© Borgis - New Medicine 4/2011, s. 116-119
Małgorzata Dębska, *Magdalena Frąckiewicz, Mieczysław Chmielik
The orbital abscess in the data of Paediatric Otolaryngological Clinic of Warsaw Medical University in 2005-2011
Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Prof. Mieczysław Chmielik, MD, PhD
Summary
Introduction. Complications can occur as a consequence of both acute and chronic sinusitis. Most frequently complications are caused by acute ethmoiditis or frontal sinusitis. The complications of paranasal sinusitis are divided into intraorbital, intracranial and osteomyelitis. The children with complications of paranasal sinusitis require hospitalization, treatment with combined intravenous antibioticotherapy and often surgical treatment.
Aim. The analysis of patients treated surgically for orbital complications of paranasal sinusitis.
Material and methods. The research included children that were operated for orbital complications of paranasal sinusitis in Paediatric Otolaryngological Clinic of Warsaw Medical University between January 2005 and February 2011. The data were collected retrospectively on basis of medical documentation.
Results. In the period 2005-02.2011 in Paediatric Otolaryngological Clinic of Warsaw Medical University 27 children were operated due to orbital complications of rhinosinusitis. The procedures that were performed most frequently were: ethmoidectomy with or without maxillary sinuses puncture and drainage of the abscess.
Discussion. In children complications of paranasal sinusitis occur more frequently than in adults. The localization of the inflammation within the eyeball (preseptal or retroseptal) plays an important role in deciding about the method of treatment. Surgical treatment should be carry out in following cases: subperiosteal abscess, orbital abscess or each case of deterioration of visual acuity or lack of improvement after exact preservative treatment.
INTRODUCTION
The paranasal sinusitis can induce very serious complications. They can occur as a consequence of both acute and chronic sinusitis. Most frequently complications are caused by acute ethmoiditis or frontal sinusitis since topographical conditions are conductive to spreading the inflammation through veins, arteries, lymphatic vessels and also directly from dehiscences in bones (1-3). In children complications of paranasal sinusitis occur more frequently than in adults (4).
The complications of paranasal sinusitis are divided into intraorbital, intracranial and osteomyelitis. The intraorbital complications are divided (according to Chandlera) into (1, 3, 4):
– inflammatory oedema of the orbit,
– orbital cellulitis,
– orbital cellulitis with subperiosteal abscess,
– orbital abscess,
– cavernous sinus thrombophlebitis.
The symptoms of intraorbital complications of paranasal sinusitis include local symptoms, such as: eyesore, oedema and erythema of the orbit (fig. 1), blepharophimosis, restriction of eyeball movements, exophtalmus, deterioration of visual acuity and even blindness and general symptoms, such as: headache, fever, weakness, loss of appetite, apathy (1, 2, 5).

Fig. 1. Clinical representation of complication of acute paranasal sinusitis.
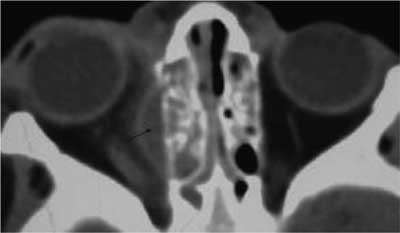
Each case of complications of paranasal sinusitis requires administration of immediate diagnostics, including paediatric, laryngological examination with evaluation of the orbit mobility and visual acuity, ophthalmological and neurological consultation. Immediate treatment is needed since the inflammation proceeds urgently and that can cause intracranial complications, sepsis or patient’s death. The computer tomography is a fundamental radiological examination in case of complications of paranasal sinusitis (1, 2, 6, 7) (fig. 2).
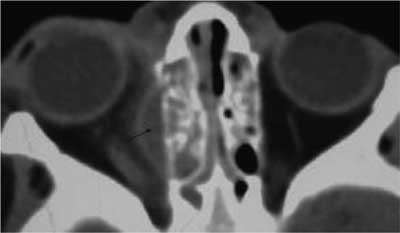
Fig. 2. Representation of complications of an acute paranasal sinusitis in CT.
The children with complications of paranasal sinusitis require hospitalization, treatment with combined intravenous antibioticotherapy and often surgical treatment. When deciding about the method of treatment, the location of inflammation is very important. The orbital septum is a membrane that originates from the orbital periosteum and inserts into the anterior surfaces of the tarsal plates of the eyelids, it separates the superficial eyelid from the deeper orbital structures. The preseptal cellulitis, the inflammation that is located anteriorly to the orbital septum, demands preservative treatment with topical nasal decongestants. Complications that are located posteriorly to the orbital septum demand combined treatment: preservative and most frequently surgical (1, 5, 6).
AIM
The particular analysis of patients treated surgically due to orbital complications of paranasal sinusitis.
MATERIAL AND METHODS
The research included 27 children that were operated due to orbital complications of paranasal sinusitis. The children were hospitalized in Paediatric Otolaryngological Clinic of Warsaw Medical University between January 2005 and February 2011. In the analyzed group there were 17 boys and 10 girls at the age from 2 months to 13 years and 7 months (mean age 6 years and 1 month). The data were collected retrospectively on the basis of medical documentation.
RESULTS
Since January 2005 and February 2011 in Paediatric Otolaryngological Clinic of Warsaw Medical University there were 124 children with acute rhinosinusitis hospitalized, 51 children were diagnosed with orbital complications and 27 were operated due to that reason.
The patients were estimated with regard for duration of symptoms before hospitalization, physical examination on admission, inflammatory parameters. In the majority of cases computed tomography of the sinuses with the assessment of the orbits was performed. At qualification to surgical treatment we took the results of physical examination, response for previous treatment and result of CT into consideration.
The average duration of symptoms before hospitalization was 4 days. All patients in physical examination presented a different degree of oedema and erythema of the eyelids. In 19 cases (70.4%) there were limitations of mobility of the orbit and exophtalmus stated. In other 8 cases the clinical condition was deteriorating in spite of the treatment and also the limitations of mobility of the orbit and exophtalmus occurred.
The majority of patients on admission presented increased inflammatory parameters, average results were as following: leukocytes – 15.4 x 103/uL (n: 4.5-13.0), OB – 70 mm/1 hour (n: 3-15), CRP – 6 mg/dL (n: 0-1).
In analyzed group of 27 patients, in 5 cases (18.5%) CT was not performed before the surgical procedures because the inflammatory lesions were spreading and also protrusion and mobility of the orbit were worsening. The results of CT, depending on described lesions were divided into 5 groups:
group I – haziness of the paranasal sinuses, without oedema of the soft tissues of the orbit, without signs of the abscess,
group II – infiltration, enhancement of the medial rectus muscle,
group III – oedema of the soft tissues of the orbit, with dislocation of the medial rectus muscle,
group IV – enhancement and dislocation of the medial rectus muscle, distraction of bones between the orbit and ethmoid sinus,
group V – bubble of the air inside the orbit (table 1).
Table 1. The distribution of the patients in each group.
| CT group | Amount of patients /% |
| group I | 6/22.2% |
| group II | 6/22.2% |
| group III | 6/22.2% |
| group IV | 2/7.5 % |
| group V | 2/7.5 % |
According to bacteriological aetiology we received the following results – table 2.
Table 2. Most frequent bacterial aetiology in our research.
| Type of patogen | Amount |
| Streptococcus pyogenes | 3 |
| Haemophilus influenzae | 3 |
| Streptococcus pneumoniae | 2 |
| mixed infection: Haemophilus influenzae, Streptococcus pneumoniae, Corynebacterium | 1 |
| Staphylococcus ureus | 1 |
| Staphylococcus spp. coagulase (-) | 1 |
| Streptococcus asaccharolyticum | 1 |
| Streptococcus constellatus | 1 |
| Bacteroides distasonis | 1 |
| Staphylococcus epidermidis | 1 |
| no growth | 12 |
In intra-operative assessment the authors stated: 9 cases of orbital abscesses, 7 cases of subperiosteal abscesses, 11 cases of purulent lesions in ethmoid sinuses and inflammation of soft tissues of the orbit.
In 17 cases (77.3%) the authors stated correlations of pathologies detected in CT and in intra-operative findings. In 3 cases (13.6%) the result of CT suggested orbital abscess but there was no confirmation intra-operatively. In 2 cases (9.1%) there were no abscess described in the CT result however such a lesion was stated intra-operatively (table 3).
Table 3. Specification of intra-operative findings, CT results, laboratory tests and duration of hospitalization.
| Intra-operative lesions | Amount | CT group/amount of patients | Laboratory tests (average) | The average duration of hospitalization |
| Orbital abscess | 9 | group II – 2
group III – 2
group IV – 2
group V – 2
no CT – 1 | L – 15,2 x 103/uL
OB – 64 mm/1 hour
CRP – 5.7 mg/dL | 10 |
| Subperiosteal abscess | 7 | group I – 3
group II – 1
group III – 3 | L – 16,7 x 103/uL
OB – 78 mm/1 hour
CRP – 3.7 mg/dL | 7 |
| Purulent lesions in ethmoid sinuses and inflammation of soft tissues of the eyeball | 11 | group I – 3
group II – 2
group III – 2
no CT – 4 | L – 14,8 x 103/uL
OB – 69 mm/1 hour
CRP – 7,2 mg/dL | 9 |
Patients were treated with intravenous, combined antibioticotherapy for 6-14 days: in 24 cases with cephalosporin the II generation (Biofuroxim) and Clindamycin, in 3 cases with cephalosporin the III generation (Biotraxon) and Clindamycin, afterwards they were treated with oral complementary antibioticotherapy (cephalosporin the II generation). Topical treatment was also administered: ophthalmic drops (Amikacin or Gentamycin) in 11 cases and topical nasal decongestants (Oxymetazoline) in all cases. The average duration of hospitalization was 9 days.
DISCUSSION
In children complications of paranasal sinusitis occur more frequently than in adults. We can also observe that inflammation spreads more quickly and the condition of the patient can deteriorate immediately. Therefore it is very vital to make a right diagnosis and introduce adequate treatment. Unnecessary delay of treatment can lead to irreversible consequence, such as blindness even up to 10% of patients with orbital complications of sinusitis (5, 6).
The appearance of exophtalmus, limitations of the orbit mobility or deterioration of visual acuity is alarming and can suggest subperiosteal or orbital abscess. However Rahbar et al. have observed that the oedema and erythema of the eyelids can be the only manifestation of subperiosteal abscess (5, 6). Therefore the decision about the method of the treatment (preservative or surgical) cannot be made only on the basis of physical examination with assessment of the protrusion and mobility of the orbit. Among radiological examination computed tomography is the most vital, NMR is less useful. NMR can be rather use in differentiation in cases of neoplastic or traumatic lesions. In CT we are able to assess the size and location of the lesions, relations to the ocular muscles and optic nerve. Despite the correlation between radiological images and intra-operative findings is not complete, CT is a fundamental radiological examination in diagnostics of orbital complications of sinusitis in children (4, 8).
The localization of inflammation within the eyeball plays an important role in deciding about the method of treatment. The complications located anteriorly to the orbital septum demand an intense, intravenous antibioticotherapy with topical, nasal decongestants. The complications located posteriorly to the orbital septum demand a combined treatment: an intense, intravenous antibioticotherapy with topical, nasal decongestants and in most cases surgical procedures. However some authors advocate an initial trial of intravenous antibiotics despite radiographic evidence of subperiosteal abscess. Others claim the presence of a subperiosteal abscess to be an absolute indication for surgical drainage (6, 9, 10). On the basis of our observation we claim that patients with proptosis and limitations of the orbit mobility in every case of deterioration of visual acuity demand surgical treatment, with ethmoidectomy and drainage of purulent collection despite negative result of CT. Whereas patients without proptosis, limitations of the orbit mobility without deterioration of visual acuity with radiographic evidence demand systematic control of visual acuity and mobility of the orbit and surgical drainage when above mentioned symptoms are present. In our research there were in 3 cases evidence of subperiosteal abscess in CT but no such lesions intra-operatively.
CONCLUSIONS
1. The intraorbital complications of paranasal sinusitis should be treated with combine intravenous antibiotics for 7-10 days and complementary oral antibiotics for 14-21 days.
2. The clinical examination is a determining factor in qualification for surgical treatment, proptosis and limitations in mobility of the orbit, deterioration of visual acuity are the most vital symptoms.
3. Computed tomography is a valuable complementary examination in qualification for surgical treatment of complications of paranasal sinusitis.
Piśmiennictwo
1. Chmielik M (red.): Otolaryngologia dziecięca. 2001, 69-72. 2. Janczewski G (red.): Otolaryngologia praktyczna. 2005, tom I, 340-349. 3. Gryczyńska D (red.): Otolaryngologia dziecięca. 2007, 267. 4. Velasco e Cruz AA, Demarco RC, Pereira Valera FC et al: Orbital complications of acute rhinosinusitis: a new classification. Rev Bras Otorrinolaringol 2007; 73(5): 684-8. 5. Rudloe TF, Harper MB, Prabhu SP et al.: Acute Periorbital Infections: Who Needs Emergent Imaging? Pediatrics 2010; 125(4): 719-26. 6. Rahbar R, Robson DC, Petersen RA et al.: Management of Orbital Subperiosteal Abscess in Children. Arch Otolaryngol Head Neck Surg 2001; 127: 281-286. 7. Pelton RW, Smith ME, Patel BCK, Kelly SM: Cosmetic Considerations in Surgery for Orbital Subperiosteal Abscess in Children Arch Otolaryngol Head Neck Surg 2003; 129: 652-655. 8. Clary RA, Cunningham MJ, Eavey RD: Orbital complications of acute sinusitis: Comparison of computed tomography scan and surgical findings. Ann Otol Rhinol Laryngol 1992; 101: 598-600. 9. Tanna N, Preciado DA, Clary MS, Choi SS: Surgical Treatment of Subperiosteal Orbital Abscess. Arch Otolaryngol Head Neck Surg 2008; 134(7): 764-67. 10. Goodyear PWA, Firth AL, Strachan DR, Dudley M: Periorbital Swelling: the important distinction between allergy and infection Emerg Med J 2004; 21: 240-242.