© Borgis - New Medicine 3/2008, s. 73-76
*Eliza Brożek-Mądry, Lechosław P. Chmielik, Mieczysław Chmielik
NASAL CYTOLOGY AND BACTERIOLOGY IN CHILDREN WITH CHRONIC SINUSITIS
Department of Otolaryngology, Medical University of Warsaw
Head of Department: Prof. Mieczysław Chmielik, MD, PhD
Summary
Introduction: Both nasal cytology and culture examination are quite simple procedures to perform in children due to their painless and non-invasive character. The results of these tests can help in evaluation of the mucous membrane and further in diagnostics and therapy.
Aim: The assessment of nasal cytology and bacteriology in children with chronic sinusitis. Introduction of preliminary results for further investigation.
Material and method: A group of thirty-five children with chronic rhinosinusitis underwent nasal cytology – the exfoliative method – both from the inferior nasal concha and from underneath the middle concha. They also had a culture taken from underneath the middle concha and from the maxillary sinus during the sinus surgery. Exfoliated material for nasal cytology was transferred onto microscope slides, fixed with 95% alcohol and dyed with haematoxylin-eosin. Such prepared cytology was next evaluated under a biological microscope, Motic model 2820. This evaluation included the presence and count of epithelial cells such as columnar, squamous, basal and goblet cells and also alluvial cells such as neutrophils, lymphocytes, eosinophils and monocytes.
Results: Nasal cytology was compared in the aspect of areas it was taken from. We also compared the results of bacteriological examination obtained from the maxillary sinus and from underneath the middle nasal concha.
Conclusions: Cytological examination in patients with chronic rhinosinusitis may reveal its inflammatory character. In children it seems more valuable to obtain a specimen for cytological examination from the area of the middle meatus and middle concha. The bacteriology results give some indications for further research.
INTRODUCTION
Diagnosing chronic rhinosinusitis in children is a serious and difficult task. These difficulties in the paediatric population are connected with the abilities of self-assessment by a child – the symptoms, their level of intensity, but also with frequent interference of uncomplicated viral infections of the upper respiratory tract, or additional symptoms of adenoid or tonsillar hypertrophy. Another problem may be connected with cooperation with the young patient. Thus for objective evaluation of the paediatric patient with chronic rhinosinusitis it is mandatory to search for methods facilitating the process of qualification of a young patient for adequate treatment and further monitoring. These methods should be easy to repeat and non-invasive.
AIM
The assessment of nasal cytology and bacteriology in children with chronic sinusitis. Introduction of preliminary results for further investigation.
MATERIAL
The examined group consisted of patients under 18 years with chronic rhinosinusitis (according to modified Melzer criteria) (1) who were qualified for surgical treatment in the Department of Otolaryngology, Medical University of Warsaw in 2005-2007. From this group we excluded patients with cystic fibrosis, ciliary dysfunction, neoplastic diseases, and children under immunosuppression. The examined group consisted of 35 patients, 18 girls, 17 boys aged 6 to 18 (mean age 11.3; med. 12). Nine patient had an allergic disease in anamnesis.
METHOD
Examinations performed in children:
– bacteriological examination from the mucosa under the middle concha and from the maxillary sinuses intraoperatively on both sides,
– exfoliative cytology taken from the inferior nasal concha taken 1 cm from the anterior pole of the concha and from the middle meatus in the area of the maxillary sinus, anterior ethmoidal cells and frontal sinus ostium – on both sides analogically.
Exfoliated material for nasal cytology was transferred onto microscope slides, fixed with 95% alcohol and dyed with haematoxylin-eosin. Such prepared cytology was next evaluated under a biological microscope, Motic model 2820. This evaluation included the presence and count of epithelial cells such as columnar, squamous, basal and goblet cells and also alluvial cells such as neutrophils, lymphocytes, eosinophils and monocytes (3, 4).
RESULTS
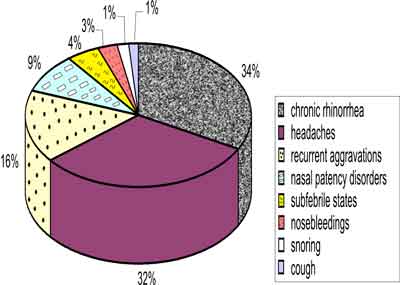
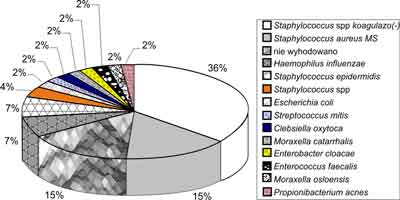
The most frequently observed symptoms in the examined group are presented in figure 1. Among the symptoms the most frequent were chronic discharge in the nasal cavities and headaches. Sixteen percent of examined children suffered from recurrent aggravations. Bacteriological examination of the area of the middle meatus presented in figure 2 shows no growth in more than one fourth of the group and the most frequently cultured pathogens were coagulase-negative Staphylococci (22%), Staphylococcus aureus (19%) and to a lesser extent Haemophilus influenzae (11%). Other bacteria were cultured in ≤5% of our patients. The results of culturing maxillary sinus contents presented in figure 3 show higher incidence of coagulase-negative Staphylococci (36%) and comparable number of cultures with Staphylococcus aureus (15%). In 15% of patients no growth was observed in the specimen.
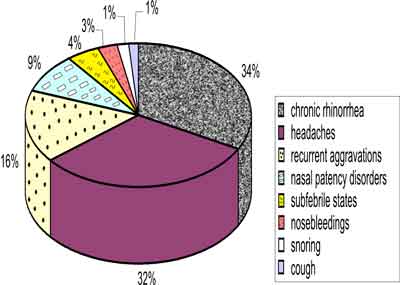
Fig. 1. Symptoms observed in study group.

Fig. 2. Bacteriology results from middle meatus in children with chronic rhinosinusitis.
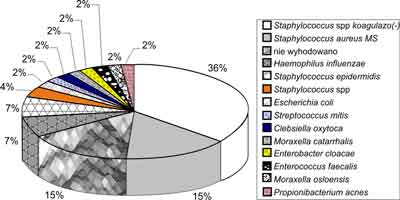
Fig. 3. Bacteriology results from maxillary sinus in children with chronic rhinosinusitis.
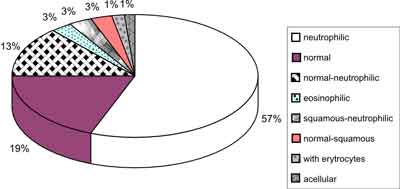
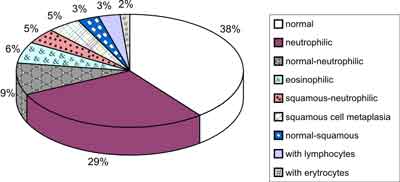
The results of cytological examination in children with chronic rhinosinusitis obtained from the inferior nasal concha presented in figure 4 show a neutrophilic cytogram in more than half of the patients (57%) while in 19% the cytogram was normal, i.e. with the majority of columnar cells (fig. 6 A, B) The results of cytology obtained from the mucosa of the middle meatus are shown in figure 5, and here the incidence of normal cytogram is higher (38%), while a neutrophilic cytogram is observed in 29%. Eosinophilic cytograms doubled when the specimen was obtained from the middle meatus (3-6%).
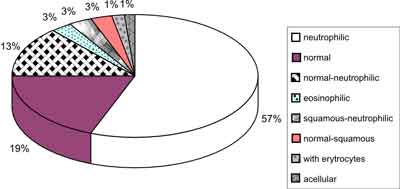
Fig. 4. Cytology results from inferior concha.
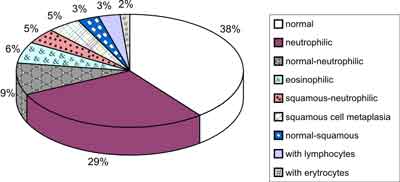
Fig. 5. Cytology results from middle concha.

Fig. 6. A – columnar cells with cilia and neutrophils, B – columnar ciliated epithelium, C – single eosinophil, D – goblet cells between columnar cells.
DISCUSSION AND PRELIMINARY CONCLUSIONS
Cytological examination of the nasal mucosa is non-invasive and allows us to evaluate the condition of the mucous membrane of patients with CRS (4). In most cytological examinations from the inferior nasal concha we obtained mostly alluvial cells – neutrophils. In cases where eosinophils were observed in the specimen, they underwent a process of degranulation. The fact that the number of eosinophils increases in the specimen taken from the middle meatus suggests potential involvement of eosinophils in a subgroup of children with rhinosinusitis. In normal cytological examination obtained from the middle meatus there were more commonly observed ciliated columnar cells, which could have a practical implication in obtaining a piece of mucosa for ciliary evaluation.
Due to the differences between the cytology in the two areas it is suggested to elaborate one place of obtaining the specimen. The fact that we observed more neutrophilic cytograms from the inferior concha than from the middle meatus of children with chronic rhinosinusitis seems to point to the fact that the mucous membrane of the inferior concha is more exposed to the environment or the specimens have been taken too far anteriorly.
Bacteriological results show a higher incidence of coagulase-negative Staphylococci in the maxillary sinus of children with chronic rhinosinusitis than in the middle meatus. In the literature it is postulated that coagulase-negative Staphylococci in the maxillary sinus are a contamination, but we should reconsider this opinion (5).
Piśmiennictwo
1. Meltzer i wsp.: Rhinosinusitis: establishing definitions for clinical research and patient care Journal of Allergy and Clinical Immunology, 2004 Dec. 114 (6). 2. Tarchalska-Kryńska B.: Diagnostyka cytologiczna błony śluzowej nosa. Kiedy i jak ją wykonać? Alergia 2003. 3. Tarchalska-Kryńska B.: Diagnostyka cytologiczna błony śluzowej nosa. Magazyn Otolaryngologiczny 2007; 6 (2): 51-54. 4. Brożek-Mądry E, Chmielik M.: Nasal cytology in children with chronic rhinosinusitis or nasal septum deviation. New Medicine 2007 Oct. -Dec. 11 (4). 5. Rombaux Ph, Gigi J, Hamoir M, et al.: Bacteriology of chronic sinusitis: the bulla ethmoidalis content. Rhinol 2002; 40: 18-23.