© Borgis - New Medicine 3/2008, s. 67-69
Eliza Brożek-Mądry, *Lidia Zawadzka-Głos, Mieczysław Chmielik
POST-OPERATIVE FOLLOW-UP IN CHILDREN WITH CHOANAL ATRESIA
Department of Paediatric ENT, Warsaw Medical University, Poland
Head of Department: Prof. Mieczysław Chmielik, MD, PhD
Summary
Choanal atresia in children can appear as an isolated congenital malformation or coexists in certain syndromes. The Department of Paediatric Otolaryngology of the Medical University of Warsaw is one of a few centres where surgical treatment of choanal atresia is performed.
Aim: Objective evaluation of nasal patency and laryngological examination of patients operated on with a transnasal approach. Material and method: A group of seven children with choanal atresia operated transnasally was examined. In this group nasal patency was evaluated using rhinomanometry and a complete laryngological examination concentrating on palate motility and phonation was performed.
Results: In the studied group the laryngological examination with particular interest in the oral and nasal cavity is presented. There were three patients with nasalization and three patients with nasal cavity obturation to various extent presented in rhinomanometry.
Conclusions: 1. Material analysis of children operated on in 1995-2007 shows an increased number of transnasal operations, which correlates with the world literature. 2. Rhinomanometry is a reliable and non-invasive method in postoperative monitoring of nasal patency. 3. Nasal decongestants show a lesser influence on the rhinomanometry results on the operated side, especially in children presenting in follow-up with nasal patency disorders. 4. Presence of nasalization in operated patients suggests the necessity of further examination of phonation in follow-ups.
INTRODUCTION
Choanal atresia (CA) is a disease that may involve choanae completely or may exist unilaterally, which underlies the differences of the intensity of symptoms, such as breathing and feeding difficulties. The incidence is evaluated to be 1:5000 to 1:8000 of live births. It is observed more frequently in females, unilaterally and on the right side (1, 2). In 70% of patients with choanal atresia there is observed a bony-membranous atretic plate, while 30% present with bony atretic plate (3). Genetic background, maternal diseases and medications used during pregnancy are discussed as factors contributing to the incidence of CA. In CHARGE syndrome, which includes coloboma (C), heart disease (H), choanal atresia (A), retardation of growth and development (R), genitourinary anomaly (G), and ear defect (E), there is a mutation described in more than half of the patients in the gene CHD7, locus 8q12 (4, 5, 6, 7). The cellular role of the protein CHD7 is in organization of chromatin (CHD7-chromodomain helicase DNA-binding protein). Among medications used during pregnancy, methimazole and carbimazole can be responsible for CA (8, 9).
Choanal atresia is managed surgically. Ways of surgical approach to choanal atresia in children involve transnasal and transpalatal approach. In adults a transseptal approach is also described.
Transnasal surgical techniques include classical surgery, endoscopic surgery, laser surgery, and balloon dilation. In the literature we often meet with different techniques of mucosal flap formation as a method of yielding mucosa for newly formed bony canal as well as with trials of abandoning stenting of the nasal cavities. In recent years many operations have been performed transnasally due to spectacular development of endoscopic techniques (10, 11).
Most frequently evaluated parameters in patients´ follow-up after surgical treatment of choanal atresia include nasal patency, sense of smell and hearing (12, 13, 14, 15). Nasal patency was evaluated using either acoustic rhinometry or rhinomanometry. Leclerc et al. examined olfaction in 7 patients and concluded that nasal patency disorders may lead to weaker development of olfactory nerves on the side with choanal atresia. Zawadzka et al. evaluated efficiency of the Eustachian tube in children operated with a transnasal and transpalatal approach and did not notice any differences between them in the measurement of acoustic impedance.
Between 1959 and 2007 there were 136 patients operated on in the Otolaryngology Department of the Medical University in Warsaw (96 females and 40 males; F/M ratio ~ 5:2). The total number of operations in this period was 183 including 47 reoperations. Unilateral CA was diagnosed in 77 patients and bilateral CA in 59 children. To achieve the aim of this paper we found the addresses of 19 patients and of this group only 7 were able and agreed to come for the examination; thus the paper has a preliminary character.
AIM
Objective evaluation of nasal patency and laryngological examination of patients operated on with the transnasal approach.
MATERIAL AND METHOD
A group of 7 children operated on transnasally attended the outpatient clinic for the follow-up. These children had a complete laryngological examination with evaluation of the soft and hard palate and nasalization. They also underwent anterior rhinomanometry with and without mucosal decongestion (abcRHINO).
RESULTS
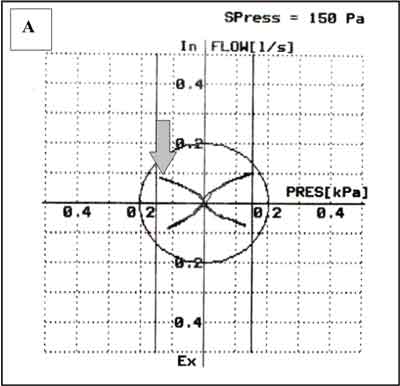
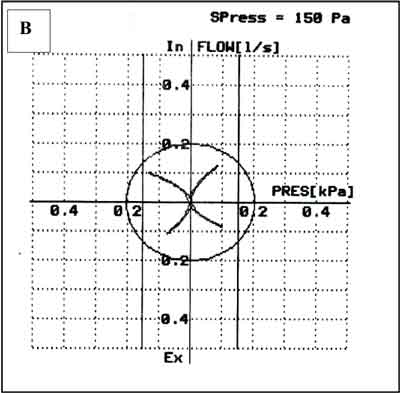
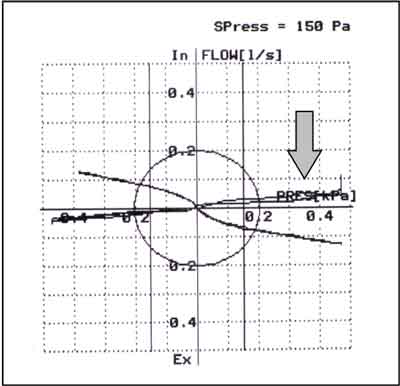
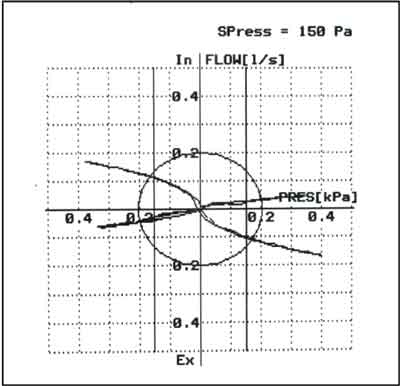
Brief characteristics of the examined children are presented in table 1. In this group we also included one boy with bilateral choanal atresia, born in 2001 and operated on twice transnasally (in 2001 and 2002). Table 2 shows the observations made in laryngological examination: two patients had nasal septum deviation and one had asymmetry of the soft palate. In the child with bilateral choanal atresia there was observed a high-arched, symmetric palate. Open nasalization was not observed but three patients presented with closed nasalization. According to the scale 0-1-2, two of our patients were stage 1 and one was stage 2. Due to infantile cerebral palsy in a patient with bilateral atresia nasalization was not evaluated. In rhinomanometry one patient (ZA) had a complete blockade of air flow on the operated side. Patient BM had a significant nasal patency disorder on the operated side. Patient NK had lesser changes on the operated side. Two examples of the rhinomanometric curves are presented in figure 1, in patients with mentioned nasal patency disorders. On the opereated side sick we can observe no reaction to decongestin.
Table 1. Patient´s characteristics (UCA – unilateral choanal atresia).
| Patient | Year of birth | Diagnosis | Year of operation | Method |
| WG | 2003 | UCA sin | 2004 | transnasal |
| BM | 2002 | UCA dex | 2006 | transnasal |
| GW | 2000 | UCA dex | 2003 | transnasal |
| NK | 2000 | UCA sin | 2006 | transnasal |
| AJ | 1996 | UCA dex | 1997, 2000 | transnasal |
| ZA | 1987 | UCA sin | 1992,2x1993, 2001 | transnasal |
Table 2. Otorhinolaryngological examination in children.
| Patient | Anterior rhinoscopy | Palate |
| mobility | Symmetry/anatomy |
| WG | No aberrations | normal | symmetric |
| BM | Straight nasal septum, right nasal cavity constricting posteriorly, nasal patency asymmetry - disordered on the right side | Submucosal soft palate cleft | symmetric |
| GW | No aberrations | normal | symmetric |
| NK | Nasal septum deviation to the left, nasal patency maintained | - | asymmetry - uvula shifting to the left, left palatine arch shorter than the right and lowered |
| AJ | No aberrations | normal | symmetric |
| ZA | Nasal septum deviated to the right, constant discharge on the left side, nasal cavity completely blocked on the left side | normal | symmetric |
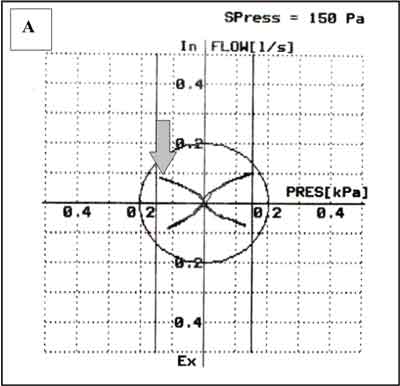
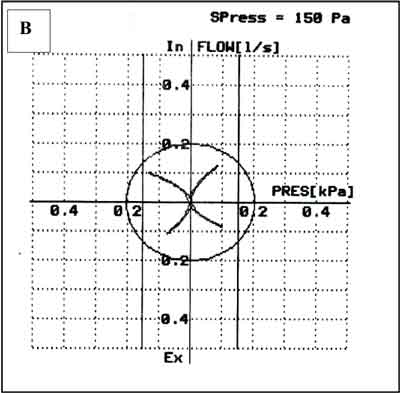
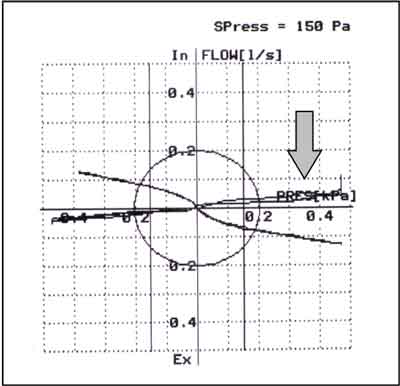
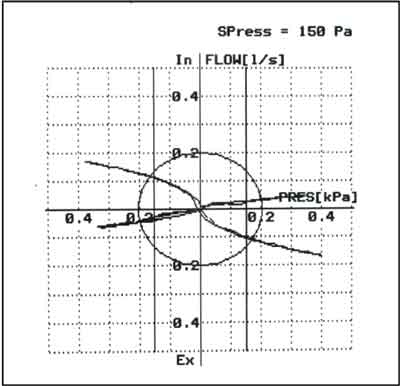
Fig. 1. Examples of the poorest rhinomanometry results in two children operated for choanal atresia on the side with an arrow. A – without decongestion, B – after decongestion.
CONCLUSIONS
1. Material analysis of children operated on in 1995-2007 shows an increased number of transnasal operations, which correlates with world literature.
2. Rhinomanometry is a reliable and non-invasive method in postoperative monitoring of nasal patency.
3. Nasal decongestants show a lesser influence on
the rhinomanometry results on the operated side especially in children presenting in follow-up with nasal patency disorders.
4. Presence of nasalization in operated patients suggests the necessity of further examination of phonation in follow-ups.
Piśmiennictwo
1. Chmielik M.: Otorynolaryngologia dziecięca. PZWL, Warszawa 2001. 2. Chmielik M, Ranocha C.: Niewykształcenie nozdrzy tylnych. Nowa Pediatria 1999, 11 (1/99): 22-23. 3. Brown OE, Pownell P, Manning SC.: Choanal atresia: a new anatomic classification and clinical management applications. Laryngoscope 1996; 106: 97-101. 4. Bosman EA, Penn AC, Ambrose JC, et al.: Multiple mutations in mouse Chd 7 provide models for CHARGE syndrome. Hum Mol Genet. 2005 Nov 15; 14 (22): 3463-76. Epub 2005 Oct 5. 5. Lalani SR, Safiullah AM, Fernbach SD, et al.: Spectrum of CHD7 mutations in 110 individuals with CHARGE syndrome and genotype-phenotype correlation. Am J Hum Genet. 2006 Feb; 78 (2): 303-14. Epub 2005 Dec 29. 6. Sanlaville D, Verloes. CHARGE syndrome: an update. European Journal of Human Genetics (2007) 15, 389-399. 7. Dumic M, Cvitanovic M, Saric B, et al.: Choanal stenosis, hypothelia, deafness, recurrent dacryocystitis, neck fistulas, short stature, and microcephaly: Report of a case. Am J Med Genet 2002 Dec 1; 113 (3): 295-7. 8. Di Gianantonio E, Schaefer C, Mastroiacovo PP, et al.: Adverse effects of prenatal methimazole exposure. Teratology 2001 Nov; 64 (5): 262-6. 9. Barwell J, Fox GF, Round J, et al.: Choanal atresia: the result of maternal thyrotoxicosis or fetal carbimazole? Am J Med Genet 2002 Jul 22; 111 (1): 55-6; discussion 54. 10. Khafagy YW.: Endoscopic repair of bilateral congenital choanal atresia. Laryngoscope 2002; 112: 316-319. 11. Schoem SR.: Transnasal endoscopic repair of choanal atresia: why stent? Otolaryngol Head Neck Surg 2004; 131: 362-366. 12. Djupesland P, Kaastad E, Franzen G.: Acoustic rhinometry in the evaluation of congenital choanal malformations. Int J Pediatr Otorhinolaryngol 1997 Sep 18; 41 (3): 319-37. 13. Leclerc JE, Leclerc JT, Bernier K.: Choanal atresia: long-term follow-up with objective evaluation of nasal airway and olfaction. Otolaryngol Head Neck Surg. 2008 Jan; 138 (1): 43-9. 14. Holzmann D, Ruckstuhl.: Unilateral choanal atresia: surgical technique and long-term results. J Laryngol Otol 2002 Aug; 116 (8): 601-4. 15. Zawadzka-Głos L, Bielicka A, Chmielik M.: Assessment of hearing in children in postoperative treatment of choanal atresia. New Medicine 2/2002 vol. 5.