*Monika Jabłońska-Jesionowska, Lidia Zawadzka-Głos
Diagnostic difficulties in determining the cause of congenital respiratory stridor in an infant with multiple congenital abnormalities – a case report
Trudności diagnostyczne w ustaleniu przyczyny wrodzonego stridoru oddechowego u niemowlęcia z licznymi wadami wrodzonymi – opis przypadku
Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Associate Professor Lidia Zawadzka-Głos, MD, PhD
Streszczenie
Termin „stridor oddechowy” odnosi się do przypadków, w których podczas oddychania słychać dodatkowy patologiczny, głośny dźwięk, zawsze świadczy on o zwężeniu światła dróg oddechowych. Patologiczna zmiana powodująca zwężenie może mieć różny charakter i występować na każdym poziomie drogi oddechowej. Może być również zmianą spoza światła dróg oddechowych i poprzez ucisk z zewnątrz powodować problem oddechowy. Diagnostyka stridoru to uzupełniające się metody endoskopowe i obrazowe. Nie ma jednej idealnej metody, która pozwala na postawienie rozpoznania. W naszej pracy chcieliśmy przedstawić trudności diagnostyczne w ustaleniu przyczyny stridoru oddechowego u kilkunastodniowego niemowlęcia płci żeńskiej z licznymi wrodzonymi wadami w obrębie twarzoczaszki, szyi i serca.
Summary
The term respiratory stridor refers to cases in which an additional pathological, loud sound is heard during breathing, and it always indicates narrowing of the lumen of the airways. The pathological change causing airway obstruction can be of various nature and can occur at any level of the airway. It can also be a lesion outside the lumen of the airway and cause a respiratory problem through external pressure. Diagnostics of stridor is based on complementary endoscopic and imaging tests. There is no one perfect method that allows to make a diagnosis. In our study, we wanted to present diagnostic difficulties in determining the cause of respiratory stridor in a several days old female infant with numerous congenital defects in the facial skeleton, neck and heart.
Introduction
Respiratory stridor is an extra sound heard during breathing, which always indicates a narrowing of the airway. Congenital respiratory stridor is associated with congenital defects that obstruct the airway lumen. The most common cause of congenital respiratory stridor is laryngomalacia followed by vocal cord paralysis and congenital cricoid cartilage stenosis. Other common pathologies include cysts, infantile hemangiomas, laryngeal webs at the level of the glottis or in the trachea, anomalies of the great vessels compressing the airways from the outside. Defects can occur at many levels of the respiratory tract at the same time (1-3). The severity of stridor depends on the diameter of the airways. Significant stenosis may require mechanical respiratory support. Each stridor requires diagnostic evaluation, which is based on complementary tests. The basis is a physical examination with a history of the course and duration of pregnancy, type of delivery, and well-being of the newborn assessed with the APGAR scale, which may suggest congenital defects. The history of endotracheal intubation, its duration, technical difficulties or injury during this procedure can also indicate respiratory problems. We should pay attention to baby’s voice and cry. Silent, quiet crying or voice may indicate pathology within the vocal folds. It is important to assess the child’s neurological status. The coexistence of possible cardiovascular pathologies or other congenital anomalies and genetic defects is important (1, 2). Basic tests for respiratory problems include: chest x-ray, blood saturation measurement, echocardiography, fetal brain ultrasound. Complementary endoscopic methods: fiberoscopy and direct laryngotracheoscopy are the basis for lower respiratory tract diagnosis. Fiberoscopy without general anesthesia allows for the evaluation of the larynx to the level of the vocal folds during breathing, phonation, swallowing, which gives the opportunity to assess functional disorders. Direct laryngotracheoscopy under general anesthesia allows for the assessment of all levels of respiratory tract from larynx to the trachea, with the division into the main bronchi. General anesthesia limits the ability to assess the mobility of the vocal folds. The diagnostics are supplemented by: ultrasonography of the larynx with the assessment of mobility the vocal cords, computed tomography and magnetic resonance imaging of the chest and neck with contrast to visualize the eventual pathologies and anatomical relations in the mediastinum (1, 2, 4, 6).
Case report
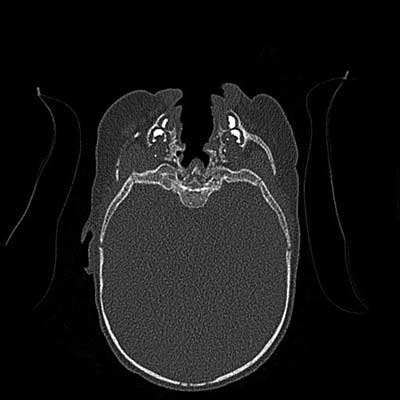
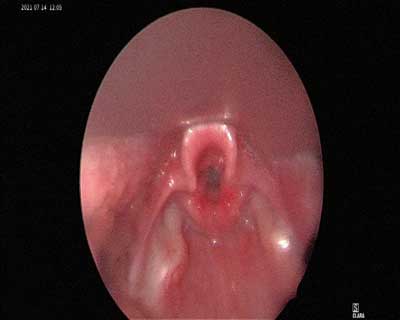
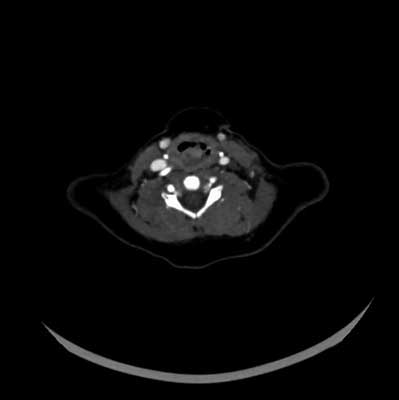
A female infant delivered by caesarean section at 39 weeks gestation was assessed with Apgar score of 7, 9 and 10. The infant’s birth weight was 2820 g, length 54 cm, and head circumference 33 cm. Polyhydramnios was diagnosed during pregnancy. No other diseases and pathologies during pregnancy were found. At birth, the newborn was diagnosed with cleft of the lip and palate, hiatal hernia of the diaphragm, absence of the thymus and ASD heart defect. From the 14th day of life the patient presented with episodic inspiratory stridor and desaturations (down to 70-80%) with an unclear pattern. Stridor appeared irregularly, usually every few days. Cephalic extension positive airway pressure (CEPAP) support was required. Additionally, the patient had difficulties in swallowing related to the cleft palate. The patient had poor weight gain. Further evaluation including chest radiography, laryngotracheal ultrasonography, fetal brain ultrasound (to exclude any pathologies in the central nervous system) shows no additional abnormalities. Due to the cleft lip changes, craniofacial CT was performed, where no other pathologies were found (fig. 1, 2). Subsequently, endoscopic examinations of the airways were performed. Due to the shortness of breath in the child requiring respiratory support, it was decided for first to perform laryngotracheoscopy under short general anesthesia in the endoscopic operating suite. The examination did not reveal any pathologies within the larynx and trachea (fig. 3, 4). The child’s condition remained unchanged, and required ongoing CEPAP support and tube feeding due to episodes of choking that exacerbated respiratory problems. The stridor continued to occur episodically, often in relation to the patient’s anxiety. An upper airway fiberoptic evaluation without sedation was recommended. During such examination, the child is restless, which was intended to induce stridor. The course of the examination was recorded and many times replayed. A periodically appearing abnormality behind the posterior commissure has been observed. This pathological change was likely to be a vascular origin which, filling with its size, closed the entrance to the larynx from the back and causing inspiratory stridor (fig. 5, 6). In the next stage, a craniofacial CT with contrast without sedation was performed in the period of the child’s anxiety – a lesion on the posterior wall of the laryngeal part of the pharynx was visualized. It has been described as a pathological contrast enhancement tissue. The lesion was defined as a fluid space that may correspond to e.g. accumulation of secretions (fig. 7). In addition, the structure of the larynx is correct. Finally, magnetic resonance imaging of the head and neck with contrast was performed under general anesthesia which revealed numerous vascular anomalies in the neck: the tortuous course of the right common and internal carotid artery along its entire length, narrowing of the bone canal of the left common and internal carotid artery in the precranial section and lack of contrast in the intracranial part of this artery (fig. 8, 9). The lesion causing the stridor was identified as a fragment of the right internal carotid artery located posteriorly to the larynx.

Fig. 1. The craniofacial CT – the cleft of lip and palate
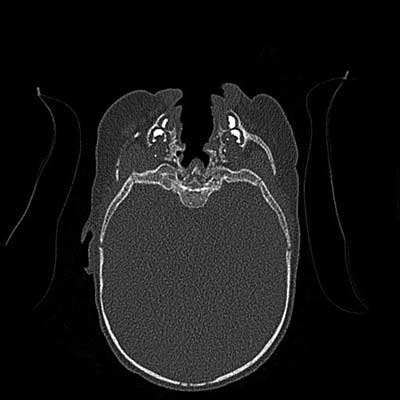
Fig. 2. The craniofacial CT – the cleft of lip and palate
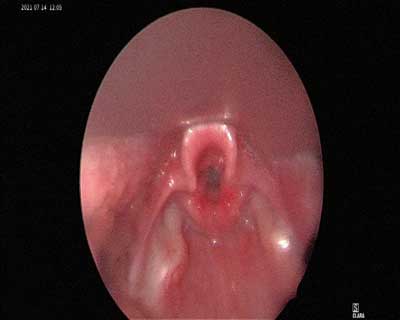
Fig. 3. The entrance to the larynx in laryngotracheoscopy

Fig. 4. The level of trachea in laryngotracheoscopy

Fig. 5. Laryngofiberoscopy – the entrance to the larynx

Fig. 6. Laryngofiberoscopy – moment with the pathological change in the entrance to the larynx
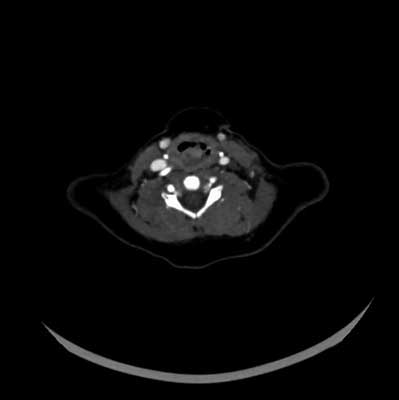
Fig. 7. The craniofacial CT with contrast – a lesion on the posterior wall of the laryngeal part of the pharynx

Fig. 8. Vascular anomalies in MRI 3D reconstructions

Fig. 9. Vascular anomalies in MRI 3D – reconstructions
Discussion
The symptom of airway obstruction is stridor. Congenital defects of the lower respiratory tract account for 0.1-4% of all congenital defects in children. They occur in 5% of newborns. They are the second leading cause of infant mortality after heart defects. Up to the age of 5 50% of children with congenital respiratory disease die. The presence of one defect does not preclude another. Multiple pathologies of the respiratory tract occur in about 50% of children with congenital respiratory stridor. Establishing a diagnosis of what is the cause of stridor often creates a lot of problems, as shown by the example of our patient. Diagnostics involves many complementary tests, often requiring repetition. There is no one perfect test that simultaneously assesses the anatomy and function of all levels of the airway. Endoscopy of the lower respiratory tract, the so-called laryngotracheoscopy under general anesthesia, which allows for the assessment of all levels of the respiratory tract, turned out to be insufficient, the patient did not present any symptoms at rest. The transmitted pulsation, characteristic of the anomalies of the great vessels, causing pressure on the airways from the outside, was not shown. Fiberoscopy performed without general anesthesia made the child anxious and revealed a pathological lesion. Contrast-enhanced computed tomography did not answer the question about the nature of the lesion. Only magnetic resonance imaging with 3D reconstructions confirmed the vascular nature of the lesion. Finally, our patient was diagnosed with anomalies of the great arteries as the cause of respiratory stridor. The most common cause of congenital respiratory stridor in children reported in the literature is laryngeal laxity, followed by vocal fold paralysis and congenital cricoid stenosis (1-3). According to the literature, anomalies of the great arteries are very rare. They account for 0.1% of all congenital heart defects (5-9), no data have been found on the frequency of causes of congenital stridor. On the basis of other studies by the author of this article (10), the analysis of 110 cases of children with congenital stridor showed that anomalies of the great vessels are an underestimated cause of congenital respiratory stridor in children, according to him, they are the second most common cause of stridor. The example of our patient is further evidence of this. We would also like to point out, as our patient’s example showed, that congenital pathologies are numerous, at different levels of the respiratory tract. Endoscopic and imaging diagnostics cannot be limited to selected sections of the lower respiratory tract, but must cover the entirety of the craniofacial, pharynx, larynx, subglottic area and trachea with the division into the main bronchi (11, 12).
Conclusions
1. Diagnosis of congenital respiratory stridor requires many diagnostic methods that complement each other and together lead to the final diagnosis. Endoscopic methods and airway imaging together constitute the diagnostic standard.
2. Anomalies of the great vessels should always be considered as a cause of congenital respiratory stridor, which is a more common cause of this stridor than is believed.
3. The coexistence of numerous congenital defects within the respiratory tract is often observed. One defect does not preclude the occurrence of others.
Piśmiennictwo
1. Jabłońska-Jesionowska M, Zawadzka-Głos L: Diagnostic evaluation of congenital respiratory stridor in children. New Med 2019; 1: 3-13.
2. Spencer S, Yeoh BH, Aspersen PPV, Fitzgerald DA: Biphasic stridor in infancy. Med J Aust 2004; 180(7): 347-349.
3. Gryczyńska D: Otorynolaryngologia dziecięca. Alfa-Medica Press, Bielsko-Biała 2007.
4. Martins RH, Dias NH, Castilho EC et al.: Endoscopic findings in children with stridor. Braz J Otorhinolaryngol 2006; 72(5): 649-653.
5. Bhimij S: Vascular rings clinical presentation. Medscape updated Mar 27, 2015.
6. Bovè T, Demanet H, Casimir G et al.: Tracheobronchial compression of vascular origin. Review of experience in infants and children. J Cardiovasc Surg (Torino) 2001; 42(45): 663-666.
7. Pumberger W, Voitl P, Göpfrich H: Recurrent respiratory tract infections and dysphagia in a child with an aortic vascular ring. South Med J 2002; 95(2): 265-268.
8. Garritano FG, Carr MM: Characteristic of patients undergoing supraglottoplasty for laryngomalacia. Int J Pediatr Otorhinolaryngol 2014; 78(7): 1095-1100.
9. Lai S-H, Liao S-L, Wong K-S: Cardiovascular-associated tracheobronchial obstruction in children. Cardiol Young 2013; 23: 233-238.
10. Jabłońska-Jesionowska M, Zawadzka-Głos L: Respiratory stridor in children due to congenital abnormalities of the great vessels. New Med 2015; 4: 3-5.
11. Hernanz-Schulman M: Vascular rings: a practical approach to imaging diagnosis. Pediatr Radiol 2005; 35(10): 961-979.
12. Hernanz-Schulman M: Vascular rings: a practical approach to imaging diagnosis. Pediatr Radiol 2005; 35(10): 961-979.