Terèzia Seres1, Zoltán Szakács2, Éva Kellős1, Márta Simon2, Attila Terray Horváth2, Veronika Fáy3, Jelena Karaszova3, Andrea Kontra3, Olivia Lalátka3, Mária Csóka4, Gyula Domján5
Research on ropinirole treatment of restless leg syndrome
1Doctoral School, Semmelweis University, Budapest, Hungary
Head of Department: Gyula Domján, MD, PhD
2Department of Neurology, Medical Centre, Hungarian Defence Forces, Budapest, Hungary
Head of Department: Zoltán Szakács, MD, PhD
3Rehabilitation Centre, Combined Szent István and Szent László Hospital, Budapest, Hungary
Head of Centre: Veronika Fáy, MD, PhD
4Department of Nursing, Faculty of Health Sciences, Semmelweis University, Budapest, Hungary
Head of Department: Zoltán Balogh, MD, PhD
5Institute of Health Care Development and Clinical Methodology, Faculty of Health Sciences, Semmelweis University, Budapest, Hungary
Head of Institute: Professor Gyula Domján, MD, PhD
Summary
Introduction. The restless leg syndrome is a clinical syndrome which frequently remains unrecognized. It belongs to a group of sleep-dependent movement disorders. It is the second most common reason for chronic sleep deficiency and hypersomnia during the day. In accordance with the international recommendations, its treatment is to be started with a dopamine agonist, the most favourable of them being (due to their efficiency and few side effects) the new selective D2/D3 agonists.
Aim. The aims of the study were to explore whether ropinirol remained effective with time, whether the dose of the drug escalated, and whether side effects affected therapy.
Material and methods. In this paper, the effectiveness of a D2/D3 agonist, ropinirole, was tested in patients with restless leg syndrome. 51 patients suffering from idiopathic restless leg syndrome received ropinirole in monotherapy in a dosage of 0.25-1.5 mg/day. The efficiency of the medicine has been verified in three ways: with tracking surveys, actigraph testing and the Forced Immobilization Test.
Results. 80% of our patients responded weel to the therapy. There was a considerable improvement based on the tracking surveys after ropinirole treatment. Time without movement of the limbs measured by actigraph testing, as well as the time spent in bed, were significantly longer. Also, the FIT index was lower after than before the treatment.
Conclusions. Based on our results, it can be stated that the restless leg syndrome can be effectively treated with ropinirole monotherapy.
Introduction
Restless Leg Syndrome (RLS) has been already known by the 17th century (1). In 1940s, public medical attention was brought to this disease by Ekbom, a Swedish neurologist (2). However, nowadays it still remains underdiagnosed, as surveys show that up to 5-15% of the population suffer from this disease (3).
In the international classification of sleep-wakefulness disorders, the restless leg syndrome is classified as a sleep-related movement disorder.
Symptoms of RLS show a circadian rhythm and they worsen in an inactive awaken state, thus, the symptoms frequently appear while falling asleep. The symptoms include a disturbing, tense feeling (dysaesthesia), mainly in the lower limbs, that occur in an inactive awaken state, often directly after going to bed. The symptoms can be relieved only by performing pedalling or kicking motion or getting up and walking. The resulting chronic disruptions in circadian rhythm may lead to mental and affective disorders and autoagression.
Based on the above described clinical features, a patomechanism including both peripheral and central nervous system that relates to the sleep and wakefulness regulation was proposed. Motor system may also be involved. Recent research suggest multiple elements that may contribute to the development of the disease, including the hypofunction of post-synaptic dopamine (DA) receptors in the motor-related areas of striatum, the role of opioid receptors in the modulation of DA release, the importance of iron metabolism to the central nervous system (4-5).
The first successful treatment for this disease was already described more than 300 years ago by Willis, who treated a patient with serious symptoms with a an opioid. Ekbom also observed the beneficial effects of opioids and other sedatives and hypnotics.
The beneficial effect of levodopa became well-known in the 1980s. It was verified in several papers, including the placebo controlled double-blinded trials (6-7). The consequences of the long-term levodopa treatment, which include the need for augumentation of the dosis and the rebound phenomenon, resulted in the decrease of use of this substance, especially after the appearance of the modern dopamine agonists. Based on the current clinical experience, dopamine agonists with longer half-life are less likely to result in the need for augumentation of the dosis and in the rebound phenomenon, but are still effective in reducing the symptoms of restless leg syndrome. Currently, they are recommended as the first-line treatment for RLS (8).
The recommendations of the American Academy of Sleep Medicine (AASM) of the 1999 remain the most commonly applied ones. They are acknowledged as having good scientific evidence (9, 10). The updated version of these recommendations was published in 2004, making it possible to include the results of the newest papers on dopamine agonists (11, 12).
In our laboratory, we examined the effectiveness of ropinirole in patients suffering from restless leg syndrome.
Ropinirole is a non-ergotamine derivative dopamine agonists as it mainly binds with D3 receptors and, to lesser extent, with D2 receptors. Its plasma half-life accounts for about 5 to 6 hours. Renal elimination prevails. It is reported to be effective in treatment of RLS (13, 14), even in patients resistant to other forms of therapy (15, 16). Long-term use causes only a slight need for augumentation of the dosis which is easily manageable (17).
Aim
The aims of the study were to explore whether ropinirol remained effective with time, whether the dose of the drug escalated, and whether side effects affected therapy.
Material and methods
51 patients suffering from idiopathic restless leg syndrome were included in the study. At the beginning of the treatment and after 12 weeks of ropinorole monotherapy, they were asked to fill in a tracking survey. The efficacy of the medicine was examined in three ways: with tracking surveys, actigraph testing and the Forced Immobilization Test (FIT test).
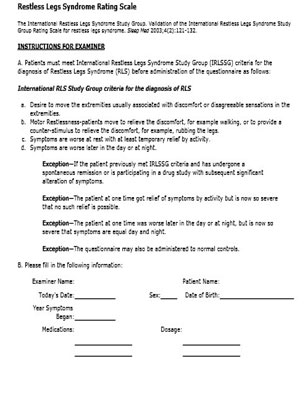
Tracking survey with self-report subjective measurement scale
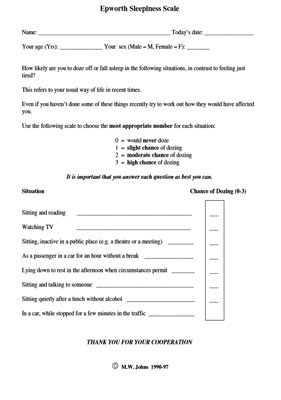
We used a survey which was developed by the International Restless Leg Study Group and is widely accepted in the international literature. The survey covers the characteristic symptoms of the disease dividing them into 12 items. To assess each item, the severity of each symptom is assessed on a scale from 1 to 5. This enables a subjective self-estimation of the patient’s state. The reliability of the survey is sufficient, as it had been validated (Annex 1). Therapeutic efficacy was monitored with the Epworth Sleepiness Scale as well as the Insomnia Severity Index (ISI) (Annexes 2-3).
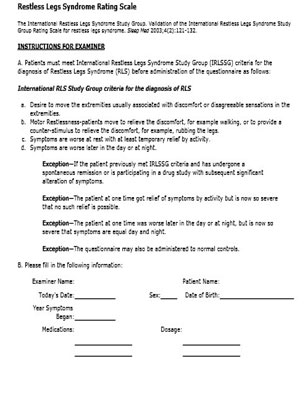
Annex 1. Restless Leg Syndrome Rating Scale

Annex 1. Restless Leg Syndrome Rating Scale

Annex 1. Restless Leg Syndrome Rating Scale

Annex 1. Restless Leg Syndrome Rating Scale
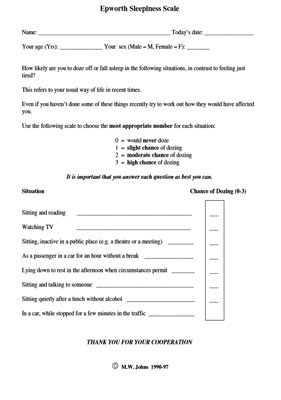
Annex 2. Epworth Sleepiness Scale

Annex 3. Insomnia Severity Index
Actigraph testing during sleep
The efficacy of the therapy was also verified by actigraph testing. For this purpose, the Actiwatch (Mini Mitter®) tool was used (fig. 1 and 2).

Fig. 1. Actiwatch actigraphy devices

Fig. 2. Actigraphy test
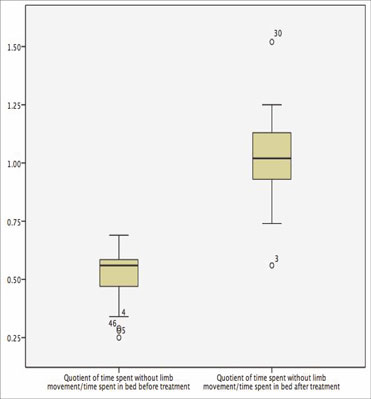
In the actigraph testing, a small-sized motion sensor (accelometer) detects limbs and torso movements. It enables continuous registration for a time ranging from few hours to many weeks and data storage. It is fastened on the ankle or on the wrist of the patient. Thanks to the software, RLS events can be filtered out of the physiological movements with a high degree of certainty. Also, the intensity and timing of these movements is registered. There are many practical applications of this device. It can also measure the range of motion (18). The ciclicity of the movements can be verified. In this research, we calculated the change of the quotient of time spent without limb movements to total time spent in bed – the increase of this quotient represents the improvement of the symptoms.
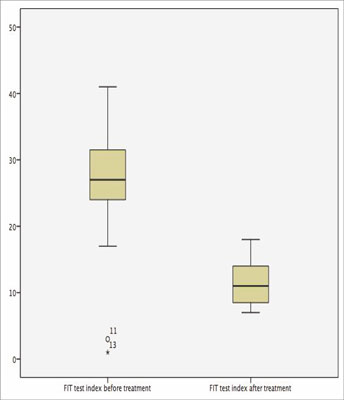
Forced Immobilization Test (FIT Test)
This test is used to verify the intensity of the main RLS symptom – the movement incentive. It is carried out during the daytime. During the test, the patient sits still on the bed with his legs upright. During the test, the limbs are to be relaxed, but motionless. EMG electrodes are placed bilaterally in the musculus tibialis anterior and the musculus quadriceps femoris. Involuntary leg movements are registered. The test takes 60 minutes. An event is recorded when a myoclonic activity is detected in EMG. FIT index is calculated by dividing the number of events by the time of recording them (in minutes) and multiplying it by sixty. The test is positive when the FIT index is higher than 10.
Statistical methods
Changes that occurred during the therapy are depicted in the “box-and whiskers” diagrams. A one-sample t-test was applied to compare the groups. This test can be used with coherent samples only. The analysis and the diagrams were created with the STATISTICA 7.0 software.
Results
We examined 106 patients with RLS and qualified 60 of them, who presented with idiopathic RLS, into our research. Dopamine2 agonist (ropinirole) monotherapy was prescribed for 51 of these patients. The dose ranged from 0.25 to 1.5 mg/day. Eight patients received the 1.5 mg dose. More than 80% of patients responded well to the therapy. The therapy was continued for over a year with no signs of the need for augumentation present. The average age of the patients was 55.2 ± 15.1 years of age in men (n = 18) and 55.9 ± 13.3 years of age in women (n = 33). The effects of the therapy were measured with tracking surveys, the actigraph testing and the FIT test.
Therapeutic effectiveness was monitored at the beginning of the treatment and after 12 weeks of the treatment with the International RLS Study Group Rating Scale (IRLS), the Epworth sleepiness scale and the Insomnia Severity Index (ISI). The change in IRLS score after ropinirole treatment suggests a substantial improvement. Daytime sleepiness measured with Epworth Sleepiness Scale decreased following treatment with ropinirole. Treatment with ropinirole was associated with an improvement of the Insomnia Severity Index (ISI) (tab. 1).
Tab. 1. Effect of ropinirole treatment on symptoms of RLS measured with IRLS Rating Scale, Epworth Sleepiness Scale and Insomnia Insomnia Severity Index
| | Before treatment | After treatment | N | t | df | p-value |
| Mean | Std. error mean | Std. deviation | Mean | Std. error mean | Std. deviation |
| IRLS rating scale | 25 | 1.421 | 6.029 | 9.06 | 0.551 | 2.338 | 51 | 10.673 | 50 | 0 |
| Epworth Sleepines Scale | 13.89 | 0.718 | 3.046 | 6.17 | 0.513 | 2.176 | 51 | 7.965 | 50 | 0 |
| Insomnia Severity Index | 19.33 | 0.836 | 3.548 | 7.72 | 0.685 | 2.906 | 51 | 12.89 | 50 | 0 |
The quotient of time spent without limb movement to total time spent in bed measured with actigraph testing improved considerably following the ropinirole treatment (fig. 3). The change was statistically significant (analysed with one-sample-Student’s t-test; p=0.01).
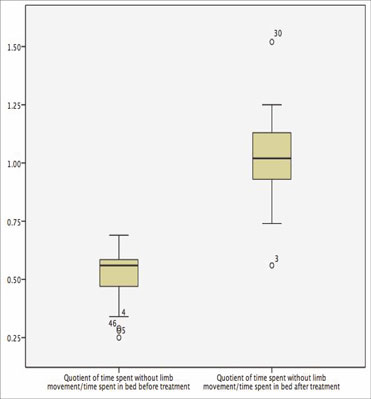
Fig. 3. The effect of ropinirole treatment on the quotient of time spent without limb movement to total time spent in bed measured by actigraph monitoring
The results of the Forced Immobilized Test also improved considerably after the treatment (fig. 4). The change was statistically significant (analysed with one-sample-Student’s t-test; p=0.01).
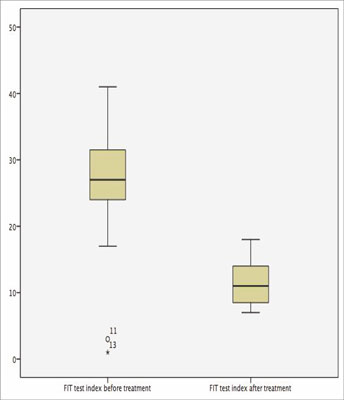
Fig. 4. FIT test results before and after ropinirole treatment
Discussion
The restless leg syndrome is a frequent form of sleep-dependent movement disorders and the second leading cause of chronic sleep deficiency, as well as of hypersomnia during the day. The disease remains often unrecognized, and its serious symptoms can significantly reduce the patient’s quality of life. What is important, these very symptoms can be considerably relieved with the current therapeutic options.
The pharmacotherapy is based on four groups of medications: dopaminergic drugs, opioids, benzodiazepines and antiepileptic drugs. The dopaminergic drugs are the most thoroughly examined and the most effective ones. The treatment algorithm recommend them as the first-line treatment, especially in cases of severe RLS. All the dopamine agonists used for treating Parkinson’s syndrome were proven to be effective in the treatment of restless leg syndrome (19, 20, 21).
Conclusions
We measured the effectiveness of ropinirole monotherapy in 51 patients suffering from RLS. The medication caused significant improvement in self-assessment as well as in actigraphic testing and FIT test, both of which enable to objectivize the results. Ropinirole was well tolerated and the treatment was not interrupted in any of the patients due to the adverse effects. In some patients, however, the adverse effects, such as gastrointestinal side effects, hypotension, peripheral edema, resulted in the dose reduction.
Based on our results, it can be stated that the symptoms of restless leg syndrome can be treated effectively using ropinirole monotherapy.
Piśmiennictwo
1. Willis T: De Animae Brutorum. Wells and Scott, London 1672. 2. Ekbom K: Restless legs: clinical study oh hitherto overlooked disease in legs characterized by peculiar paresthesia ('Anxietas tibiarum'), pain and weakness and occuring in two main forms, asthenia crurum paraesthetica and asthenia crurum dolorosa. Acta Med Scand 1945; 158: 5. 3. Dauvilliers Y, Winkelmann J.: Restless legs syndrome: update on pathogenesis. Curr Opin Pulm Med. 2013 Nov; 19(6): 594-600. 4. Phillips B, Young T, Finn L et al.: Epidemiology of restless legs symptoms in adults. Arch intern Med 2000; 160: 2137-2141. 5. Earley CJ, Kuwabara H, Wong DF et al.: Increased synaptic dopamine in the putamen in restless legs syndrome. Sleep 2013 Jan 1; 36(1): 51-57. 6. Akpinar S: Treatment of restless legs syndrome with levodopa plus benzeraside. Arch Neur 1982; 39: 739. 7. Brodeur C, Montplaisir J, Godbout R et al.: Treatment of restless legs syndrome and periodic movements during sleep with L-Dopa: a double blind, placebo controlled study. Neurology 1988; 38: 1845-1848. 8. von Scheele C: Levodopa in restless legs. Lancet 1986; 2: 426-427. 9. Schapira HV: Restless legs syndrome – an update on treatment options. Drugs 2004; 64(2): 149-158. 10. Chesson AL Jr, Wise M, Davila D et al.: Practice parameters for the treatment of restless legs syndrome and periodic limb movement disorder – an American Academy of Sleep Medicine report. Sleep 1999; 22: 961-968. 11. Hening W, Allen R, Earley C et al.: The treatment of restless legs syndrome and periodic limb movement disorder – an American Academy of Sleep Medicine review. Sleep 1999; 22: 970-998. 12. Hening WA, Allen RP, Earley CJ et al.: An Update on the Dopaminergic Treatment of Restless Legs Syndrome and Periodic Limb Movement Disorder. Sleep 2004; 27: 560-583. 13. Littner MR, Kushida C, Anderson WM et al.: Practice parameters for the Dopaminergic Treatment of Restless Legs Syndrome and Periodic Limb Movement Disorder – an American Academy of Sleep Medicine Report. Sleep 2004; 27: 557-559. 14. Adler CH, Hauser RA, Sethi K et al.: Ropinirole for restless legs syndrome: a placebo-controlled crossover trial. Neurology 2004; 62: 1405-1407. 15. Allen R, Becker PM, Bogan R et al.: Ropinirole decreases periodic leg movements and improves sleep parameters in patients with restless legs syndrome. Sleep 2004a; 27: 907-914. 16. Allen RP, Tidswell P, Ritchie S: Clinical efficacy of ropinirole for RLS is unaffected by age-at-onset phenotype: pooled analysis of three clinical trials. American Academy of Neurology, Miami Beach, FL, USA, April 9-16, 2005. Neurology 2005b; 64 (suppl. 1): A41-42. 17. Bogan RK, Fry JM, Schmidt MH et al.: Ropinirole in the treatment of patients with restless legs syndrome: a US-based randomized, double-blind, placebo-controlled clinical trial. Mayo Clin Proc 2006; 81: 17-27. 18. Chokroverty S.: Overview of sleep & sleep disorders. Indian J Med Res. 2010 Feb;131:126-40. 19. Trenkwalder C, Garcia-Borreguero D, Montagna P et al.: Ropinirole in the treatment of restless legs syndrome: results from the TREAT RLS 1 study, a 12 week, randomised, placebo controlled study in 10 European countries. J Neurol Neurosurg Psychiatry 2004; 75: 92-97. 20. Winkelman JW, Bennet S: Augmentation with ropinirole in the long-term treatment of restless legs syndrome. Sleep 2000; 25 (suppl.): A253. 21. Stiasny K, Oertal WH, Trenkwalder C: Clinical symptomatology and treatment of restless legs syndrome and periodic limb movement disorder. Sllep Med Rev 2002; 6: 253-265.