© Borgis - New Medicine 4/2011, s. 122-124
Małgorzata Dębska, *Eliza Brożek-Mądry, Anna Gorzelnik, Monika Jabłońska-Jesionowska, Mieczysław Chmielik
Management of the parapharyngeal space infection – diagnostic and therapeutic issues
Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Prof. Mieczysław Chmielik, MD, PhD
Summary
Introduction: Pathology leading to infection in the parapharyngeal space is associated with different conditions beginning with upper respiratory tract infections. Therapeutic possibilities include conservative (pharmacological) and surgical treatment.
Aim: The aim of the presented study was to analyze the management of parapharyngeal space infections in our department.
Material and methods: The group of children who underwent conservative, pharmacological treatment included three boys at age 7, 12 and 14 months and two girls at age 18 months and 12 years. Surgical drainage was performed in three girls at age 3 (2 patients) and 12 years.
Results: Patients treated only pharmacologically did not meet any complications or relapse of the disease.
Conclusions: Conservative treatment can be applied in patients without complications threatening patients’ life, when improvement of the general condition is observed with normalization of the body temperature and reduction of inflammatory parameters in 24-48 hours.
INTRODUCTION
Pathology leading to infection in the parapharyngeal space is associated with different conditions beginning with upper respiratory tract infections and otitis media through posttraumatic changes including foreign bodies and frequently forgotten tuberculosis. However, most cases are strictly connected with cervical lymphadenitis (1). Parapharyngeal space infections may have a fatal course due to respiratory distress or spread of the infection to other areas.
Therapeutic possibilities in parapharyngeal space pathology refer to anatomic division of the discussed space into prestyloid compartment containing mainly fatty tissue and retrostyloid compartment with neuro-vascular bundle. Infection in the prestyloid compartment may lead to liquefaction of the fatty tissue and pus formation that can easily penetrate in loose fibrous tissue to adhering spaces. Such location of the disease requires surgical drainage. On the other hand inflammation in the retrostyloid compartment is mainly connected with lymphadenitis and their fibrous capsule serves a better separation from surrounding tissues allowing introducing pharmacological treatment and watchful observation. Surgical treatment of retrostyloid abscess is reserved for patients in poor general condition, patients with respiratory distress due to mass effect and if there is no improvement after intravenous antibiotic therapy (1).
AIM
The aim of the presented study was to analyze the management of parapharyngeal space infections in our department.
MATERIAL AND METHOD
A retrospective analysis was conducted including eight patients diagnosed and treated in Pediatric Otolaryngology Department of Warsaw Medical University between 2005 and 2010 due to infection of the parapharyngeal space. The group of children who underwent conservative, pharmacological treatment included three boys at age 7, 12 and 14 months and two girls at age 18 months and 12 years. Surgical drainage was performed in three girls at age 3 (2 patients) and 12 years.
Patients treated pharmacologically presented following symptoms prior to admission: upper respiratory tract infection accompanied by temperature approx. 38°C for 4-6 days, anorexia and dysphagia, irritability and anxiousness. Patients’ history also revealed prior treatment with amoxicillin or fespiride. Physical examination performed at admission showed lymph nodes enlargement in all patients, impaired cervical mobility in two cases, trismus in one patient, enlargement and significant medial displacement of palatine tonsil on one side in four patients and ptosis on the contralateral side in one patient. Laboratory testing on admission showed elevated white blood cells count (19.7-40.2 x 103/mm3), elevated inflammatory parameters: C-reactive protein at level 8.5-53 mg/dl, erythrocyte sedimentation (ES) at 42-88 mm/h and anemia in four younger patients.
All patients underwent differential diagnosis towards toxoplasmosis, mononucleosis, cytomegaly and boreliosis and showed negative results. The diagnostic path reached radiologic tools such as computed tomography with contrast and magnetic resonance imaging and also ultrasonography was performed repeatedly to monitor the course of disease. Contrasted computed tomography in one patient showed well separated fluid compartment sized 12 x 12 mm with inflammatory oedema and the abscess was observed medially and anteriorly to the neuro-vascular bundle, in another patient the area pathologically changed sized 26 x 26 mm in parapharyngeal space. Magnetic resonance performed in one patient revealed pathologically changed lymph node located between antero-medial wall of internal carotid artery and capitis longus muscle, surrounded with the fluid margin. The last two patients were followed just with ultrasonography.
Pharmacological treatment was supplied intravenously with combined antibiotic therapy. Conjugated therapy included beta lactam antibiotics and lincosamides. Two patients received ceftriaxone, one patient cefotaxime, one patient cefuroxime, and one patient amoxicillin with clavulonic acid; additionally all patients received clindamycin. Hospital stay and intravenous treatment lasted 10-14 days until the symptoms withdrew and the normalization of laboratory testing was accomplished. Oral antibiotic treatment was continued until the regress of inflammatory changes in the parapharygeal space in ultrasonography was observed. Patients treated only pharmacologically did not meet any complications or relapse of the disease.
Patients treated surgically presented with different length of disease prior to admission to the Department and oscillated between few days and few weeks. Among reported symptoms there were upper respiratory tract infection with temperature to 39°C and cervical lymph nodes enlargement.
In one patient, cervical lymph nodes were enlarged in packages, stiff, hardly movable and painless, suggesting neoplasmatic process. Additional laboratory findings revealed very high erythrocyte sedimentation (ES) 120 mm/h. Treatment prior to admission included amoxicillin with clavulonic acid. Other reported symptoms were sore throat, night sweats and skin itching over the enlarged lymph nodes. Physical examination revealed cervical asymmetry, palatine arches asymmetry and enlarged cervical lymph nodes in ultrasonography. Hospital pharmacological treatment included ceftriaxone, amikacin and metronidazole, eventually changed to cefuroxime and clindamycin (additionally fluconasole). Patient suspected of neoplasmatic disease had a biopsy of the lymph node performed. The biopsy showed purulent process within the node with negative culture and without neoplasmtic changes in pathological examination, with reactive changes in trepanobiopsy of bone marrow and with normal marrow in mielogram.
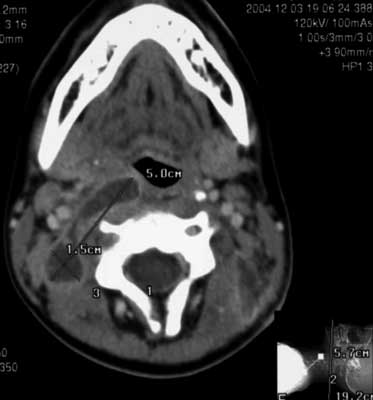
Other patients had erythrocyte sedimentation 82 and 89 mm/h with white blood cells level 9,4 and 16.0 thousand/μl. Additionally neck ultrasonography was performed and a suspicion of abscess was described. Computed tomography performed in all patients revealed polycystic fluid compartment (fig. 1A, B) in parapharyngeal space either in retrostyloid and prestyloid compartment. Differential diagnosis included immunoenzymatic testing and antibodies (class IgG) against EBV were found and the first described patient had present IgM against Borrelia burgdorferi.
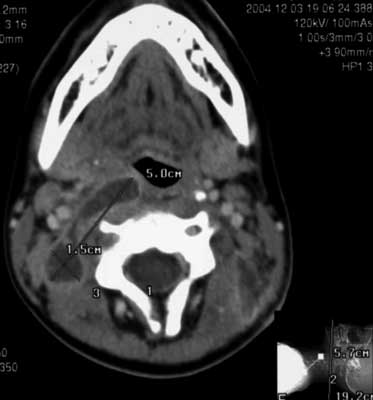

Fig. 1A, B. Policystic abscess in the parapharyngeal space (CT with contrast).
Under general anesthesia, with the help of ultrasonography the puncture and drainage were performed in external approach in all patients. Culture of the pus was positive in one patient and it was Bacteroides fragilis. Passive drainage after the surgical procedure was continued for 3-5 days. Similarily to the patients treated only pharmacologically, the antibiotic treatment was continued until normalization of the inflammatory response in laboratory assessment and the resolution of the symptoms.
DISCUSSION
The management in inflammatory conditions of the parapharyngeal space requires elaborate assessment of patient condition including symptoms, level of inflammatory response with the dimentions and localisation of the abscess. Newborns and infants can present symptoms such as stridor and dyspnea (2) and may require relevant protection of the airways. Among factors that predict complications Baldassari et al. include young age, retropharyngeal location, and S. aureus (3). The development of the imaging allowed earlier registration of the changes in the neck what followed earlier administration of the pharmacological treatment. The early treatment in some cases gives improvement and further surgical treatment is unnecessary (4, 5). In recent years our patients are more often early diagnosed and do not require surgical treatment (6).Diagnostic process of infection in the neck spaces may be based on the ultrasonography if performed by an experienced radiologist. Furthermore computed tomography can be reserved for patients who fail to improve and have deep neck space involvement (7). The role of computed tomography in decision making considering the choice of treatment was not uniformly described. Malloy et al. did not find any statistically significant features suggesting conservative or surgical treatment thus they state that computed tomography should be discussed altogether with clinical data, thus leading to the optimal choice of treatment (8). Kirse and Robertson noticed that irregularities of the wall of the observed change will imply the presence of the purulent content and it will point the patients requiring surgical treatment (9). Nagy et al. observed that abscesses with the volume smaller than 2000 mm3 have a greater chance to improve after conservative treatment (10).
In our material changes presenting in CT as polycystic and involving both compartments of the parapharyngeal space suggested surgical treatment. On the other hand the oval changes smaller than 26 mm were treated conservatively with complete resolution.
In patients with worsening course of disease it is worthy to include into the diagnostic process the most frequent infectious nodal pathology such as mononucleosis, cytomegaly, toxoplasmosis or boreliosis.
CONCLUSIONS
On the basis of our observation we conclude that conservative treatment can be applied in patients without complications threatening patients’ life, when improvement of the general condition is observed with normalization of the body temperature and reduction of inflammatory parameters in 24-48 hours. Among the diagnostic tools the ultrasonography is valuable in decision making and the evaluation of the course of disease. CT is more accurate allowing planning further surgical treatment.
Piśmiennictwo
1. Sichel JY, Attal P, Hocwald E, Eliashar R: Redefining Parapharyngeal Space Infections. Annals of Otology, Rhinology & Laryngology 2006; 115(2): 117-123. 2. Abdullah V, Ng KS, Chow SN et al.: A case of neonatal stridor. Archives of Diseases in Childhood 2002; 87(3): 224-5. 3. Baldassari CM, Howell R, Amorn M et al.: Complications in pediatric deep neck space abscesses. Otolaryngol Head Neck Surg 2011; 144(4): 592-5. 4. Johnston D, Schmidt R, Barth P: Parapharyngeal and retropharyngeal infections in children: Argument for a trial of medical therapy and intraoral drainage for medical treatment failures. Int J Ped Otorhinolaryngol 2009; 73: 761-765. 5. Czecior E, Pawlas P, Scierski W et al.: Ropowica przestrzeni przygardłowej. Otolaryngol Pol 2008; 62(4): 486-8. 6. Dębska M, Jabłońska-Jesionowska M, Chmielik M: Parapharyngeal abscesses in children – symptoms, diagnosis and treatment. New Medicine 2008; 3: 50-51. 7. Rozovsky K, Hiller N, Koplewitz BZ, Simanovsky N: Does CT have an additional diagnostic value over ultrasound in the evaluation of acute inflammatory neck masses in children? Eur Radiol 2010; 20: 484-490. 8. Malloy KM, Christenson T, Meyer JS et al.: Lack of association of CT findings and surgical drainage in pediatric neck abscesses. International Journal of Pediatric Otorhinolaryngology 2008; 72, 235-239. 9. Kirse DJ, Roberson DW: Surgical management of retropharyngeal space infections in children. Laryngoscope 2001; 111: 1413-22. 10. Nagy M, Pizzuto M, Backstrom J, Brodsky L: Deep Neck Infections in Children: a new approach to diagnosis and treatment. Laryngoscope 1997; 107: 1627-1634.