Maria Wolniewicz, Alicja Piotrowska, Macej Pilch, *Lidia Zawadzka-GŇāos
Acute complication after frenulotomy – case report
Ostre powikŇāanie po podcińôciu wńôdzideŇāka jńôzyka – opis przypadku
Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Associate Professor Lidia Zawadzka-GŇāos, MD, PhD
Streszczenie
Kr√≥tkie wńôdzideŇāko jńôzyka to najczńôstsza wrodzona wada jńôzyka, w kt√≥rej wńôdzideŇāko jńôzyka jest nieprawidŇāowo przymocowane do dna jamy ustnej. Taka budowa anatomiczna znacznie ogranicza normalne ruchy jńôzyka, prowadzńÖc do licznych nieprawidŇāowoŇõci. Mińôdzy innym trudnoŇõci z karmieniem w okresie niemowlńôcym, wady wymowy, wady zgryzu, zaburzenia czynnoŇõciowe, dusznoŇõńá, dyzartrińô, problemy socjalne oraz mechaniczne. Istnieje kilka metod leczenia tego schorzenia. Wyr√≥Ňľniamy zar√≥wno metody zachowawcze w postaci ńáwiczeŇĄ ruchomoŇõci jńôzyka, terapii logopedycznej, jak i zabiegowe, do kt√≥rych zalicza sińô m.in. frenotomińô (tzw. plastyka wńôdzideŇāka jńôzyka). Technicznie zabieg frenotomii jest stosunkowo prosty do wykonania, jednak konieczna jest znajomoŇõńá budowy anatomicznej tej okolicy i zwińÖzane z tym moŇľliwoŇõci zakresu zabiegu oraz dokŇāadna ocena wńôdzideŇāka u danego pacjenta, by nie doprowadzińá do powaŇľnych, w tym zagraŇľajńÖcych Ňľyciu powikŇāaŇĄ.
W naszym artykule prezentujemy przypadek 16-letniej pacjentki leczonej przewlekŇāe z powodu wady zgryzu w prywatnym oŇõrodku stomatologicznym, kt√≥ra na podstawie konsultacji logopedycznej zostaŇāa zakwalifikowana do plastyki wńôdzideŇāka jńôzyka. Zabieg ten zostaŇā wykonany w znieczuleniu miejscowym i powikŇāany byŇā masywnym krwawieniem z jamy ustnej.
Summary
The shorten lingual frenulum is the most common congenital defect of the tongue, in which the frenulum is incorrectly tied to the bottom of the oral cavity. This type of anatomy significantly reduces normal tongue movement and leads to several abnormalities, like problems with breast feeding, speech impediments, malocclusion, functional disorders, dyspnea, dysarthria, social problems. We can distinguish several methods of the treatment of this abnormality, both conservative (like exercise of the muscles of the tongue or appropriate speech therapy) and surgical, most commonly frenulotomy. Technically, the procedure of the frenulotomy is quite easy to perform, but requires proper acquaintance with the anatomy of this region determining the potential extent of the procedure and thorough investigation of our patient in order to avoid possible serious, sometimes even life-threatening, complications.
In our article we present a case of a 16-year-old patient treated chronically due to malocclusion in a private dental center that was qualified for the procedure of frenulotomy after a speech therapy consultation. The procedure was performed under local anesthesia and unfortunately complicated by massive bleeding from the mouth.
Introduction
The short frenulum of the tongue, referred to in Anglo-Saxon literature as “ankyloglossia” or “tongue-tie”, is a variant of the anatomical structure in which we observe the limitation of the tongue protruding forward resulting from the strong attachment of the tongue to the bottom of the cavity through the fibrous, less often fibrous-muscular structure, the so-called the frenulum of the tongue. The degree of tongue fixation and the range of its mobility related to it may be different – from the difficulty of extending the tongue beyond the border of the lower dental arch to discreetly noticeable restriction of movement towards the chin. The aforementioned spread leads to differences in the clinical picture and means that the related problems may manifest themselves at various stages of life – from the neonatal period, through early childhood and adolescence, to adulthood (1-3).
The frequency of occurrence is determined in the literature in the range from 0.02% to almost 11%, which results from the ambiguity in the classifications and depends on the age of the studied population. The most serious defects appear already in the neonatal period, when we observe breastfeeding disorders in the form of problems with grasping the nipple by the child or nipple pain (resulting from pressure on the base of the nipple on the border of the soft and hard palate or point pressure and drawing the nipple in the area of the palatine uvula). It is one of the most common indications for surgery, possible to be done under local anesthesia, and the qualification usually takes place in the neonatal ward. The so-called “Continuous feeding cycle”, in which ineffective feeding leads to the sleep during breastfeeding, and then awakening, trying to attach and detach from the nipple without satisfying the thirst.
Speech development disorders are the dominant problem in early childhood. In this situation, qualification for the procedure takes place with the support of the speech therapist who takes care of the patient (3).
Below we present a case of a 16-year-old patient treated chronically due to malocclusion in a private dental center. After a speech therapy consultation, she was qualified for frenulotomy under local anesthesia. This procedure was complicated by massive bleeding from the mouth.
Case report
A 16-year-old patient was referred to the hospital due to bleeding after the surgery of the frenulum of the tongue. On the morning of admission, she underwent surgery of the frenulum under local anesthesia in a private dental center, where she was referred by an orthodontist providing corrective treatment. Qualification for the procedure took place after a specialist speech therapy consultation. According to the description, the course of the procedure was uneventful and afterwards the patient was discharged home. At home, the girl observed bleeding from the sublingual area. After the anesthesia had subsided, the attempts to move the tongue were painful and the bleeding intensified. She was unable to take food and fluids. In the evening hours, due to the deterioration of her general condition, weakness and continued bleeding, after a telephone consultation with the Ambulance Service, she was referred to the center carrying out the procedure for help. After an unsuccessful assessment of bleeding, the Ambulance Team was called, and the patient was transported to the ER of the Children’s Teaching Hospital of the University Clinical Center in Warsaw.
After the initial assessment in the ER examination, the laryngologist was called. During the examination, the patient was pale, had breathing problems (she was sitting in a slumped position), with proper oxygenation. She was unable to speak properly, in logical contact – to respond with gestures and eye-blinking. The interview was collected with the parent. The examination of the oral cavity showed a significant amount of fresh clots and bloody discharge. After suctioning and rinsing the area with Octenisept, a deep wound of the tongue was found – a longitudinal cut of the tongue with its cut off from the bottom of the mouth, accompanied by significant swelling of the tongue causing contact between the tongue and the palate, leading to an almost complete obstruction of the airways. The tongue was very tense and hard, and it was impossible to lead downwards due to severe pain. Under the supervision of an anesthesiologist, intravenous port was secured, control laboratory tests were taken, steroids, painkillers and antibiotics were administered. The patient was qualified to assess the wound in the operating theater conditions. The history of COVID-19 infection was negative, but due to the lack of a PCR result, the procedure was performed using enhanced personal protection measures. In a history of no chronic diseases, patient is allergic to Amoxicillin.
During general anesthesia, it was possible to fully assess the oral cavity, and apart from a massive cut of the tongue, extensive damage was found in the floor of the mouth, especially in the anatomical location of the frenulum and near the lower dental arch (fig. 1). A single absorbable suture was visible at the bottom of the mouth. The dorsal surface of the tongue was very bloodshot, brown in color. After careful palpation, there was no evidence of a tongue hematoma. There was no active arterial bleeding, and the preoperative bleeding was most likely the result of generalized bleeding from damaged mucosa and muscles and was intensified by changes in the muscle tone of the tongue. Layered suturing of the tongue was performed and an attempt was made to reconstruct the sublingual area. Suturing difficulties were encountered in the area of the floor of the mouth and the lower dental arch due to significant defects in the mucosa. Due to the massive swelling of the tongue, it was decided to leave the patient intubated until the swelling was reduced and to be monitored in the post-surgical room. The intravenous antibiotic therapy was continued: Cefuroxime and Clindamycin, also general steroid therapy. The examination after the procedure showed no signs of bleeding and no reopening of the wound edges. An Octenisept was used to clean the oral cavity and flushed topically with Clindamycin. It was decided to continue treatment in the ICU. On day 1, due to the increased swelling and hyperemia of the tongue, a contrast enhanced CT scan of the head was performed to exclude the presence of a hematoma. On day 3, the patient was extubated with good results, but left in the ICU. She did not require passive oxygen therapy. On day 4, she was transferred to the Laryngology Department (fig. 2). The patient was circulatory and respiratory efficient, the mobility of the tongue was maintained in all directions, but limited due to the inflammation resulting from the healing process, she could hardly pronounce words, and received meals in a semi-liquid/mushy form. The swelling and congestion of the tongue gradually decreased. There was no need to re-examine the wound. After each meal, a careful toilet was used – rinsing with water, brushing the teeth, and rinsing the mouth with a 1:1 solution of water and Octenisept. On the 9th day after surgery, the patient was discharged home. The patient was advised to use increased oral toilet and to gradually expand her diet and exercise tongue mobility.

Fig. 1. Dressing the wound in operating theater conditions

Fig. 2. 4th day after surgery
During the first outpatient check-up, about 1,5 week after discharge home and 3 weeks after the procedure, the patient reported a significant improvement in well-being, speech disorders in the form of a pronounced lisp. Until now, the patient had not extended her diet for fear of cracking the wound – she was following a mushy diet all the time. ENT examination revealed a significant amount of fibrin in the floor of the mouth, apart from that, there were visible single absorbable sutures. Edges the tongue was less swollen, smooth. The mobility of the tongue was significantly limited – the tip of the tongue barely touched the palate (fig. 3), while the maximum protrusion to the front was limited to the line of the lower dental arch (fig. 4). It was recommended to intensify tongue mobility exercises in conjunction with the introduction of chewing foods into the diet.

Fig. 3. 3 weeks after surgery – restriction of mobility of the tongue

Fig. 4. 3 weeks after surgery – significant attachment od tongue to the floor of the oral cavity, restriction of mobility
In the next control, about 7 weeks after the procedure, a significant improvement in speech quality was observed. The lisp has been greatly reduced. During this period, the patient performed regular and intensive speech therapy exercises and complied with dietary recommendations. ENT examination showed a marked reduction in tongue swelling and the color returned to normal (fig. 5). The lower surface of the tongue healed with the formation of adhesions bilaterally laterally from the area of the frenulum of the tongue, tightening when moving and slightly limiting its mobility. Nevertheless, the mobility of the tongue was improved – the patient was able to touch the palate more easily (fig. 6), she was able to touch the lower lip and lick it (fig. 7).

Fig. 5. 7 weeks after surgery – clearly marked apex

Fig. 6. 7 weeks after surgery, improvement od mobility, able to touch the palate with tip

Fig. 7. 7 weeks after surgery – ability to stick out the tongue
Discussion
Ankyloglossia is the most often congenital defect of tongue, an isolated defect, also it can coexist with others genetic syndromes such as Smith-Lemil-Opitz, Beckwith Weidmann, X-linked cleft palate (4). The term ankyloglossia was first described by Wallace in the 1960s. A condition in which the tip of the tongue does not protrude beyond the lower teeth of the incisors due to a significant restriction of tongue mobility. There are several classifications described in the literature, incl. Horton et al., Kotlow, Garcia Pola et al., Ruffoli et al. (5-8).
Below we present the Kotlow Classification, which includes 4 classes:
– Class I: mild ankyloglossia (12-16 mm),
– Class II: moderate ankyloglossia (8-11 mm),
– Class III: severe ankyloglossia (3-7 mm),
– Class IV: complete ankyloglossia (less than 3 mm) (5).
The defect can be recognized at any age and affects both adults and newborns. Most often detected in the neonatal period.
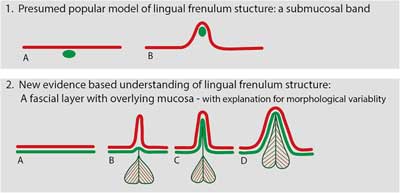
The frenulum of the tongue is located at the bottom of the mouth in the sublingual area, it comes in three anatomical varieties: 1. The frenulum is made up exclusively of the raised layer of the oral floor mucosa. It has the form of a transparent, flexible fold – “Transparent” frenulum; 2. The frenulum is made of the raised mucosa and the remaining fascia of the floor of the mouth. It has the form of a non-transparent and inelastic fold – “Opaque” frenulum; 3. The frenulum is made of the raised mucosa and the remaining fascia of the floor of the mouth together with the chin-lingual muscle. It has the form of a very thick inelastic fold – “Thick” Frenulum (fig. 8) (9). This is an odd structure in the midline. The adjacent anatomical structures visible during the examination are the sublingual muscle, the fold of the sublingual gland, while deeper under the mucosa, in the vicinity of the frenulum, there are: the salivary gland of the tongue, the lingual nerve, the arteries and deep veins of the tongue, the sublingual gland, and the submandibular gland duct (10, 11).
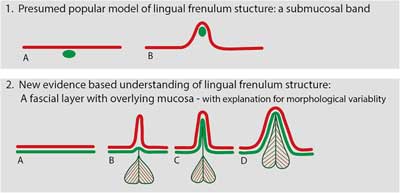
Fig. 8. 1. Location of the frenulum of the tongue A – when the tongue is relaxed, B – when the tongue is elevated. 2. Types of frenulum: red line – oral mucosa, green line – floor of mouth fascia, shape – the genioglossus muscle. A – The tongue is at rest, B – the first type “Transparent”, C – the second type “Opaque”, D – the third type, “Thick” Frenulum – the genioglossus muscle drawn into fold (9)
The defect is easily detectable, available in a basic oral examination.
Initially, it will show up with feeding problems. Along with the development of the oral cavity, its shape and size changes within 4-5 years after birth. Gradually, the symptoms may decrease (12).
Tongue-tie as an interdisciplinary problem involves many specialists: dentists, orthodontists, otolaryngologists, pediatricians, phoniatrists, speech therapists, and lactation advisers (13).
The incidence of anomalies in the form of a short frenulum of the tongue is 0.02-10.70%. According to the latest research, about 4-5% in newborns. About 1,5-3 times more often it affects the male sex (1, 3, 4, 13-15).
Increased incidence occurs in infants of mothers who abuse cocaine (16).
The short frenulum of the tongue leads to functional disorders, e.g.:
– Feeding disorders – difficulties in breastfeeding are particularly described in the literature. About a quarter of newborns with a short frenulum of the tongue will have a feeding problem. Additionally, in later age, due to the reduced mobility of the tongue, it is impossible to clean the molars after a meal, which will result in halitosis and the development of caries (17).
– Milder forms of tongue adhesion appear at a later age and result from the mechanical limitations of tongue mobility, leading to subjective discomfort in the sublingual area, the frenulum catching on the lower dental arch (12, 18).
– Speech disturbance – when pronouncing sounds – mainly “s, z, t, d, l, j, zh, ch, th, dg” in Polish mainly „sz, Ňľ, cz, dŇľ, r, l” (4, 18).
– Malocclusions – open bite, it is also believed that the limited mobility of the tongue leads to abnormal craniofacial development. The low position of the tongue leads to an increase in pressure both anteriorly and downwardly, thus promoting the development of mandibular prognosis with impaired maxillary development (3, 4).
– Social problems: unable to blow a balloon, to suck a lollypop, problems with kissing, difficulty playing the wind instruments (12, 18).
The above disorders are an indication for the procedure.
Not every case of short frenulum requires surgical treatment. When qualifying the patient, it is advisable to carefully assess the functioning of the language in meeting basic life needs, such as feeding or functioning in social life. Some of the observed symptoms can, but very rarely, be treated with appropriate speech therapy.
There are various methods of treating this anomaly, both conservative – exercise of the muscles of the tongue, speech therapy and surgery. The surgical methods include: Frenulotomy, i.e. transverse section of the frenulum, Frenulectomy – removal of the frenulum, and Frenuloplasty (fig. 9a-c) – the “Horizontal-to-Vertical Frenuloplasty” method or four-flap Z-frenuloplasty. All procedures can be performed under local or general anesthesia (4, 18). Due to the patient’s safety and greater control during the procedure, as the Department of Pediatric Laryngology, we opt for performing the procedure under short general anesthesia, after appropriate patient qualification. Post-operative speech therapy is also recommended (2, 13, 19).
Fig. 9a-c. Illustration of 4-flap Z-frenuloplasty operative technique. A – Initial markings of the incisions and flaps marked as “A, B, C, D”; B – Transposition of flaps “ABCD” to “CADB”; C – Closure of transposed flaps, results in observed tongue lengthening (18)
Complications that can occur after any surgery include infection, bleeding, massive bleeding, fever, and pain. Due to the localization, tear of the lingual artery, damage to the lingual nerve and impaired mobility of the tongue, massive swelling of the tongue and sublingual area may also occur, leading to airway obstruction and, consequently, dyspnea; the collapse of the tongue during sleep which causes sleep apnea, re-attachment of the tongue.
PiŇõmiennictwo
1. Brzńôcka D, Brzńôcka D, Garbacz M, MicaŇā M et al.: Diagnosis, classification and management of ankyloglossia including its influence on breastfeeding. Dev Period Med 2019; 23(1): 79-87.
2. Lalakea ML, Messner AH: Ankyloglossia: Does it matter? Pediatr Clin North Am 2003; 50: 381-397.
3. Suter VG, Bornstein MM: Ankyloglossia: facts and myths in diagnosis and treatment. J Periodontol 2009; 80: 1204-1219.
4. Stan?czyk K, Ciok E, Perkowski K, Zadurska M: Ankyloglossia – literature review. Forum Ortod 2015; 11: 123-133.
5. Horton CE, Crawford HH, Adamson JE, Ashbell TS: Tongue-tie. Cleft Palate J 1969; 6: 8-23.
6. Kotlow LA: Ankyloglossia (tongue-tie): A diagnostic and treatment quandary. Quintessence Int 1999; 30: 259-262.
7. Garci?a PMJ, Gonza?lez GM, Garci?a MJM et al.: A study of pathology associated with short lingual frenum. ASDC J Dent Child 2002; 69: 59-62.
8. Ruffoli R, Giambelluca MA, Scavuzzo MC et al.: Ankyloglossia: A morphofunctional investigation in children. Oral Dis 2005; 11: 170-174.
9. Mills N, Pranksy SM, Geddes DT, Mirjalili SA: What is a tongue tie? Defining the anatomy of the in-situ lingual frenulum. Clinical Anatomy 2019; 32(6): 749-776.
10. Cummings, Fredrickson, Harker, Krause, Schuller Otolaryngology – Head and Neck Surgery. Chapter 67, 1170-1171.
11. Aleksandrowicz R, Ciszek B: Anatomia kliniczna. GŇāowy i szyi. PZWL, Warszawa 2007.
12. Kummer A: Ankyloglossia: To clip or not to clip? That’s the question. The ASHA Leader 10 2005; 17(6-7): 30.
13. Messner AH, Lalakea ML: Ankyloglossia: controversies in management. Int J Pediatric Otorhinolaryngology 2000; 54: 123-131.
14. Segan LM, Stephenson S, Dawes M: Prevalence, diagnosis, and treatment of ankyloglossia. Methodologic review. Can Fam Physician 2007; 53: 1027-1033.
15. Ballard JL, Auer CE, Khoury JC: Ankyloglossia assessment, indicence and effect of frenuloplasty on the breastfeeding. Pediatrics 2002; 100: e63.
16. Harris EF, Friend GW, Tolley EA: Enhanced prevalence of ankyloglossia with maternal cocaine abuse. Cleft Palate Craniofac J 1992; 29: 72-76.
17. Fitz-Desorgher R: All tied up. Tongue tie and its implications for breastfeeding. Practicing Midwife 2003; 6(1): 20-22.
18. Heller J, Gabbay J, O’Hara C et al.: Improved ankyloglossia correction with four – flap Z-frenuloplasty. Ann Plast Surg 2005; 54(6): 623-628.
19. Daggumati S, Cohn JE, Brennan MJ et al.: Caregiver perception of speech quality in patients with ankyloglossia: Comparison between surgery and non-treatment. Int J Pediatric Otorhinolaryngology 2019; 119: 70-74.