© Borgis - New Medicine 4/2003, s. 108-111
Barbara Gryglewska, Tomasz Grodzicki
Betaxolol in elderly patients in primary care
Department of Internal Medicine and Gerontology Collegium Medicum Jagiellonian University,
Cracow, Poland
Head of Department: Tomasz Grodzicki MD, PhD
Summary
The object of the study was to evaluate the effectiveness and tolerance of betaxolol in elderly patients with hypertension (HT) and/or coronary heart disease (CHD) in primary care.
Material and methods: An open study was carried out in general practice. Treatment using betaxolol (Lokren, Sanofi-Synthelabo) was given in a dose of 10-40 mg daily to patients with CHD and HT, not taking b-blockers and without contraindications. The treatment was continued over 8 weeks. At the beginning and end of the study, measurements of blood pressure, heart rate, and weight were performed in addition to a questionnaire related to the history of HT and CHD, medicines, concomitant diseases and risk factors of CV diseases. Effectiveness and tolerance were assessed by the physician (using a 4-point scale) and the patient (3-point scale).
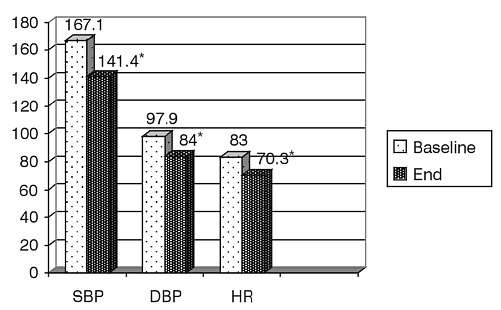
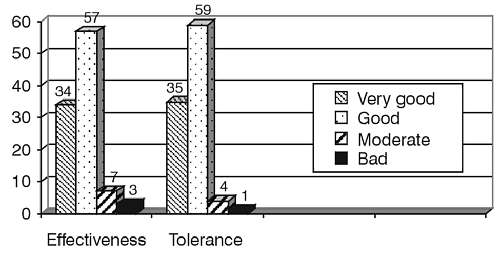
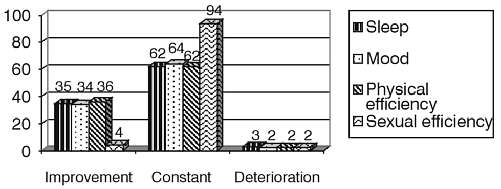
Results: A total of 2839 patients (42%M) aged between 60 – 93 years (mean 68±5.8) were enrolled. Blood pressure values at entry were 167.1±18.6/97.9±10.2 mmHg and heart rate was 83±10.5 beats/min. Almost all subjects (97%) suffered from hypertension, and 67% of them were diagnosed as having CHD (22% after myocardial infarction). Other complications of hypertension are retinopathy (49%) or left ventricular hypertrophy confirmed by electrocardiography or echocardiography (65%). Concomitant diabetes was diagnosed in 22% studied. Family history of hypertension was confirmed in 59% subjects. Betaxolol was mainly used at a dose of 20 mg (63%) or 10mg (36%) daily. The drug was most often added to antihypertensive (91%), lipid-lowering (50%), and anti-platelet (51%) treatment. Treatment led to a significant drop in blood pressure from 167.1±18.6/97.9±10.2 to 141.4±13.7/84±8.3 mmHg, accompanied by a reduction in heart rate from 83±10.5 beats/min. to 70.3±8.4ud/min. at good (59%) or very good (35%) tolerance and effectiveness (good – 57%; very good – 34 %). Only 3% of the studied patients did not reach normal values of systolic blood pressure, and 12% of diastolic blood pressure. Side effects occurred only in 7% of the patients (mainly bradycardia <50 beats/min – 1.5%, headaches and dizziness – 1.2%, weakness – 0.7%. Health condition improved in in the opinion of the majority of patient (74%). Treated subjects did not report any deterioration of sleep quality (no change – 62%, improvement – 35%), mood (no change – 64%, improvement – 34%), physical efficacy (no-change – 62%, improvement – 36%) or sexual performance (94%).
Conclusions: Betaxolol is a safe and effective medication in the treatment of elderly patients with hypertension and coronary heart disease in primary care.
INTRODUCTION
Cardiovascular drugs are the most frequently-prescribed drugs for the elderly (1). But there is very little clinical data on the effects of medications in the elderly, due to a poor representation of the real geriatric population in clinical trials (1). Most drug prescription information for the elderly is extrapolated from younger patients, and there is evidence of underutilization of effective cardiovascular medications in the elderly patients. Moreover, optimal medication prescribing for older people is especially daunting, because they require complex regimens for multiple chronic conditions (2). Additionally, to minimise adverse drug reactions, practitioners must consider age-related changes in drug pharmacokinetics and pharmacodynamics, when selecting from the thousands of chemical entities available (3).
Beta-blockading is one of the most permissible forms of therapy for hypertension (HT) and preferred treatment in patients with coronary heart disease (CHD), (4, 5, 6). However, there are observed differences between guidelines in use beta- blockers among older patients with these diseases, the differences being said to have great prognostic importance in the elderly (1, 7). Although desensitisation, and a decrease in the number of beta-adrenergic receptors are observed and decreased responses to beta-blockers are seen with ageing, beta –blockers are effective to reduce mortality and morbidity either in younger or in older patients with CHD or HT (8, 9). A decreased response to beta blockade is seen predominantly in their action to the contractility, heart rate, and to a lesser extent on peripheral vasodilatation (9). The beta-blockers, especially non-selective beta-blockers, are contraindicated in patients with asthma or moderate-to severe bronchospastic disease (10). They may also affect the sleep pattern and worsen depression and sometimes, if left ventricular dysfunction is present, they can cause decompensation. So beta-blockers are not a good choice of therapy for some elderly patients suffering from chronic diseases.
Betaxolol is one of the newer cardioselective beta-adrenoreceptor antagonists with a long half-life, 16-22 hrs, making it suitable for once-a-day administration (11). It has been shown that betaxolol is effective in the treatment of hypertension and stable angina pectoris in comparison to other beta-blockers (10). Batoxolol is widely used in the treatment of glaucoma in the elderly, but its safety and efficiently in older patients with HT and CHD are limited (12, 13). The objective of the study was to evaluate the effectiveness of, and tolerance to betaxolol in therapy on patients over 59 years old with hypertension and/or coronary heart disease in primary care.
MATERIALS AND METHODS
This study is a part of wider research, which is in press. All patients agreed orally to participate to the study. The study was conducted at primary care. Patients over 59 years old not receiving a beta-blocker were enrolled in an open-label clinical trial. Treatment with betaxolol (Lokren, Sanofi-Synthelabo) was given at a dose of 10-40 mg daily to patients with CHD and/or HT without contraindications. Remaining antihypertensive or antianginal therapy was not modified during the study.
The treatment continued for 8 weeks. At the beginning and end of the study measurements of blood pressure and heart rate were made in twice addition to a questionnaire related to the history of HT and CHD, medication, and any concomitant diseases. The effectiveness of betaxolol was analysed by changes in systolic blood pressure and heart rate from baseline values, and by the physician´s assessment as very good, good, moderate or bad. Tolerance of the drug was also assessed by the physician (using a 4-point scale) and the patient (3-point scale). The subjective opinions of the patients related to their estimates of the quality of sleep, mood, and physical and sexual efficiency were gathered. All complaints related to side effects of the drug were noted.
All data are expressed as mean ±SD. Comparisons between data at the beginning and the end of the study were done by Student´s T-test for paired data. For all tests, p values?>?0.05 were considered statistically significant.
RESULTS
A total of 2839 patients (42%M) aged between 60-93 years (mean 68±5.8) were enrolled (Table 1). Almost all subjects (97%) suffered from hypertension, and 67% of them from CHD (22% after myocardial infarction). Other complications of hypertension were retinopathy (49%), and left ventricular hypertrophy confirmed by electrocardiography or echocardiography (65%). Concomitant diabetes was present in 22% of the subjects. A family history of hypertension was confirmed in 59%. Betaxolol was mainly used at a dose of 20 mg (63%) or 10 mg (36%) daily. The drug was most often added to antihypertensive (91%), lipid-lowering (50%), or anti-platelet (51%) treatment (Table 2).
Blood pressure values at entry were 167.1±18.6/97.9±10,2 mmHg and heart rate 83±10.5 beats/min. Treatment led to a significant drop in blood pressure, to 141.4±13.7/84±8.3 mmHg and a reduction in heart rate to 70.3±8.4 beats/min (Figure 1). Only 3% of patients did not reach normal values of systolic blood pressure, and 12% did not reach normal diastolic blood pressure. Tolerance and effectiveness assessed by the physician was good or very good (Figure 2). Side effects occurred only in 7% of the patients (mainly bradycardia <50 beats/min – 1.5%, headaches and dizziness – 1.2%, weakness – 0.7%), (Table 3). It is interesting that an excessive fall in blood pressure was observed only sporadically in the elderly subjects. The condition of health improved in the majority of patients´ opinion´s (74%). The subjects did not report sleep deterioration nor negative effects on mood qualities, physical efficiency or sexual performance (Figure 3).
DISCUSSION
Table 1. Characteristics of 2839 studied patients.
| Parameter | Initial data
(Mean values ? SD) |
| Age (years) | 68 ? 5.8 |
| Male (%) | 42 |
| SBP (mmHg) | 167 ? 18.6 |
| DBP (mmHg) | 97.9 ? 10.2 |
| HR (beats/min) | 83 ?10.5 |
| Patients with HT and CHD (%) | 66 |
SBP – systolic blood pressure, DBP – diastolic blood pressure, HR – heart rate, HT – hypertension, CHD – coronary artery disease
Table 2. Concomitant treatments.
| Class of drugs | Prevalence (%) |
| Diuretics | 58 |
| ACE-I | 68 |
| Calcium channel blockers | 25 |
| Antiarrhythmic | 7 |
| Lipid-lowering | 50 |
| Antidiabetic | 19 |
| Antiplatelet | 51 |
| Hypnotic | 18 |
ACE-I – angiotensin-converting enzyme inhibitors
Table 3. Prevalence of side effects during betaxolol treatment.
| Side effect | Prevalence (%) |
| Bradycardia | 1.5 |
| Headaches and dizziness | 1.2 |
| Weakness | 0.7 |
| Sleeping disorders | 0.4 |
| Dyspeptic symptoms | 0.3 |
| Excessive fall of blood pressure | 0.07 |
| Problems with erection | 0.1 |
| Dyspnoea | 0.2 |
| Other | 2.53 |
Fig. 1. Effects of betaxolol on blood pressure (mmHg) and heart rate (beats/min.).
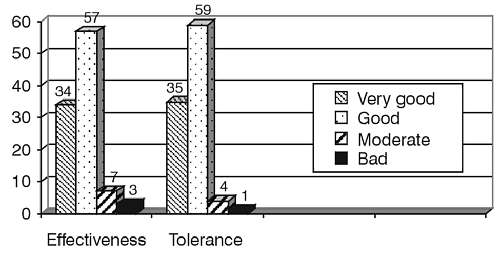
Fig. 2. Effectiveness and tolerance of betaxolol therapy assessed by the physician using a 4-point scale.
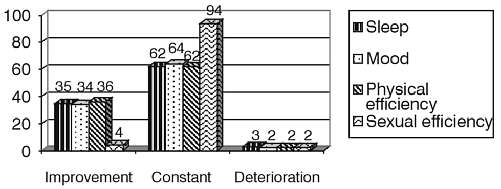
Fig. 3. Patient´s estimaties of sleep, mood quality and physical and sexual efficiency.
Betaxolol, a long-acting cardioselective beta-blocker, was effective and very well tolerated in elderly patients with hypertension and coronary heart disease treated in primary care. This is shown in the objective parameters (blood pressure, heart rate, side effects) and unonymous subjective opinions of both physicians and patients.
Betaxolol is used as a topical antiglaucoma drug (12). Many antiglaucoma medications, when systemically absorbed, can cause adverse effects, especially in elderly people, who are most prone to chronic eye disease. However, betaxolol appears to be an effective and well-tolerated ocular hypotensive agent in a typical glaucoma population (12). Moreover, betaxolol treatment is associated with a beneficial effect on retinal artery width, whereas timolol does not yield the same size of benefit (14). The pharmacological properties and the therapeutic efficiency of betaxolol in the treatment of mild-moderate hypertension have been demonstrated (11). It reduces myocardial oxygen demand in patients with hypertension, angina, and cardiac ischaemia, and appears to be very useful as a once daily treatment for angina (15). The high beta 1-selectivity of betaxolol explains its good tolerability with respect to lung function and lipid profile (11). Although its safety and efficacy has been demonstrated in younger patients, studies in older patients with HT and CHD, except with glaucoma, are limited. A study in a small group of elderly patients with hypertension showed that betaxolol produced a significant reduction in systolic and diastolic pressure, thickness of the posterior wall of the left ventricular myocardium, ejection fraction, and total peripheral vascular resistance without significant side effects or a rise in the levels of cholesterol, beta-lipoproteins, triglycerides, or glucose (13). Our study confirmed the safety and good tolerance of betaxolol in a larger group of elderly patients with HT and CHD.
In the studied patients betaxolol was used mostly as a concomitant therapy. It is a typical observation that up to 80% of the elderly, suffer from chronic diseases, and need polypharmacy (1). Unfortunately, this may lead to increase a risk of interactions, adverse effects, and toxic reactions. Moreover, age-related changes in drug pharmacokinetics and pharmacodynamics are connected with the need to increase drug levels for a longer time, and thus increasing any drug side effects (3). The presented data shows that the use of betaxolol in association therapy was safe and well-tolerated. The most frequent side effect was bradycardia an effect which depends on the negative chronotropic properties of all beta-blockers. It is interesting that an excessive fall of blood pressure was observed only sporadically in the studied elderly subjects. Autonomic control of blood pressure appears to decline with age, giving an increased risk of orthostatic hypotension and major hypotensive reactions to antihypertensive drugs (16). In various populations with increased sympathetic activity, beta-blockers have been demonstrated to cause pressor effects, presumably due to alfa-adrenoceptor-mediated vasoconstriction unopposed by beta-receptor-mediated vasodilatation. This phenomenon cannot be demonstrated with non-beta-blocker antihypertensive drugs, including ACE inhibitors, calcium channel antagonists, diuretics and angiotensin II receptor antagonists (16). In elderly patients beta-blockers may, therefore, be the most appropriate antihypertensive agents, as they protect the elderly from orthostatic impairment. The elimination half-life of betaxolol, longer than most beta-blockers, decreases the risk of a rebound phenomenon after stopping beta-blockers in which if a patient has CHD there is an increased incidence of myocardial ischaemic events, including death (10, 11). The use of beta-blockers in heart failure for a long time was regarded as contra-indicated because of their negative inotropic effects. Nevertheless, there is growing evidence that beta-blockers have a predictive value for survival (17). In the studied population only a few subjects complaint of dyspnoea. The presumed benefit of a beta-blockade with betaxolol in chronic heart failure is assessed in the BETACAR trial, a comparative study versus carvedilol (18).
It has been noted in the past that the response in the elderly is less favourable from a non-selective beta blockade, than from a diuretic, and similar from diuretics and beta 1-seletive beta-blocking drugs (10). Although in the elderly diuretics may be superior to beta-blockers as primary prevention in hypertension for both coronary events and cardiovascular disease (19), it is evident that in patients with coexistent coronary artery disease there was a reduction in the risk of death and cardiovascular events (4). Moreover, a lack of the beta-blockers in the treatment was associated with poor blood pressure control, and that effect was independent of age (20).
In conclusion, this study has demonstrated that betaxolol given in a single daily dose is effective, safe and well-tolerated in the treatment of elderly patients with hypertension and coronary heart disease in primary care, even in combination therapy.
Piśmiennictwo
1. Raza J.A., Movahed A.: Use of cardiovascular medications in the elderly. Int. J. Cardiol. 2002; 85: 203-9. 2. Anderson G., Kerluke K.: Distribution of prescription drugs exposure in the elderly: description and implications. J. Clin. Epidemiol. 1996; 49:929-936. 3. Podrazik P.M., Schwartz J.B.: Cardiovascular disease in the elderly. Cardiovascular pharmacology of ageing. Cardiol. Clin. 1999; 17:1-34. 4. Gibbons R.J. et al.: ACC/AHA 2002 guideline update for the management of patients with chronic stable angina-summary article: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on the Management of Patients With Chronic Stable Angina). J. Am. Coll. Cardiol. 2003; 41:159-68. 5. World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. J. Hypertens. 1999, 17:151-183. 6. Stanowisko Polskiego Towarzystwa Nadciśnienia Tętniczego: Zasady postępowania w nadciśnieniu tętniczym. Nadc. Tętn. 2000; 4:B1-B34. 7. Juliard J.M. et al.: Age and lack of beta-blocker therapy are associated with increased long-term mortality after primary coronary angioplasty for acute myocardial infarction. Int. J. Cardiol. 2003; 88(1):63-8. 8. Hanlon J.T. et al.: Suboptimal prescribing in older inpatients and outpatients. J. Am. Geriatr. Soc. 2001; 49:200-5. 9. Lakatta E.G.: Cardiovascular regulatory mechanisms in advanced age. Physiol. Rev. 1993; 73:413-467. 10. Prichard B.N.C., Cruickshank J.M.: Beta blockade in hypertension. In: Mancia G. et al. editors. Manual of Hypertension. London: Churchill Livingstone, 2002; p. 318-335. 11. Beresford R., Heel R.C.: Betaxolol: A review of its pharmacodynamic and pharmacokinetic properties and therapeutic efficacy in hypertension. Drugs 1986; 31:6-28. 12. Goldberg I., Goldberg H.: Betaxolol eye drops. A clinical trial of safety and efficacy. Aust. N Z J. Ophthalmol. 1995; 23(1):17-24. 13. Lazebnik L.B. et al.: [Pharmacodynamic effects of lokren (betaxolol) in 3 month treatment of blood hypertension in elderly patients] (Russian) Ter. Arkh. 1998; 70(6):44-7. (abstr.). 14. Collignon N.J., Collignon-Brach J.D.: Effect of topical beta-blockers on human retinal vessel diameters. Int Ophthalmol. 1997-98; 21(4): 199-203. 15. Chrysant S.G., Bittar N.: Betaxolol in the treatment of stable angina pectoris. Cardiology 1994; 84:316-21. 16. Cleophas T.J., van Marum R.: Age-Related Decline in Autonomic Control of Blood Pressure: Implications for the Pharmacological Management of Hypertension in the Elderly-Drugs Ageing. 2003; 20 (5): 313-319. 17. Cas L.D. et al.: Prevention and Management of Chronic Heart Failure in Patients at Risk. Am. J. Cardiol. 2003; 91(suppl.): 10F-17F. 18. Bohler S. et al.: Betaxolol versus carvedilol in chronic heart failure (BETACAR study). Rationale and design. Arzneimittelforschung. 1999; 49(4):311-7. 19. Messerli F.H. et al.: Are beta-blockers efficacious as first-line therapy for hypertension in the elderly? A systematic review. JAMA 1998; 279:1903-1907. 20. Grodzicki T. et al.: Risk of uncontrolled hypertension according to current treatment regimen. XIII Europ. Meeting, Mediolan 2003 (abstr.).