*Emil Korporowicz1, Piotr Firlej2, Dariusz Gozdowski3, Dorota Olczak-Kowalczyk1
Shear bond strength of different materials used for pit and fissure sealing
Wytrzymałość połączenia różnych materiałów stosowanych do uszczelniania bruzd i szczelin
1Department of Paediatric Dentistry, Medical University of Warsaw, Poland
Head of Department: Professor Dorota Olczak-Kowalczyk, MD, PhD
2Zhermapol Sp. z o.o., Warsaw, Poland
3Department of Experimental Statistics and Bioinformatics, Warsaw University of Life Science, Poland
Head of Department: Professor Wiesław Mądry, PhD
Streszczenie
Wstęp. Uszczelnianie bruzd i szczelin stanowi skuteczną metodę zapobiegania próchnicy, czego dowiedziono w wielu badaniach klinicznych. Zazwyczaj w technice tej stosuje się uszczelniacze na bazie żywic, choć w niektórych badaniach sugeruje się również stosowanie płynnych kompozytów. Najnowsze generacje tych materiałów obejmują samoadhezyjne kompozyty płynne i materiały kompozytowe typu bulkfill. Retencja tych materiałów stanowi jeden z głównych czynników przyczyniających się do zapobiegania próchnicy. Ich skuteczność kliniczną można oceniać za pomocą testów wytrzymałości połączenia, które pozwalają określić zdolność materiału do wiązania się ze szkliwem.
Cel pracy. Celem pracy była ocena wytrzymałości wiązania ze szkliwem następujących materiałów: Helioseal F (Ivoclar Vivadent), Vertise Flow (Kerr) i SDR (Dentsply Sirona) z systemem łączącym XP Bond (Dentsply Sirona).
Materiał i metody. Do trzech grup losowo przydzielono 15 stałych trzecich zębów trzonowych usuniętych z przyczyn ortodontycznych i opracowanych w celu uzyskania płaskiej powierzchni szkliwa. Na opracowanych powierzchniach przy użyciu formy polimeryzowano badane materiały ? Helioseal F, Vertise Flow oraz SDR z użyciem systemu łączącego XP Bond. Próbki zanurzono w wodzie destylowanej i pozostawiono w temperaturze 37°C na 24 godziny, a następnie umieszczono w urządzeniu Instron. Urządzenie zatrzymywało się przy pęknięciu próbki i rejestrowano obciążenie. Obliczano wartości wytrzymałości wiązania. Przeprowadzono analizę statystyczną. Ponadto w celu ustalenia rodzaju uszkodzenia próbki poddano badaniu z użyciem mikroskopu optycznego.
Wyniki. Analizą objęto 35 próbek, w tym 11 Helioseal F, 12 Vertise Flow i 12 SDR. Najwyższą wartość wytrzymałości wiązania odnotowano dla materiału SDR z systemem wiążącym XP ? 23,70 (± 6,35) MPa, nieco niższą dla Vertise Flow ? 20,10 (± 3,95) MPa oraz najniższą dla Helioseal F ? 15,93 (± 3,17) MPa. Stwierdzono statystycznie istotną różnicę między kompozytami płynnymi (SDR i Vertise Flow) a uszczelniaczami na bazie żywicy (Helioseal F). Stwierdzono 18 pęknięć kohezyjnych w obrębie szkliwa, 14 pęknięć adhezyjnych i 4 pęknięcia typu mieszanego.
Wnioski. Materiał SDR z systemem wiążącym XP Bond oraz materiał Vertise Flow charakteryzują się statystycznie wyższą wytrzymałością wiązania niż materiał Helioseal F. Niemniej jednak kluczowa wydaje się również ocena kliniczna skuteczności tych materiałów.
Summary
Introduction. Pit and fissure sealing is a effective procedure in preventing caries, as proven in numerous clinical trials. Materials used for this technique are usually resin-based fissure sealants, but some studies suggested using flowable composites as well. The latest generations of these materials include self-adhesive flowable composites and bulk fill composites. Retention of these materials is one of the main factors that contribute to caries prevention. Therefore, shear bond strength tests that determine the material’s ability to bond with the enamel may help determine their clinical effectiveness.
Aim. The aim of the study was to assess the shear bond strength to the enamel of the following materials: Helioseal F (Ivoclar Vivadent), Vertise Flow (Kerr), and SDR (Dentsply Sirona) with XP Bond (Dentsply Sirona).
Material and methods. 15 permanent third molars extracted for orthodontic reasons with prepared flat enamel surfaces were randomly divided into three groups. Tested materials ? Helioseal F, Vertise Flow and SDR with XP Bond were polymerised on these surfaces, using a mould. Samples were immersed in distilled water, kept at 37°C for 24 h, and then installed in an Instron testing machine. The machine stopped at sample fracture and the load was recorded. Shear bond strengths were calculated. Statistical analysis was performed. Also, samples were assessed using an optical microscope to assess sample failure type.
Results. 35 samples, including 11 Helioseal F, 12 Vertise Flow, and 12 SDR were analysed. SDR with XP bond had the highest shear bond strength ? 23.70 (± 6.35) MPa; Vertise Flow ? 20.10 (± 3.95) MPa, and Helioseal F the lowest ? 15.93 (± 3.17) MPa. There was a statistically significant difference between flowable composites (SDR and Vertise Flow) and resin-based fissure sealant (Helioseal F). There were 18 cohesive sample fractures within the enamel, 14 adhesive fractures and 4 mixed.
Conclusions. The shear bond strength of SDR with XP Bond and Vertise Flow is statistically significantly higher than that of Helioseal F. However, it is also crucial to clinically assess the effectiveness of these materials.
Introduction
Occlusal surfaces can be prone to caries due to their complicated morphology (1, 2). Sealing pits and fissures, which was introduced in the 60s, isolates the pit from the oral cavity and indirectly facilitates the cleaning of masticatory surfaces (1, 2). This procedure is highly effective in preventing caries as proven in numerous clinical trials (3-6). Nowadays, there are four groups of dental sealants: resin-based sealants, glass ionomer cements, polyacid-modified composite resins, and resin-modified glass ionomer cements (6). Despite numerous clinical studies, it is still impossible to unequivocally tell which sealant is the most effective. International scientific societies recommend resin-based sealants as they prevent caries and offer an acceptable level of retention. Glass ionomer cements should only be used temporarily, when it is impossible to fully isolate the area to be treated (5, 7, 8).
More efficient solutions are still being researched. Some studies suggested using flowable composites to seal pits and fissures (9). Properties like low viscosity, porosity and better abrasion resistance (9-11) can make flowable composites a good alternative to conventional fissure sealants (2, 10, 12). The latest generations of these materials include self-adhesive flowable composites, not requiring bonding before application (which shortens the clinical procedure) (13) and bulk fill composites with reduced polymerisation stress, which could be particularly beneficial in deep fissures (14).
Sealant retention is directly linked to micromechanical bonding between composite and enamel. Shear bond strength tests determine the material’s ability to bond with the tooth, and, in consequence, may help determine its clinical effectiveness (15).
Aim
The aim of the study was to assess the shear bond strength to the enamel of the following materials: Helioseal F (Ivoclar Vivadent) ? resin-based fissure sealant, Vertise Flow (Kerr) ? self-adhesive flowable composite, and SDR (Dentsply Sirona) ? bulk fill composite (which requires using a bonding agent).
Material and methods
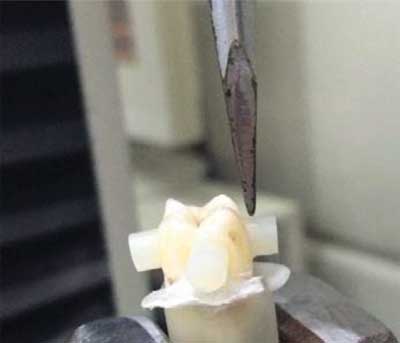
Fifteen permanent third molars extracted for orthodontic reasons were used in the study. Healthy enamel from mesial, distal, lingual and buccal surfaces was prepared; surfaces were finished with grind paper with different abrasive grades (#320-600). The prepared surfaces were then assessed with an optic microscope (Smart Optic Basic, Seliga Microscopes) to exclude samples with exposed dentin. Thirty-five flat enamel surfaces were qualified for the study. The roots of the teeth were immersed in acrylic resin to facilitate mounting in the testing machine. Surfaces were then polished with a slow speed brush using Clean Polish paste (Kerr). Teeth were randomly divided into different material groups. The assessed surfaces were covered in strips with a 4 mm round holes to have even enamel surfaces for material adhesion. Surfaces were etched with 36% orthophosphoric acid (Arkona) for 20 seconds and then thoroughly rinsed and dried until enamel turned chalk white. A 4 mm high and 4 mm wide Honigum-Fast Putty (DMG) cylindrical matrix was prepared, in which selected materials were placed: Helioseal F was light cured in two 2 mm layers. The first layer of Vertise Flow was brushed into the enamel surface and then light cured; then, second layer was applied and cured. XP Bond (Dentsply) was thoroughly applied, dried for 20 seconds, then its excess was removed with compressed air, and finally light cured for ten seconds prior to SDR application. One 4 mm SDR layer was applied. Every material was cured using the Bluephase Style (Ivoclar Vivadent) lamp (fig. 1). Then, the samples were immersed in distilled water, kept at 37°C for 24 h, and installed in an Instrom testing machine (fig. 2). Its crosshead speed was set at 0.5 mm/min. The machine stopped at sample fracture and the load was recorded. To calculate bond strength, the force [N] was divided by the area of the material surfaces adhering to the enamel, using the formula of circle area ? P = πr2 [mm2]. Results were expressed in [MPa].

Fig. 1. Samples with tested materials
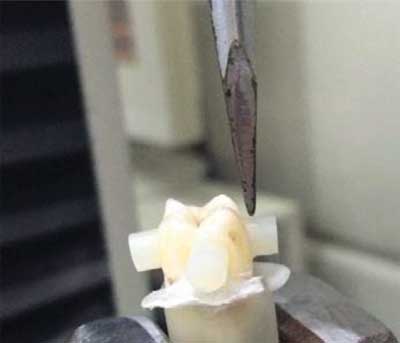
Fig. 2. Sample in the testing machine
Furthermore, the samples were evaluated with an optical microscope (Smart Optic Basic, Seliga Microscopes) with 17 x zoom to assess the sample failure. Samples were divided into the following groups: 1. Adhesive ? loss of bond between composite and enamel; 2. Cohesive ? within the material or enamel; 3. Mixed ? partially adhesive and cohesive.
Statistical analysis was conducted with the Statistica 12 software, using analysis of variance and Fisher’s least significant difference method for multiple comparisons. The p level was set at 0.05.
Results
Thirty-five samples, including 11 Helioseal F, 12 Vertise Flow, and 12 SDR were analysed. Table 1 presents the mean results for each material. SDR with XP bond had the highest shear bond strength ? 23.7 (± 6.35) MPa; Helioseal F the lowest ? 15.93 (± 3.17) MPa. Table 2 presents the results of the statistical analysis. There was a statistically significant difference between flowable composites (SDR and Vertise Flow) and resin-based fissure sealants (Helioseal F). There were 18 cohesive sample fractures within the enamel, which made it the most frequent fracture pattern. Adhesive fractures came second (14) and mixed came third (4). There were no cohesive fractures within the materials; however, there were two mixed, i.e. adhesive-cohesive fractures (some of the material remained at enamel surface). Table 3 presents the detailed results.
Tab. 1. Shear bond strengths of the assessed materials
| Material | Pressure [MPa] |
| Mean | SD |
| Helioseal F | 15.93 | 3.17 |
| Vertise Flow | 20.10 | 3.95 |
| SDR | 23.70 | 6.35 |
Tab. 2. P values of the results
| Material | SDR | Vertise | Helioseal F |
| Helioseal F | 0.000* | 0.043* | ? |
| Vertise Flow | 0.071 | ? | 0.043* |
| SDR | ? | 0.071 | 0.000* |
*statistical significance at p ≤ 0.05
Tab. 3. Patterns of sample failures
| Sample destruction type | Material |
| Helioseal F | Vertise Flow | SDR |
| Cohesive | 2 | 7 | 9 |
| Adhesive | 7 | 4 | 3 |
| Mixed | 2 | 2 | 0 |
Discussion
Some published studies compare shear bond strengths of self-adhering composites and pit and fissure sealants. Derelioglu et al. compared Vertise Flow with Grandio Seal (Voco), a highly filled fluoride-containing sealant. Vertise Flow was applied after enamel etching, as well as without etching. The shear bond strength of both pit and fissure sealant and the self-adhering composite was high after enamel etching, i.e. 42.6 (± 3.2) MPa and 49.8 (± 5.3) MPa, respectively (16). These results were higher than those obtained in the present study ? 15.93 (± 3.17) MPa for Helioseal F and 20.1 (± 3.95) MPa for Vertise flow. These differences could have resulted from different methodologies. The method used for calculating the surface area was not described by the authors, and the samples were not polished to smoothen the enamel surfaces (16). Schuldt et al. claimed that despite technical difficulties, using non-smoothened enamel surface is better as it leaves aprismatic enamel layer and therefore more accurately reflects pit and fissure sealing in clinical situations. They also claimed that, since their results were constant, surface curvature that is present when the samples are not smoothened, is of no importance in the final material assessment (17).
Dereiglou et al. showed a statistically significant difference between shear bond strengths for Vertise Flow without enamel etching ? 4.2 (± 0.9) MPa and after enamel etching ? 49.8 (± 5.3) MPa. Shear bond strength of Vertise Flow used without enamel etching was even lower than that of a resin-based sealant. The authors explained that these differences might have resulted from an inadequate ability of Vertise Flow to alter the enamel structure (contrary to orthophosphoric acid which altered enamel to a depth of 10-30 μm and created a surface prone to adhesion), and also its pH, at 1.9, which was higher than the pH of orthophosphoric acid. Furthermore, by thermocycling the samples, the authors demonstrated that self-etching composites degraded in water and therefore their bond strength was reduced (16). There was no statistically significant difference between the sealant and the self-adhering composite after enamel etching; however, Vertise Flow had higher mean shear bond strengths with enamel, which was explained by the prevalence of the GPDM adhesive monomer in the self-adhesive composite (16).
Schuldt et al. also compared the shear bond strength of Constic (DMG) (without and after enamel etching) and Helioseal F. Samples were aged in various ways: 1. they were stored in distilled water at 37°C for one day; 2. they were stored in distilled water at 37°C for three months; 3. they were stored in distilled water at 37°C for one day and then underwent thermocycling at 5-55°C with 5000 cycles (17). In the present study, the samples were stored in distilled water at 37°C for 24 hours, which corresponded to the first ageing type described by the authors. In a study conducted by Schuldt et al., Helioseal F shear bond strength was 19.1 (± 6.2) MPa and for self-adhesive ? Constic it was 17.1 (± 5.1) MPa after etching. The differences were not statistically significant. Similarly to Dereiglou’s study, the bond strength of self-adhesive composite used without etching was statistically significantly lower, i.e. 4.3 (± 1.6) MPa (17).
Biria et al. compared the shear bond strength of self-adhesive Enamel Loc (Premier Dental), used without enamel etching, and Conchise (3m Espe) ? resin-based fissure sealant. The shear bond strength of the self-adhesive material was statistically lower (5.59 (± 0.72) MPa) than that of the pit and fissure sealant, both after enamel etching and using a self-etch bonding agent (14.59 (± 1.19) MPa and 12.86 (± 1.98) MPa, respectively). These results were similar to Helioseal F results in the present study, i.e. 15.93 (± 3.17) MPa, even though the samples used by Biria et al. underwent thermocycling at 5-55°C (18).
Babaji et al. used Enamel Loc Self-Etch (Premier Dental), however they applied it onto surfaces etched with orthophosphoric acid. The mean shear bond strength of the material equalled 12.8 (± 4.8) MPa; however, this result was not statistically significantly different from the Helioseal F result, i.e. 13.7 (± 7) MPa. There was a statistically significant difference between the self-etch material and Tetric Flow composite (Ivoclar Vivadent), whose shear bond strength equalled 16.8 MPa (± 2.7), although it was applied after enamel etching without using a bonding agent (19). In the present study, shear bond strength of SDR bulk fill, after using XP Bond, was 23.7 (± 6.35) MPa, which was not statistically significantly different from Vertise Flow, but different from Helioseal F.
Ilie et al. compared Tetric Evo Ceram (Ivoclar Vivadent) and bulk fill (SDR and Tetric Evo Ceram Bulk Fill, Ivoclar Vivadent) shear bond strengths. Two self-etch bonding systems, Xeno V (Dentsply) and Adhese One F (Ivoclar Vivadent), were used before composite application. SDR shear bond strength on permanent tooth surfaces with etched enamel was 16.62 (± 9.07) MPa with Xeno V and 9.1 (± 5.15) MPa with Adhese One F (20). SDR bond strength lower than the one in the present study, i.e. 23.7 (± 6.35) MPa, could have resulted from using a different bonding system. Fifth generation XP Bond, after prior orthophosphoric etching, was used in the present study. Some studies established that the use of bonding systems requiring prior etching (4th or 5th generation) guaranteed a stronger bond than the use of self-etching systems (21-23). Furthermore, as shown by Ilie et al., despite the fact that bulk fill composites had similar, or even better retention results than traditional composites, the bonding system was the factor that statistically affected adhesion the most (20).
In the present study, Helioseal F samples most often underwent adhesive failures. Vertise Flow and SDR samples mainly underwent cohesive failures within the enamel, which means that the bond between the material and enamel was much stronger than the bond between dentin and enamel. Although the results of cohesive enamel fractures did not fully reflect the bond strength of a given material, they reflected a strong adhesive bond strength between enamel and composite. Also, there were no purely cohesive fractures within the assessed samples and there were adhesive-cohesive fractures only in four samples (two Helioseal F and two Vertise Flow), which reflected the high cohesive strength within these materials. For Dereiglou et al., there was mainly cohesive bond failure in Grandio Seal and Vertise Flow (after etching with orthophosphoric acid) groups (16). A higher number of cohesive fractures seemed to confirm that there was a strong bond between composite and dental tissues. For Ilie et al., most of the failures where adhesive, despite using a bonding agent prior to composite application (20). For Schuldt et al. adhesive damage prevailed in both pit and fissure sealants and in self-etching materials (17).
Conclusions
The shear bond strength of SDR with XP Bond and Vertise Flow is statistically significantly higher than that of Helioseal F. However, it is crucial to clinically assess the effectiveness of the afore-mentioned materials when sealing pits and fissures, including their retention and the prevalence of caries on the sealed surfaces as the clinical success of pit and fissure sealing depends on more than just shear bond strength.
Piśmiennictwo
1. Simonsen RJ, Neal RC: A review of the clinical application and performance of pit and fissure sealants. Aust Dent J 2011; 56(1): 45-58.
2. Erdemir U, Sancakli HS, Yaman BC et al.: Clinical comparison of a flowable composite and fissure sealant: a 24-month split-mouth, randomized, and controlled study. J Dent 2014; 42(2): 149-157.
3. Ahovuo-Saloranta A, Forss H, Walsh T et al.: Sealants for preventing dental decay in the permanent teeth. Cochrane Database Syst Rev 2013; 28(3): CD001830.
4. Wright JT, Tampi MP, Graham L et al.: Sealants for Preventing and Arresting Pit-and-fissure Occlusal Caries in Primary and Permanent Molars. A systematic review of randomized controlled trials ? a report of the American Academy of Pediatric Dentistry and the American Dental Association. J Am Dent Assoc 2016; 147(8): 631-645.
5. Beauchamp J, Caufield PW, Crall JJ et al.: Evidence-based clinical recommendations for the use of pit and fissure sealant: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 2008; 139: 257-268.
6. Wright JT, Crall JJ, Fontana M et al.: Evidence-based Clinical Practice Guideline for the Use of Pit-and-Fissure Sealants. A report of the American Dental Association and the American Academy of Pediatric Dentistry. J Am Dent Assoc 2016; 147(8): 672-682.
7. Welbury R, Raadal M, Lygidakis NA; European Academy of Paediatric Dentistry: EAPD guidelines for the use of pit and fissure sealants. Eur J Paediatr Dent 2004; 5(3): 179-184.
8. American Academy on Pediatric Dentistry Clinical Affairs Committee ? Restorative Dentistry Subcommittee; American Academy of Pediatric Dentistry Council on Clinical Affairs: Guideline on pediatric restorative dentistry. Pediatr Dent 2008-2009; 30(7): 163-169.
9. Corona SA, Borsatto MC, Garcia L et al.: Randomized, controlled trial comparing the retention of a flowable restorative system with a conventional resin sealant: one-year follow up. Int J Paediatr Dent 2005; 15(1): 44-50.
10. Kucukyilmaz E, Savas S: Evaluation of Different Fissure Sealant Materials and Flowable Composites Used as Pit-and-fissure Sealants: A 24-Month Clinical Trial. Pediatr Dent 2015; 7(5): 468-473.
11. Asefi S, Eskandarion S, Hamidiaval S: Fissure sealant materials: Wear resistance of flowable composite resins. J Dent Res Dent Clin Dent Prospects 2016; 10(3): 194-199.
12. Jafarzadeh M, Malekafzali B, Tadayon N, Fallahi S: Retention of a flowable composite resin in comparison to a conventional resin-based sealant: one-year follow-up. J Dent (Tehran) 2010; 7: 1-5.
13. Eliades A, Birpou E, Eliades T, Eliades G: Self-adhesive restoratives as pit and fissure sealants: a comparative laboratory study. Dent Mater 2013; 29(7): 752-762.
14. Bagherian A, Sarraf Shirazi A, Sadeghi R: Adhesive systems under fissure sealants: yes or no? A systematic review and meta-analysis. J Am Dent Assoc 2016; 147(6): 446-456.
15. Dhillon JK, Pathak A: Comparative evaluation of shear bond strength of three pit and fissure sealants using conventional etch or self-etching primer. J Indian Soc Pedod Prev Dent 2012; 30(4): 288-292.
16. Derelioglu S, Yilmaz Y, Celik P et al.: Bond strength and microleakage of self-adhesive and conventional fissure sealants. Dent Mater J 2014; 33(4): 530-538.
17. Schuldt C, Birlbauer S, Pitchika V et al.: Shear Bond Strength and Microleakage of a New Self-etching/Self-adhesive Pit and Fissure Sealant. J Adhes Dent 2015; 17(6): 491-497.
18. Biria M, Ghasemi A, Torabzadeh H et al.: Assessment of Microshear Bond Strength: Self-Etching Sealant versus Conventional Sealant. J Dent (Tehran, Iran) 2014; 11(2): 137-142.
19. Babaji P, Vaid S, Deep S et al.: In vitro evaluation of shear bond strength and microleakage of different pit and fissure sealants. J Int Soc Prev Community Dent 2016; 6: 111-115.
20. Ilie N, Scho?ner C, Bu?cher K, Hickel R: An in vitro assessment of the shear bond strength of bulk-fill resin composites to permanent and deciduous teeth. J Dent 2014; 42(7): 850-855.
21. Raposo CC, Santana IL: Shear bond strength of self-etch and total-etch adhesives to bovine enamel and dentin. Rev Odonto Cie?nc 2012; 27(2): 143-146.
22. Nagayassu MP, Shintome LK, Arana-Chavez VE, Fava M: Micro-shear bond strength of different adhesives to human dental enamel. J Clin Pediatr Dent 2011; 35(3): 301-304.
23. Kimmes NS, Barkmeier WW, Erickson RL, Latta MA: Adhesive bond strengths to enamel and dentin using recommended and extended treatment times. Oper Dent 2010; 35(1): 112-119.