© Borgis - New Medicine 2/2011, s. 61-66
*Zsuzsanna Kovács1, Adrien Pigniczkiné Rigó2, Éva Szabó3, Árpád Sebestyén4, Mária Hoyer1, Emőke Fülöp1, Nóra Garamvölgyi1, Imre András Török1, Zsolt Petke1
THE PREVALENCE OF DEPRESSION AND ANXIETY IN PATIENTS WITH MALIGNANT BREAST TUMOUR
1Semmelweis University, Faculty of Health Sciences, Budapest
Head of Faculty: Prof. dr Judit Mészáros
2Eötvös Loránd University, Faculty of Pedagogy and Psychology, Budapest
Head of Faculty: Prof. dr Zsolt Demetrovics
3National Institute of Oncology, Department of Radiodiagnostics
Head of Department: Prof. dr Mária Gődény
4 Source of Health Fundation
Head of Fundation: Prof. dr Mihály Réger
Summary
Aim. The aim of the study is to examine the prevalence of depression and anxiety, and their correlation to quality of life in patients with malignant breast tumour.
Material and methods. The research has been carried out in Budapest at the Department of Radiological Diagnostics of the National Institute of Oncology. 221 women have participated in the study, all suffering from breast cancer. The Shortened Beck Depression Inventory, the Spielberger’s State-Trait Anxiety Inventory and the EORTC QLQ C30 BR23 quality of life questionnaire have been used for the research.
Results. The prevalence of clinical depression in the study-sample is 11.5% of the cases, 64.3% of the patients had mild depression (mean 12.97, std. deviation: 4.63). Concerning anxiety, 18.8% of the patients had severe and 13.6% had subclinical trait-anxiety (mean: 43.35, std. deviation: 10.31). There was a significant correlation between depression and anxiety (r=0.758, p=0.001). Both psychological disorders are reliable predictors for global, functional and symptom ratings of the quality of life, determined by the EORTC QLQ C30 BR23 questionnaire.
Conclusion. The recognition of the presence of anxiety and depression, and their medical and psychological support are crucial as they fundamentally determine the patient’s quality of life and can hugely help encourage the patient’s cooperation and evoke the fighting spirit.
Cancer is characteristically accompanied by anxiety and depression. Even if the disease is detected at an early stage and the prognosis is good, the patient will experience deep emotional pain and excessive anxiety. Cancer, despite the fact that the majority of patients are considered chronically ill, still constitutes a deadly threat.
Medical literature clearly demonstrates the presence of anxiety and depression during cancerous affections. Polsky inducted a large sample research involving more than 8,000 patients, in which he analysed the presence of depression in the most common conditions (cancer, cardiovascular conditions, chronic lung disease, arthritis, diabetes). According to his findings, patients with cancer had the highest rate of depression. He measured clinical depression in 13% of the cases (1).
Concerning the rates of psychological disorders, various data can be found. Some authors suggest that the presence of psychological distress is 50%; these are mainly adjustment difficulties accompanied by anxiety and depression (2). Derogatis studied the prevalence of psychiatric disorders in cancer patients and found psychological disorders in 47% of the cases (3). Another research team have also registered related symptoms in 50% of patients; their symptoms being hopelessness, resignation, depression, and in terminal cases an excessive desire for death (4).
Similar results can be found in women suffering from breast cancer. In a large cohort of 4,496 patients the prevalence of depression was estimated to be around 52% (5).
Numerous authors have registered similar symptoms of psychological morbidities, such as anxiety, depression, stress, distress, (5, 6, 7), while others reported difficulty in adjustment and decreased social interactions (8). Such responses may arise from the fear of pain, fear of recurrence, and from the unpleasant treatment side-effects (9).
A recent study suggests however that the number of patients approaching threshold for depressive and anxiety disorders is close to 50% in the first year after diagnosis, dropping rapidly in the second year to 25% and sustaining a further gradual decrease over the five-year study period to 15% in the fifth year (10). A review of 37 studies on the epidemiology of major depression in women with breast cancer suggested a rate of 10% to 25% (6). Close correlation is found between depression and anxiety: about one third (35%) of the patients reported anxiety or depression, or both, which did not significantly change over five years of follow up (11). This wide variation in rates of psychological disorders may be attributed to methodological differences across studies (cross-section researches, experimental group-studies). The stage of the illness and the circumstances of the research may also influence the outcome, in the same way as the use of different tools and different diagnostic criteria or even the focus of the study (6, 7, 12, 13).
Concerning the subject, only a few studies have been conducted in Hungary. There has been a national representative study carried out as a part of the Hungarostudy 2002, surveying the physical and mental health of the adult population of Hungary, and the relation between health indicators and the environmental, social and economic background. According to their research results the incidence of clinically significant depression rate in women affected with cancer was 28.5%, while in men it showed 27.4%. (14) A study conducted in Transylvania examined the prevalence of depression in correlation with numerous factors (demographic, medical, lifestyle and psychosocial). The results suggested that about 50% of the inpatients questioned suffered from clinical depression (15). Riskó basing on her clinical experience, reports similar results (16).
The appearance and the degree of anxiety and depression are correlated with numerous factors: type of cancer, its seriousness, chances of curability, the impact of symptoms (associated with various treatments) on the quality of patient’s life (10), the patient’s social support network, psychosocial background, length of time passed since the diagnosis, but even the characteristics of the premorbid personality, and the patient’s way of coping (6, 13, 17); all factors influencing the appearance of emotional distress, depression and anxiety. On the other hand, the high levels of anxiety observed in patients can influence their life, their condition and the management of their illness in many different ways. There is a so-called Kindling phenomenon which is characteristically present in patients: it is typical that before each control visit patients feel more uneasy, uncertain; anxiety and depression become more prominent, the same ways as deterioration may appear after repeated surgical interventions, treatments or a relapse (18). The prevalence of depression has a very strong deteriorative affect on the quality of life of the patient, puts a burden on the patient’s social relations and, at the same time, interferes with her/his active coping attitude and increases the chances of the recurrence (19). Kepplinger and Steige, in their comprehensive study of development of family and social relations, also researching the levels and characteristics of distress of the relatives, have come to a conclusion that the levels of stress, anxiety and depression in the patient’s relatives are similar to those of the patient with cancer (20).
The recognition of the presence of anxiety and depression, and their medical and psychological support are crucial. They fundamentally determine the patient’s quality of life, and can hugely help encourage the patient’s cooperation and evoke the fighting spirit.
METHODS
In 2009-2010 a comprehensive psycho-oncology research was conducted, intending to develop a complex, complementary rehabilitation method in addition to the traditional medical cancer treatment, in order to improve the health and quality of life, strengthen coping abilities, and increase the life expectancy of patients suffering from cancer. In the first step of this study, cross-sectional studies have been carried out, and a randomized sample has been introduced to a complex, psychosocial intervention program.
The presented study explores some of the outcomes of the cross-sectional research:
– the prevalence of anxiety and depression,
– the correlation of anxiety and depression to quality of life.
The assessed sample
The sample involved 221 female patients suffering from malignant breast tumour (C50), who agreed to cooperate and who at the time were actually undergoing a treatment for active cancer. The research was carried out in Budapest at the Department of Radiological Diagnostics of the National Institute of Oncology, with an official approval from the Ethical Committee of the Institute.
We used an eight-page self-assessment form filled in by each patient individually, taking about 50 minutes in each case. The questionnaires have been completed within the frames of the mammographic investigation.
Among the demographic variables the following have been included: age, level of education, marital status, and the number of children. Age division was between 30 and 68, with the average of 52.8 years. 35% of the patients were younger than 50; 46% were between 50 and 60, and 19% of them were over age of 60. Concerning qualifications, 45% of them had higher, 38% had secondary, while 16% had elementary or vocational education (2 patients did not answer this question). Concerning their marital status, most of the patients were married or in a stable relationship (72%), 14% of them were divorced, 10% widowed and 4% single. 12% of the patients had no children, 28% had one, 49% of them had two, 10% had three and 10% of them had four children. The time period since the diagnosis of the condition was 2.48 year in average (std. deviation: 1.17). The time period since the surgical intervention was 2.26 year in average (std. deviation: 1.11).
APPLIED METHODOLOGIES
Shortened Beck Depression Inventory BDI
The Shortened Beck Depression Inventory BDI for measuring the symptoms of depression has been administered. The above questionnaire had been assessed on Hungarian sample, has good psychometrical parameters and its reliability has a high degree. The shortened version has nine items (e.g. ‘I lost all interest in others) measured with a Likert Scale 0-3 (0 – not characteristic at all, 1 – somewhat characteristic, 2 – characteristic, 3 – very much characteristic). According to the resulting points (0 – minimum, 60 – possible maximum points) the following categories have been defined:
0-9: not depressed, 10-18: mild symptoms of depression, 19-25: moderate depression, above 26 points: severe depression. According to clinical validity the borderline for clinical depression is 19 points (21).
The reliability of the questionnaire on the sample proved adequate (Cronbach-alpha: 0,89).
Spielberger’s State-Trait Anxiety Inventory
The Spielberger’s State-Trait Anxiety Inventory STAI-T measures the levels of trait-anxiety. The questionnaire consisted of 20 questions. The answers were recorded on a four-point Likert Scale. The choice of answers is as follows: 1 – hardly ever, 2 – sometimes, 3 – often, 4 – almost always. Minimum 20, maximum 80 points were achievable. Standard scores in female population: mean: 45.37; std. deviation: 7.97 (22). As the original questionnaire does not include standard limit values, the definitions used in a previous Hungarian research have been applied: 1. STAI-T < 48: no anxiety, 2. STAI-T > 52: severe clinical anxiety, 3. STAI-T = 48-52: mild or subclinical level trait-anxiety (23, 24).
In the sample the Cronbach-alpha coefficient is 0.89.
EORTC QLQ C30 BR23
The European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ C30 ) is one of the most approved and most frequently used quality of life questionnaires in international research practice. It consists of 30 items divided into 3 scales: 1) Global quality of life, 2) Functional quality of life and 3) Symptom-related quality of life.
The global health status (quality of life) is assessed by two questions: “How would you rate the overall state of your health last week?” and “How would you rate the general quality of life last week?” The answers have to be indicated on a 1 to 7 scale, varying from “1 – very bad” to, “7 – excellent”. The functional scale (quality of life) assesses: physical functioning, role functioning, emotional functioning, cognitive functioning and social functioning. The symptom-related quality of life scales measure: fatigue, nausea, pain, dyspnoea, insomnia, loss of appetite, constipation, diarrhoea, and financial difficulties. The answers are recorded in a four-point Likert-scale: 1 – not at all characteristic, 2 – somewhat characteristic, 3 – characteristic, 4 – strongly characteristic. A breast cancer-specific additional module, the QLQ-BR23 was used for the research. This module incorporates 8 functional and 15 symptom scales (25, 26).
The European Organisation for the Research and Treatment of Cancer (EORTC), a non-profit international cancer research organisation, has made the Hungarian translation of the test available. These tests have previously been used only a few times in Hungary; therefore their validation on a national sample is also one of the objects of the present study.
Applied Statistical Methods
Our research is cross-sectional, descriptive; we conducted multivariable statistical calculations; assessed the core results of depression, anxiety and quality of life; analysed the means, the standard deviation and the correlation between variables; performed a calculation on correlation and linear regression aligning to the characteristics of the variables. The SPSS 18 software package has been used for the analysis.
RESULTS
The Prevalence of Depression and Anxiety
The average score on the Shortened Beck Depression Inventory was 12.97 points, the standard deviation: 4.63.
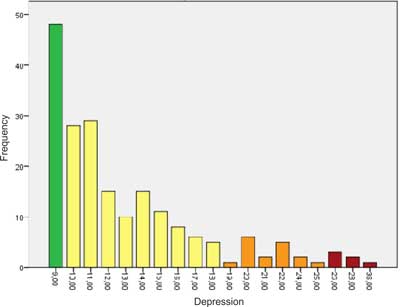
24.2% of the patients participating in the research were not characterised by symptoms of depression (scores 0-9). Mild or subclinical depression was present in 64.3% of the cases (scores 10-18); 11.5% of the patients reached the limits for clinical depression (scores above 19 points) of which 8.5% had moderate while 3% severe (clinical) depression (fig. 1).
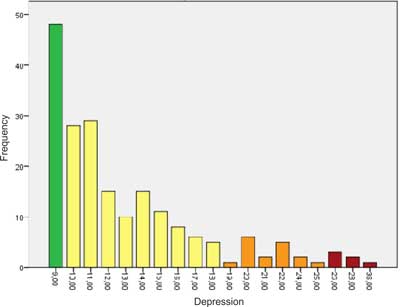
Fig. 1. Depression Score Distribution.
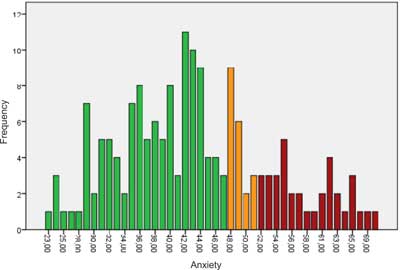
The average scores for anxiety were: 43.35, std. deviation: 10.31. The results showed similar distribution to the average population (fig. 2).
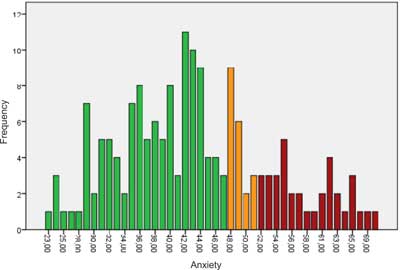
Fig. 2. Anxiety Score Distribution.
Table 1. Correlations between depression, anxiety and the quality of life.
| EORTC Global QL | EORTC Functional QL | EORTC Symptom QL | BR23 Functional QL | BR23 Symptom QL |
| Depression | -0.55 | -0.73 | 0.69 | -0.23 | 0.59 |
| Anxiety | -0.6 | -0.67 | 0.55 | -0.28 | 0.53 |
67.6% of the participating patients were not characterised by trait-anxiety (below 48 points), while 13.6% of them had mild (from 48 to 52 points) and 18.8% severe anxiety (above 52 points). We observe a close relationship between the scores of anxiety and depression, the Spearman correlation coefficient is significant: r = 0.758 (p = 0.001).
Correlation between anxiety and depression and the quality of life
An important aspect of the present research was to explore how depression and anxiety affect the patient’s quality of life, and to what degree they are predictors of the quality of life. Analysing the regressive coefficients, one comes to a conclusion that the quality of life shows close correlation with all three aspects, namely the global, the functional and the symptom-related quality of life. All three correlation coefficients are statistically significant (p = 0.000).
DISCUSSION
Depression and anxiety disorders demonstrate a significantly damaging impact on health and cause deterioration in quality of life. If they are accompanied by chronic conditions, their effect can be significantly multiplied. More than one tenth of the studied samples showed depression reaching the clinical borderline, and nearly two thirds of the patients experienced mild (subclinical) symptoms of depression. The results concerning anxiety showed mild to severe trait-anxiety in one third of the assessed patients.
The outcomes of the research have confirmed the clinical observations recorded by Riskó (16) and relate to similar medical sources (7). A close relationship between scores of anxiety and depression has been found, also confirmed by clinical experience (10).
The cross-sectional nature of the research does not allow confirmations concerning the cause and effect relationship. Therefore, according to the results we can establish that an anxious, hopeless, depressed state has been demonstrated to have an impact on the patient’s quality of life. Similarly to the outcomes of other researchers (6, 7), the present research has also found a close correlation between the scores of symptom-related, global and the functional quality of life, assessed by the EORTC quality of life questionnaire. Both depression and anxiety are reliable predictors of the quality of life. Psychological distress has a significant effect on the physical sense of well-being, as well as on the degree of comfort and the sensitivity to physical symptoms. And vice versa, a strong sense of physical discomfort can also intensify a depressed, low emotional state. There are studies confirming that pain and general physical complaints of non-psychiatric origin can significantly increase the scores of the depression scale. These are non-specific symptoms of depression, like sleep disorder, hypochondria and fatigue (21), therefore organising further investigations analysing the complexity of these correlations would be valuable. When examining the relationship between the areas defined by functional quality of life scales (physical limitations, role, emotional, cognitive and social functioning) and anxiety and depression, significant correlations can be identified. There is evidence that depression impairs cognitive abilities, narrows social functioning and generally determines and affects the global quality of life (7,8).
CONCLUSION
Based on the results, it is considered rather important and highly recommended to monitor mental distress in patients with cancer routinely on a regular basis. With the use of self-assessment questionnaires quick, simple and reliable results on the psychological state of the patient can be obtained. Apart from the risk of clinical level distress, it is very important to also pay attention to subclinical categories.
Early recognition of the presence of anxiety and depression, and their medical and psychological support are crucial as they fundamentally determine the patient’s quality of life, can hugely help encourage the patient’s cooperation and evoke the fighting spirit.
We would like to thank the co-workers of the Department of Radiodiagnostics (National Institute of Oncology, Budapest) for distributing the questionnaires to the patients.
Special thanks to Prof. Dr Sándor Eckhardt for supervision and professional advises.
Piśmiennictwo
1. Polsky D, Doshi JA, MarcusS et al.: Long-Term Risk For Depressive Symptoms After A Medical Diagnosis. Archives Of Internal Medicine 2005;165: 1260-1266. 2. Massie MJ: Prevalence of depression in patients with cancer. JNCI Monographs, 2004; 32: 57-71. 3. Derogatis LR, Morrow GR, Fetting J Et al.: The prevalence of psychiatric disorders among cancer patients. Journal of the American Medical Association 1983; 249: 751-757. 4. Breitbart W, Rosenfeld B, Pessin H Et al.: Depression, Hopelessness, and Desire for Hastened Death in Terminally Ill Patients With Cancer. Journal of the American Medical Association 2000; 284: 2907-2911. 5. Zabora J, Brintzenhofe K, Curbow B et al.: The prevalence of psychological distress by cancer site. Psycho-oncology 2001; 10(1): 19-28. 6. Fann J: Major depression after breast cancer: a review of epidemiology and treatment. General Hospital Psychiatry 2008; 30 (2): 112-26. 7. Reich M, Lesur A, Perdrizet-Chevallier C: Depression, quality of life and breast cancer: a review of the literature. Breast Cancer Research and Treatment 2008; 110(1): 9-17. 8. Vos PJ, Visser AP, Garssen B et al.: Effects of delayed psychosocial interventions versus early psychosocial interventions for women with early stage breast cancer. Patient Education and Counseling 2006; 60(2): 212-221 9. Reddick BK, Nanda JP, Campbell L et al.: Examining the influence of coping with pain on depression, anxiety, and fatigue among women with breast cancer. Journal of Psychosocial Oncology 2005;23(2-3): 137-57. 10. Burgess C, Cornelius V, Love S et al.: Depression and anxiety in women with early breast cancer: five year observational cohort study. BMJ 2005; 330(7493): 702-5 . 11. Hopwood P, Sumo G, Mills J et al.: The course of anxiety and depression over 5 years of follow up and risk factors in women with early breast cancer: Results from the UK Standardisation of Radiotherapy Trials (START). Breast 2010;19 (2): 84-91. 12. Chochinov HM, Wilson KG, Enns M, Lander S: Prevalence of depression in the terminally ill: effects of diagnostic criteria and symptom threshold judgments. The American Journal of Psychiatry 1994; 151: 537-40. 13. Baider L, Andritsch E, Uziely B et al.: Effects of age on coping and psychological distress in women diagnosed with breast cancer: review of literature and analysis of two different geographical settings. Critical Reviews in Oncology/Hematology 2003; 46(1): 5-16. 14. Dégi L. Csaba: Pszichoszociális kockázati tényezők szerepe a daganatos megbetegedésekben, 2008. [In:] Kopp, M. (szerk.), Magyar lelkiállapot (pp. 557-568). Semmelweis Kiadó, Budapest . 15. Dégi L. Csaba: A depresszió prevalenciája az onkológiai ellátásban Erdélyben. Kórházban kezelt daganatos betegek körében végzett multicentrikus felmérés Beck-féle depresszió önértékelő kérdőívvel, Erdélyi pszichológiai szemle 2009; 4, 299-321 16. Riskó Á: Bevezetés az onkopszichológiába. Animula, Budapest 1999. 17. Barsevick AM, Sweeney C, Haney E, Chung E: A systematic qualitative analysis of psychoeducational interventions for depression in patients with cancer. Oncology Nursing Forum 2002; 29(1): 73-87. 18. Veres Zs: A daganatos betegségek lehetséges pszichológiai és pszichiátriai tünetei, 2006. [In:] Horti, J.,Riskó, Á. (szerk.), Onkopszichológia a gyakorlatban (pp. 203-209), Medicina, Budapest. 19. Greer S, Morris T, Pettingale KW: Psychological response to breast cancer: effect on outcome. Lancet 1979; ii: 785-7. 20. Kepplinger J, Steige R: Psychosoziale Belastungen und soziale Unterstützung bei Partnern von Krebskranken. [In:] Kállai J, Varga J, Oláh A (szerk): Egészségpszichológia a gyakorlatban, 2007, Medicina, Budapest. 21. Rózsa S, Szádóczky E, Füredi J: A Beck Depresszió Kérdôív rövidített változatának jellemzôi hazai mintán. Psychiatria Hungarica 2001; 16: 384-402. 22. Sipos K, Sipos M, Spielberger CD: A State-Trait Anxiety Inventory (STAI) magyar változata. [In:] Mérei F, Szakács F (szerk.): Pszichodiagnosztikai vademecum I/2. Nemzeti Tankönyvkiadó, Budapest 1994; 123-148. 23. Spielberger CD, Gorsuch RL, Lushene RE: Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press 1970; Palo Alto, CA. 24. Stauder A, Kovacs M: Anxiety symptoms in allergic patients: Identification and risk factors. Psychosom Med 2003; 65, 816-823. 25. Aaronson NK, Ahmedzai S, Bergman B et al.: The European Organisation for Research and Treatment of Cancer QLQ-C30: a uality of life instrument for use in international clinical trials in oncology. Journal of National Cancer Institute 1993; 85, 365-367. 26. Aaronson NK, Ahmedzai S, Bullinger M et al.: The EORTC Core Quality of Life Questionnaire: interim results of an international field study. [In:] Osoba D. (ed.), Effect of Cancer on Quality of Life (Boca Raton, FL: CRC Press) 1991; pp. 185-203.