*Ewa Krasuska-Sławińska1, Dariusz Polnik2, Dorota Olczak-Kowalczyk3, Tomasz Dzik4, Katarzyna Świstak1
Congenital granular cell tumour – two case reports
Wrodzony guz ziarnistokomórkowy – opis dwóch przypadków
1Dental Surgery Clinic, The Children’s Memorial Health Institute
Head of Clinic: Agnieszka Pieniak, MSc
2Department of Paediatric Surgery and Organ Transplantation, The Children’s Memorial Health Institute
Head of Department: Professor Piotr Kaliciński, MD, PhD
3Department of Paediatric Dentistry, Medical University of Warsaw
Head of Department: Professor Dorota Olczak-Kowalczyk, MD, PhD
4Department of Pathology, The Children’s Memorial Health Institute
Head of Department: Associate Professor Maciej Pronicki, MD, PhD
Streszczenie
Wrodzony guz ziarnistokomórkowy jest to rzadko występująca zmiana o łagodnym charakterze, najczęściej pojedyncza, uszypułowana, wyrastająca z przedniej części wyrostka zębodołowego szczęki, rzadziej części zębodołowej żuchwy. Guzy o znacznych rozmiarach mogą utrudniać odżywianie i oddychanie, dlatego wymagają interwencji chirurgicznej, polegającej na ich usunięciu. W przypadku zmian o niewielkich rozmiarach możliwa jest spontaniczna regresja.
Celem pracy jest przedstawienie dwóch pacjentek, u których bezpośrednio po urodzeniu stwierdzono obecność uszypułowanych guzów w jamie ustnej.
Dwa noworodki płci żeńskiej, leczone w Klinice Chirurgii Dziecięcej i Transplantacji Narządów IP-CZD z powodu guzów w obrębie wyrostka zębodołowego szczęki/części zębodołowej żuchwy zdiagnozowanych bezpośrednio po urodzeniu, niewidocznych w badaniach USG wykonywanych w czasie ciąży. Obydwa guzy o średnicy około 1,5 cm łatwo ulegały urazom podczas ssania, powodując krwawienie, dlatego podjęto decyzję o ich chirurgicznym usunięciu. W materiale histopatologicznym uzyskano obraz wrodzonego guza ziarnistokomórkowego noworodków. Badanie kontrolne obu pacjentek po 6 miesiącach wykazało prawidłową budowę wyrostka zębodołowego szczęki/części zębodołowej żuchwy.
W przypadku guzów ziarnistokomórkowych o dużych rozmiarach leczeniem z wyboru jest leczenie chirurgiczne. Guz nie powoduje zmian w budowie wyrostka zębodołowego szczęki/części zębodołowej żuchwy.
Summary
Congenital granular cell tumour is a rare, usually single, pedunculated benign lesion, originating from the anterior part of the maxillary alveolar process, less frequently from the alveolar part of the mandible. Large tumours can cause problems in eating and breathing, therefore require surgical intervention involving excision. Smaller lesions can resolve spontaneously.
The aim of the study was to present 2 case reports of patients with pedunculated oral tumours diagnosed immediately after birth.
Two female newborns treated at the Department of Paediatric Surgery and Organ Transplantation (CMHI) due to tumours located within the maxillary alveolar process/alveolar part of the mandible, which were diagnosed immediately after birth, but were not visualised during prenatal ultrasound. Both tumours with a diameter of about 1.5 cm were easily damaged during sucking, causing bleeding. Therefore a decision was made to perform their surgical removal. Histopathological examination revealed congenital granular cell tumour of the newborn. A follow up after 6 months showed normal structure of the maxillary alveolar bone/alveolar part of the mandible.
Surgery is the treatment of choice in patients with large granular cell tumours. The tumour does not cause changes in the structure of the alveolar process/the alveolar part of the mandible.

Introduction
Congenital granular cell tumour was for the first time described by Neuman in 1871 as a rare benign lesion of unknown aetiology, eight times more common in female compared to male newborns (1). Clinically, it appears as a single pedunculated tumour originating from the anterior part of the maxillary alveolar process, mostly from the gingival papilla, less often from the alveolar part of the mandible. Large tumours can cause problems in eating and breathing, therefore require surgical intervention involving their excision. Smaller lesions can resolve spontaneously. Histologically, congenital granular cell tumour is identical to granular cell tumour, also known as Abrikosoff’s tumour, which typically occurs in adults, mostly on the tongue. Their differentiation is based on immunohistochemistry and electron microscopy. Differential diagnostics should also include neuroectodermal tumors, hemangiomas, teratomas, fibromas, rhabdomyomas, odontogenic tumours, dermoid cysts (1, 2).
Case reports
Case 1
A 3-day-old female newborn was admitted to the Department of Paediatric Surgery and Organ Transplantation (CMHI) due to an exophytic lesion present in the anterior part of the maxillary alveolar process. The girl was born from the first pregnancy, first delivery by Caesarean section due to lack of progress in labour at 39 weeks gestation, in overall good condition (Apgar score of 10). Medical history of normal course of pregnancy, maternal group B streptococcal (GBS) genital tract colonisation managed with antibiotic prophylaxis.
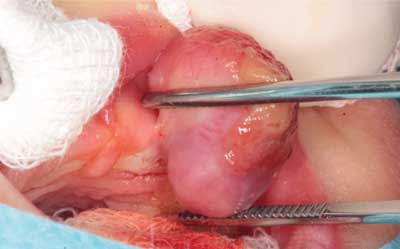
Physical examination of the oral cavity revealed an exophytic tumour with a broad pedicle in the anterior part of the maxillary alveolar process (fig. 1). The lesion measuring 1.5 x 1.5 x 2 cm did not prevent sucking or breathing, however, it was easily damaged causing bleeding when sucking. Other than that, normal pink smooth and shiny oral mucosa without pathological lesions. Blood tests (blood count, coagulation parameters, ionogram, blood type), abdominal and CNS ultrasound revealed no abnormalities.
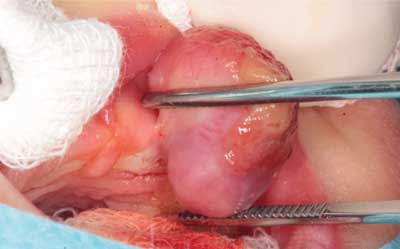
Fig. 1. Case 1. Maxillary alveolar tumour
The entire polypoid tumour of the alveolar soft tissues was removed at 4 hours of life, under general anaesthesia with endotracheal intubation using a bipolar diathermy (fig. 2). The wound was closed with absorbable sutures. The postoperative period was uneventful.

Fig. 2. Case 1. Maxillary alveolar tumour post-excision
Histopathological examination revealed gingival granular cell tumour of the newborn. Immunochemistry was also performed: CD68(+), AE1/AE3(-), CD34(+), S-100(-). The patient has remained under observation at the Surgery Outpatient Clinic for Children and Adults: six months after surgery the child develops normally. Intra- and extraoral clinical examination revealed no abnormalities. Normal vestibular and oral mucosa. Symmetrical maxillary alveolar process with no pathological lesions (fig. 3).

Fig. 3. Case 1. Maxillary alveolar process 6 months after surgery
Case 2
Powyżej zamieściliśmy fragment artykułu, do którego możesz uzyskać pełny dostęp.
Mam kod dostępu
- Aby uzyskać płatny dostęp do pełnej treści powyższego artykułu albo wszystkich artykułów (w zależności od wybranej opcji), należy wprowadzić kod.
- Wprowadzając kod, akceptują Państwo treść Regulaminu oraz potwierdzają zapoznanie się z nim.
- Aby kupić kod proszę skorzystać z jednej z poniższych opcji.
Opcja #1
29 zł
Wybieram
- dostęp do tego artykułu
- dostęp na 7 dni
uzyskany kod musi być wprowadzony na stronie artykułu, do którego został wykupiony
Opcja #2
69 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 30 dni
- najpopularniejsza opcja
Opcja #3
129 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 90 dni
- oszczędzasz 78 zł
Piśmiennictwo
1. Sowa A, Borszewska-Kornacka MK, Małdyk J, Dębska M: Nadziąślak u noworodka z ciąży bliźniaczej – opis przypadku. Ginekol Pol 2013; 84: 733-736. 2. Shaw L, Al-Malt A, Carlan SJ et al.: Congenital epulis. Tree-Dimensional Ultrasonographic Findings and Clinical Implications. J Ultrasound Med 2004; 23: 1121-1124. 3. Bosanquet D, Roblin G: Congenital Epulis: A Case Report and Estimation of Incidence. Int J Otolaryngol 2009; 2009: 508780. 4. Lapid O, Shaco-Levy R, Krieger Y et al.: Congenital Epulis. Pediatrics 2001; 107: 22. 5. Dzieniecka M, Komorowska A, Grzelak-Krzymianowska A, Kulig A: Multiple congenital epuli (congenital granular cell tumors) in the newborn: a case report and review of literature. Pol J Pathol 2011; 1: 69-71. 6. McGuire TP, Gomes PP, Freilich MM, Sandor GKB: Congenital Epulis: A Surprise in the Neonate. J Can Dent Assoc 2006; 72(8): 747-750. 7. Wittebole A, Bayet B, Veyckemans F et al.: Congenital Epulis of the Newborn. Acta chir belg 2003; 103: 235-237. 8. Koch BL, Myer III C, Egelhoff JC: Congenital Epulis. AJNR 1997; 18: 739-741. 9. Silva GCC, Vieira TC, Vieira JC et al.: Congenital granular cell tumor (congenital epulis): A lesion of multidisciplinary interest. Med Oral Patol Oral Cir Bucal 2007 Oct; 12(6): E428-430. 10. Kumar P, Hyon Soo Kim H, Zahtz GD et al.: Obstructive Congenital Epulis: Prenatal Diagnosis and Perinatal Management. Laryngoscope 2002; 112: 1935-1939. 11. Ritwik P, Brannon RB, Musselman RJ: Spontaneous regression of congenital epulis: a case report and review of the literature. Journal of Medical Case Reports 2010; 4: 331. 12. Garg S, Embleton ND, Cole B: Congenital epulis: from birth to childhood. Turk J Pediatr 2014; 57: 97-99. 13. Sakai VT, Oliveira TM, Silva TC et al.: Complete spontaneous regression of congenital epulis in a baby by 8 months of age. International Journal of Paediatric Dentistry 2007; 17: 309-312.