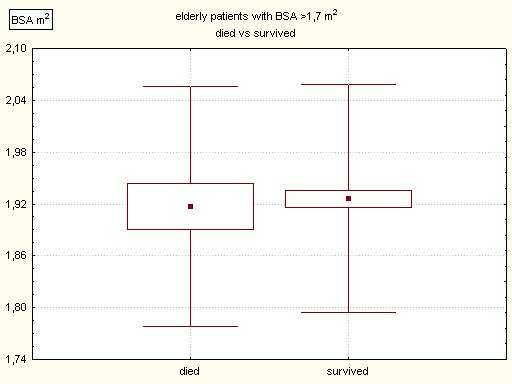
Results: In the analyzed group of 276 patients, aged 65 or older, mean BSA was 1.869 ± 0.176 m2. In the subgroup of women BSA was significantly lower, at 1.751 ± 0.166 m2, p <000.1; (Fig. 1). In those up to 1.7 m2 BSA, there were 39% of women and 7% of men. In the study group there were 35 early deaths (12.68%). The BSA of the patients who died in the early postoperative period was 1.837 ± 0.195 m2 and did not differ significantly from the BSA of the survivors – 1.874 ± 0.172 m2 (Fig. 2). Analyzing the subset of patients with the lowest BSA (up to 1.7 m2), we observed a higher mortality rate than in the total group (18.19%). Also, we found that the survivors had a lower BSA than those who died (1.567 ± 0.070 m2 vs. 1.603 ± 0.079 m2). However, the above-mentioned differences were not statistically significant (Fig. 3). In the subset of patients with BSA higher than 1.7 m2 the mortality rate was 12.5%, and there was no difference in BSA between those who died and the survivors (1.917 ± 0.139 m2 vs. 1.926 ± 0.132 m2, Fig. 4). In the subgroup of women there were 13 early deaths (15.66%). The BSA of women who died was 1.746 ± 0.183 m2 and did not differ from the BSA of women who survived – 1.753 ± 0.164 m2. In the subgroup of men there were 22 early deaths (11.4%) and the effect of BSA on early mortality was not significant (BSA of the dead: 1.891 ± 0.185 m2 vs. BSA of the survivors: 1.924 ± 0.150 m2, ns).
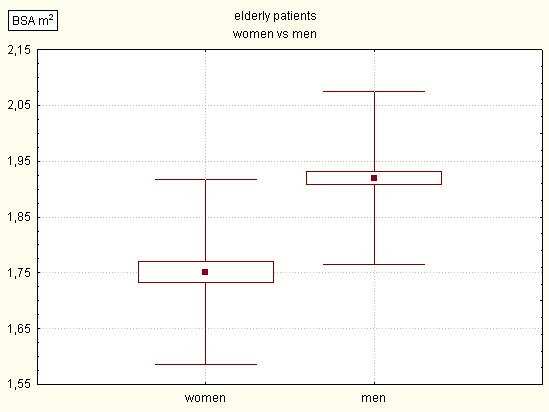
Fig. 1. Comparison of body surface area (BSA) in elderly patients with coronary artery bypass grafting – women vs men (p= 0.00).
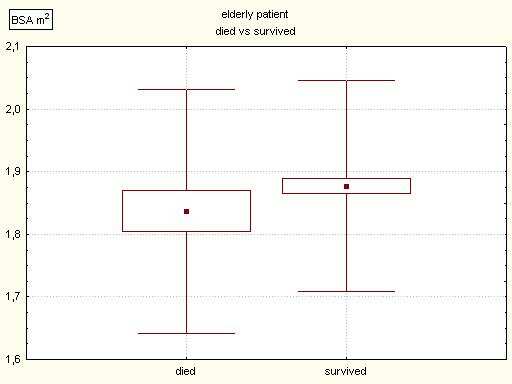
Fig. 2. Comparison of body surface area (BSA) in elderly patients with coronary artery bypass grafting – died vs survived (NS).
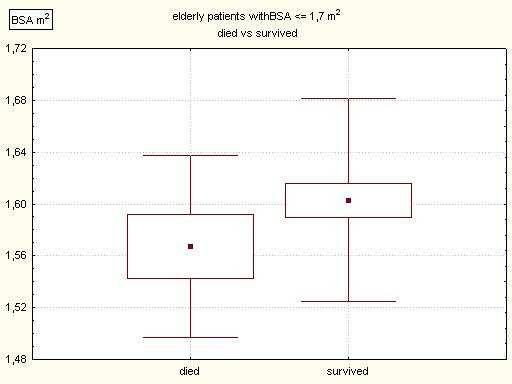
Fig. 3. Comparison of body surface area (BSA) in elderly patients with BSA > 1.7 m2 with coronary artery bypass grafting – died vs survived (NS).
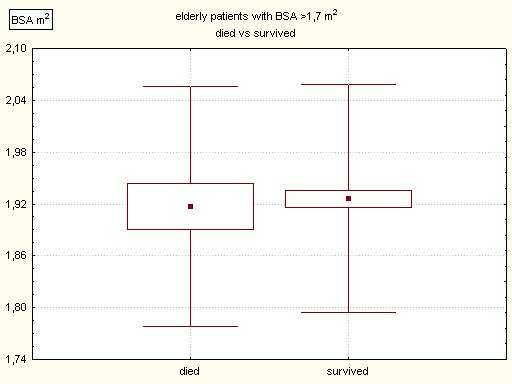
Fig. 4. Comparison of body surface area (BSA) in elderly patients with BSA> 1.7 m2 with coronary artery bypass grafting – died vs survived (NS).
Discussion
In the world, especially in the developed countries, the number of elderly continues to increase. On the other hand, the prevalence of ischaemic heart disease rises with age. Data from the National Database for Adult Cardiac Surgery – Society of Thoracic Surgeons (STS), concerning USA and Canada, showed a constant increase of age in patients undergoing myocardial revascularization procedures and an increase in the number of procedures. In 1990 the mean age of all patients undergoing coronary surgery was 63.7 years, and by 1999 it had risen to 65.1 years (1). In Poland a similar phenomenon can be observed. Between 1995 and 2000 the number of operations performed under cardiopulmonary by-pass doubled, and the percentage of patients over 65 increased from 16% to 25%. In that period, surgical myocardial revascularization was the most frequently performed procedure (79%) in elderly cardiac patients (2). The analyzed group makes up 25% of all patients who underwent a CABG procedure between 1999 and 2000, in our centre. The mean age of all patients who were operated on due to ischaemic heart disease in this period was 58 ± 9.15 years. The influence of risk factors on the outcome of CABG has been assessed many times. In a multicentre Coronary Artery Surgery Study (CASS) it was found that perioperative mortality rose along with a decrease in patients´ body mass and size of coronary arteries. This relationship concerned both men and women, but in the latter it was much more significant (3). Similar conclusions were drawn by O´Connor et al., who found an inverse relationship between body size, vessel diameter, and mortality rate (4). However, Edwards et al. (5) and Mickleborough et al. (6) did not share this opinion and they did not regard the smaller diameter of arteries as a factor increasing operative risk. Analyzing a group of women under 45 who underwent CABG, Zwolinski et al. observed a significant difference in BSA between the patients who died and the survivors (7). The differences in assessment of the effect of BSA on CABG outcome made us decide to examine this problem. We decided to assess the effect of this parameter on mortality rate in a group of patients over 65. In our group, the women had a significantly lower BSA than the men (1.751 ± 0.166 m2 vs. 1.920 ± 0.154 m2, p <0.001). The higher mortality rate in the women was not statistically significant. Similarly, the higher mortality rate in the subset of patients with BSA up to 1.7 m2 also did not reach a level of significance. We did not observe significant differences in BSA, either in the men or in the women, between those who died and those who survived. The high mortality rate in our material resulted from the fact that we assessed the patients with a mean age over 69 years with multiple risk factors – as many as 97% of them were in the moderate or high risk group according to the EuroSCORE classification. In a high risk EuroSCORE group, predicted mortality rate is about 11% (8). Predicted mortality rate in the fifth (the highest) risk group according to the STS classification exceeds 13% (9). In the classification of Higgins from the Cleveland Clinic Foundation, the predicted mortality rate in the highest risk group is over 26% (10). For comparison, in the analyzed period, the mean mortality rate in our centre was below 5%. The mortality rate in elderly patients is comparable with outcomes of high operative risk groups presented in commonly-accepted classifications, but is higher than in the total operated population. The elderly with multiple comorbidities and risk factors remain a great challenge for the whole team – the surgeons, the cardiologists and the anaesthesiologists. We must not forget that this group of patients is going to be bigger and bigger, considering the continually-increasing duration of human life.
Conclusions
In the assessed group of elderly patients who underwent surgical myocardial revascularization early postoperative mortality was higher (not significantly) and BSA was lower (significantly) in the women than in the men. No significant effect of BSA on early mortality was observed in either the women or in the men.
Piśmiennictwo
1. Ferguson T.B., Jr. et al.: A decade of change-risk profiles and outcomes for isolated coronary artery bypass grafting procedures, 1990-1999: a report from the STS National Database Committee and the Duke Clinical Research Institute. Society of Thoracic Surgeons. Ann. Thorac. Surg. 2002; 73:480-489. 2. Zaslonka J. i wsp.: Operacje kardiochirurgiczne u chorych powyżej 65 roku życia w Polsce. Polski Przegląd Kardiologiczny 2001; 3:211-218. 3. Fisher L.D. et al.: Association of sex, physical size, and operative mortality after coronary artery bypass in the Coronary Artery Surgery Study (CASS). J. Thorac. Cardiovasc. Surg. 1982; 84:334-341. 4. O´Connor N.J. et al.: Effect of coronary artery diameter in patients undergoing coronary bypass surgery. Northern New England Cardiovascular Disease Study Group. Circulation 1996; 93:652-655. 5. Edwards F.H. et al.: Impact of gender on coronary bypass operative mortality. Ann. Thorac. Surg. 1998; 66:125-131. 6. Mickleborough L.L. et al.: Is sex a factor in determining operative risk for aortocoronary bypass graft surgery? Circulation 1995; 92:II80-II84. 7. Zwolinski R. i wsp.: Obraz kliniczny i powikłania oko-ooperacyjne u chorych poddanych chirurgicznej rewaskularyzacji mięśnia sercowego do 45 roku życia. Polski Przegląd Kardiologiczny 2002; 4:349-354. 8. Nashef S.A.M. et al.: European system for cardiac operative risk evaluation (EuroSCORE). Eur. J. Cardiothorac. Surg. 1999; 16:9-13. 9. Haan C.K. et al.: Comparison of risk profiles and outcomes in women versus men ? 75 years of age undergoing coronary artery bypass grafting. Am. J. Cardiol. 2003; 91:1255-1258. 10. Higgins T.L. et al.: Stratification of morbidity and mortality outcome by preoperative risk factors in coronary artery bypass patients. A clinical severity score. JAMA 1992; 267:2344-2348.