A hot environment (hot discomfort or thermal stress conditions), for which the heat balance equation is positive (accumulation of heat in the body), exceeds the threshold of thermal comfort, i.e. PMV ≥+2. The basis for risk assessment in a hot environment is PN-85 N-08011 standard "Ergonomics: Hot Environments. Estimation of heat stress on working man, based on the WBGT index” [10]. The index is used for the assessment of average, prolonged exposure of humans to heat, ignoring very-short-duration heat strain or strains close to comfort zones.
WBGT value is calculated according to the following formula: WBGT=0.7tnwb+0.3tg, where:
tnw = natural wet-bulb temperature,
tg = black globe thermometer temperature.
To determine thermal strain with the WBGT index, additional measurement or assessment is needed, which is based on: the table presented in the standard listing occupations; metabolic rate (energy production); information from workers on acclimation to heat (or lack of it); and assessment of air flow (perceptible, imperceptible). Thereafter, a benchmark WBGT value corresponding to the given metabolic rate is read out from the table [1, 10]. The WBGT value calculated for the working post is then compared to benchmark values. These correspond to the level of exposure of any person without any side effects. These values may change, if e.g. psychomotor disturbances that might cause accident at work are found.
However, the occupation categories proposed in the standard give no obvious clue in determining safe temperature limits as regards the work of the operating theatre personnel. The table proposed in the standard for work in a standing posture ("light manual work, such as writing, sewing, or work involving hand and palm, such as work with the use of small locksmith´s and carpenter´s tools”) classifies such work as light work (652). The admissible temperature limit in this case (benchmark WBGT value) is WBGT = 30°C (29°C for unacclimated persons). On the other hand, the table counts "actions performed with palms or hands with muscle tension, such as ramming, filling” as moderate work, causing increased metabolism 1302. In that case the WBGT ceiling is 28°C (26°C for unacclimated persons)
If these thresholds are exceeded [10]:
– either thermal strain at the working post should be lowered by appropriate methods (adjustment of the environment, level of load, duration of stay in the given environment and the use of individual protection measures),
– or a detailed analysis of thermal strain with more precise methods should be carried out.
At the same time, one should bear in mind that the binding hygienic standards concerning the methods of studying load in persons working in protective clothing in various thermal environment conditions are developed based on research carried out with the participation of young males. In reality, persons of various ages can be found in a given working post. The strain level may be inappropriate for other age groups [2].
In addition, the above-mentioned benchmark WBGT values have been developed for normally clad persons (i.e. thermal insulation index Icl=0.6 Clo). If the properties of the clothing used differ substantially from the benchmark values (e.g. water-vapour resistant wear) expert advice should be sought [10], because such a situation should lead to the lowering of the benchmark value. Besides, although conformity with the requirements of that standard protects the inside of the human body against exceeding a core temperature of 38°C, it does not guarantee the meeting of other physiological criteria, such as heart rate or sweat output. This is so because the index is a compromise between the pursuit of a precise indicator and the need to carry out easy measurements in an industrial environment. A better indicator is the sweat output calculated according to the equation of heat exchange between humans and the environment [11, 12].
It seems, therefore, that the optimal solution in determining the thermal stress of the operating suite personnel would be to carry out direct measurements of both metabolic rate [13] and thermal insulation values of sets of medical clothing, in simulated conditions, with the participation of workers in a climatic chamber and the use of a thermal manikin, which are used for that purpose in research carried out at the Central Institute for Labour Protection – National Research Institute [2].
Optimization of working comfort of operating suite personnel
The environment, or conditions of climate, affects the human body through several factors, including: air temperature, humidity and velocity, and mean radiant temperature. These values and their configuration determine thermal comfort, heat and cold sensation in humans. Other factors, such as level of activity, thermal insulation and air and water vapour permeability of clothing, also influence the perception.
In the rooms in which an artificial microclimate is created, attempts are made to provide thermal comfort conditions. The most important variables affecting thermal comfort are the above-discussed parameters combining to form the thermal comfort equation:
– energy production (quantity of heat produced in the body)
– thermal insulation of clothing
– air temperature
– mean radiant temperature
– relative air velocity
– partial pressure of water vapour in the surrounding air.
Thermal comfort may be achieved through adequate combination of the above-mentioned variables, by using various heating and air-conditioning installations. Among air-conditioning tasks, the following may be listed [9, 17]:
– retention of adequate air temperature (22-25°C),
– retention of suitable relative humidity of the air (55-60%; humidity above 65% may cause intracrystalline corrosion and damage medical apparatus, whereas humidity below 50% is conducive to static electricity accumulation),
– supplying fresh and clean air to the operating theatre and the operating area,
– ensuring even airflow through the operating theatre,
– elimination to the minimum of whirls and secondary air movements.
For a given heat production and kind of clothing, any combination of air temperature, mean radiant temperature, relative humidity and air velocity may be determined to find the optimum conditions of thermal comfort for humans [9].
The thermal comfort equation was derived from experiments carried out with the participation of American academic youth. In order to apply it to the assessment of comfort of the operating suite personnel, surgeons in particular, some adjustments should be made taking into account the specific nature of the occupation, including the influence of stress and of special protective clothing on the feeling of thermal comfort. At the same time, such an assessment should take into account additional factors that may have an effect on thermal comfort, such as the number of individuals in a given room, room colours and air pressure.
From the point of view of optimization of the thermal environment of the operating theatre, a conflict of interests arises between the working conditions of the surgeon and the medical and technical personnel, and the conditions for the patient.
The surgeon´s and other personnel´s work is performed in standing postures, often bent, in protective clothing, within the range of operation of heat radiators. It is associated with intrinsic physical and mental strain. Its inherent feature is stress of various origins (operations of multiple injuries, transplantology, deaths, team work, work overload). It is difficult to provide thermal comfort for the operating suite personnel in such circumstances. At the same time, these conditions are not favourable to the patient, as it is difficult to maintain a thermoneutral zone in the operating room, i.e. such a range of temperatures as to minimize the consumption of oxygen, loss of fluids and heat (comfortable temperature for a nude human is approx. 29°C). In a hot environment the patient is cooled by using cold fluids in the peritoneal washing and by facing the organs with cold gauze sheets. On the other hand, a scantily dressed patient, whose period of stay in the operating theatre may be long, is vulnerable to heat escape from the inside of the body through the open operating area. In such conditions he/she is covered with an additional thermal insulation layer (particularly lengthy neurosurgeries and laryngologic surgeries), warm fluids are used for washing wounds and body cavities, and warm sheets are used for covering internal organs. After all, unplanned hypothermia is not a rarity [14].
Due to their purpose, operating theatres are rooms in which thermal and humidity parameters of the air and strictly defined microbiological and dust purity requirements must be met. Satisfying these conditions ensures working comfort of the operating team and adequate climatic conditions for the patients, and greatly reduces hazards to the health and lives of patients resulting from pollution of the surrounding air.
The requirements concerning air-conditioning and ventilation of the operating suite determine the temperature, minimum rate of air exchanges in each of the rooms, their purity class and relative humidity, noise level, etc. In various countries there are various standards of temperature for operating theatres, 18-25°C on average. In Germany it is 20-25°C, in France 22-25°C, in Sweden and Switzerland 25°C. In Poland the requirements regarding air temperature, humidity and velocity for ventilation and air-conditioning of operating theatres are as follows [15]:
– temperature 22-25 °C (hyperaseptic, aseptic, septic rooms)
– relative humidity 55% (procedure and operating rooms 40-60%),
– maximum air velocity 0.4-0.5 m/s (0.2 m/s procedure and operating rooms).
At the same time, the possibility of adjustment of internal temperature should be available in every operating room, at least within the range of several degrees, independently of the general regulation related to external temperature.
In the rooms in which no air-conditioning or mechanical ventilation systems operate, the appropriate temperature of the air should be provided by a central heating system, and the minimum number of replacements by gravitational ventilation.
Setting a temperature in the operating theatre that would provide comfort to all persons is rather unlikely. The preferable temperature is different for surgeons, who perform more dynamic work, and for anaesthesiologists, who perform more static work. Research carried out by Polish scientists found that, in this country´s climate, surgeons are fitter when the temperature of the incoming air is 19°C. According to English researchers, it depends on the actions performed by the personnel and their mental tension. A distinct issue is the microclimate in the children´s operating theatre, in which operating procedures with the use of an open incubator are carried out in temperatures of 25-28°C.
The above-described PN-EN ISO 7730 standard [1], which is used to determine if the conditions in a given place of work meet the requirements of comfort, may be applied in designing new environments or in assessing the existing working places. In annex D of that standard, thermal comfort requirements at working posts are presented:
1. It is recommended that PPD be <10% (which corresponds to -0.5>PMV<0.5). Based on that assumption, a comfortable range of each of the environment parameters, for instance temperature (e.g. as a function of activity and clothing insulation), may be found based on the PMV formula.
2. It is recommended that relative humidity be 30-70%. Such conditions allow one to reduce the risk of irritation to the eyes, growth of bacterial flora and development of diseases of the respiratory track, the sensation of wet or dry skin, and static electricity.
However, as in the case of the WBGT index (presented above), it is difficult to properly classify the work of the operating suite personnel in order to calculate thermal comfort indices. This applies in particular to surgical work which could be classified in the 4th or 5th category (Annex A):
Group 4: work in a standing posture, low activity ("purchasing, laboratory work, light industry”); 93W/m2 (1.6 met);
Group 5: work in a standing position, moderate activity ("shop assistant, housework, machine work”); 116 W/m2 (2.0 met).
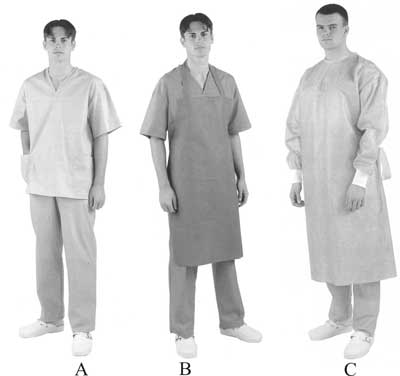
A distinct problem is the selection of appropriate protective clothing for the operating suite personnel. Such clothing is designed to protect against bacterial pathogens and infectious biological agents. Advanced operating clothing should be comfortable, light and non-restricting to the surgeon´s and other personnel´s movements. At the same time it should be made of a fabric that is soaking-resistant, impermeable to fluids and blood, and permeable to the sterilizing agent (water vapour), enabling skin respiration, having thermoregulatory properties. In our times, recommended one-way gowns are made of a non-woven material or paper strengthened with a multiple-use film (Gore-Tex type, for instance).
Knowledge of the metabolic rate of a given worker of the operating suite and his/her clothing insulation allows calculation of the range of operating temperature to corresponding to the thermal comfort zone. It also allows the reverse calculation to be performed: for a given temperature of the room and worker´s activity, desirable clothing insulation parameters that provide comfort may be determined. At the same time, one should bear in mind that the binding hygienic standards concerning the methods of studying strain in persons working in protective clothing in various thermal environment conditions were developed based on research carried out with the participation of young males. In reality, persons of various ages can be found in a given working post. The strain level may be inadequate for other age groups [2].
In order to select worker´s clothing fitting the thermal conditions of the environment and his/her activity, it may be worthwhile to assess a moderate thermal environment. Worker´s wear should be selected in such a way that he/she perceives thermal conditions as comfortable. Conditions outside the thermal comfort range are perceived by the worker as wearisome and may adversely affect his/her work quality. A problem arises when specific working conditions (e.g. in the operating suite) require use of certain protective clothing.
If above-normal temperature is found in the working place, workers´ comfort may be increased by increasing air velocity. ASHRAE Standard 55-1992 and ASTRAE Standard 55-2004 [16, 17] discuss the topic of how air velocity increase (with the use of a fan, for instance) may compensate for the increase in temperature, when it exceeds the higher limit of the comfort range in the summer season. Unfortunately, in particular in the case of the operating theatre, both temperature and air velocity increases are unfavourable. In the former case, the emission of volatile organic compounds (VOCs) may increase; in the latter, evaporation of volatile or even less volatile chemicals from open surfaces may also increase, and concentration of dust over the area may rise as well.
Also, modification of air humidity is not recommended, for it results not only in changed concentration of water-soluble chemicals and bioaerosols, but affects the perceived air quality.
On the basis of the literature review, wherever human activity requires artificial adjustment of the microclimate of the room, thermal conditions are sought that provide comfort to the majority of individuals present in the room. Due to biological differences, it is impossible to satisfy all persons present in the room with regard to the microclimate. What should be sought are optimal thermal comfort conditions, i.e. a state in which the greatest possible number of people feel thermal comfort [9].
The need to create thermal comfort results mainly from the increasing awareness of the influence of thermal comfort on work quality. Numerous experiments confirm that maximum physical and intellectual capabilities of humans are reached when humans work in thermal comfort conditions, whereas hot or cold discomfort adversely affects work quality [6, 7, 9].
To ensure high quality of medical services provided by the operating suite personnel to the patient, it is very important to create comfortable working conditions. However, the working posts occupied by operating suite personnel have not been analysed in depth as yet, which is confirmed by the difficulty in finding these occupations in tables proposed for the assessment of thermal comfort. For that reason, such assessment should be carried out specifically for individual workers of the operating suite. This would provide reliable data on the actual strain and allow practical organizational and climatic solutions to be designed.
Piśmiennictwo
1. EN ISO 7730:2005: Moderate thermal environments – Determination of the PMV and PPD indices and specification of the conditions for thermal comfort. 2. Koradecka D. Work safety and ergonomy (a book in Polish). Central Institute for Labour Protection – National Research Institute, Warsaw 1999. 3. Sołtyński K., Konarska M., Pyryt J., Sobolewski A. Test research of a new generation thermal manikin. Third International Meeting on Thermal Manikin Testing 3 IMM, 12-13 października 1999. 4. Sołtyński K., Konarska M., Pyryt J., Sobolewski A. Research on typical medical work clothing on humans and on a thermal manikin. Third International Meeting on Thermal Manikin Testing 3 IMM,2000. 5. Traczyk WZ, Trzebski A. Human physiology with the element of clinical and applied physiology (a book in Polish). PZWL Warsaw 2004. 6. Grether WF. Human performance at elevated environmental temperature. Aerospace Med. 1973; 44:747-55. 7. Pilcher JJ, Nadler E, Busch C. Effects of hot and cold temperature exposure on performance: a meta-analytic review. Ergonomics 2002;45:682-698. 8. EN ISO 9886:2004 Ergonomics – Evaluation of thermal strain by physiological measurements (ISO 9886:2004). 9. Fanger P.O. Komfort cieplny, Arkady 1974. 10. EN 27243:1993Hot environments. Estimation of the heat stress on working man, based on the WBGT-index (wet bulb globe temperature) (ISO 7243: 1989). 11. EN ISO 7933:2004 Ergonomics of the thermal environment – Analytical determination and interpretation of heat stress using calculation of the predicted heat strain (ISO 7933:2004). 12. EN 12515:1997 Hot environments - Analytical determination and interpretation of thermal stress using calculation of required sweat rate (ISO 7933:1989 modified). 13. EN ISO 8996:2004 Ergonomics of the thermal environment – Determination of metabolic rate (ISO 8996:2004). 14. Arndt K, 1999, Lenhardt R, Kurz A, Marker E, Goll V. Clinical guideline for the prevention of unplanned perioperative hypothermia. AORN J 1999;70:204-206. 15. Sitko K. Air-conditioning and ventilation of the existing operating theatres (article in Polish). Weiss Klimatechnik Polska Sp. Z o.o., WWW.wktp.pl. 16. ANSI/ASHRAE 55-2004 Thermal Environmental Conditions for Human Occupancy. 17. ANSI/ASHRAE Standard 55-1992 Thermal Environmental conditions for human occupancy, Atlanta 1992, ASHRAE Addendum 55a,1994.