© Borgis - New Medicine 4/2012, s. 129-130
Małgorzata Dębska, *Jolanta Jadczyszyn, Lidia Zawadzka-Głos
Rare cause of subperiosteal abscess – a case report
Department of Pediatric Otolaryngology, Medical University of Warsaw
Head of Department: Lidia Zawadzka-Głos, MD, PhD
Summary
Sinusitis occurs frequently in children. Foreign bodies, inserted randomly into nasal cavities might also be the cause of sinusitis in children. In our case, the foreign body obstructing causing the maxillary and ethmoid sinusitis and further, the orbital soft tissue infection with suoeroeriosrali abscessus.
INTRODUCTION
Sinusitis occurs frequently in children and is associated with recurrent infections of the upper airways, which include the nasal mucosa, and in the developing period of the air spaces of the sinuses. In small children, the most common form is the ethmoid sinusitis, unrestrainedly, with high fever, septic state and possible inflammatory reaction on the part of the orbit. Approximately 3% of the cases are affected by orbital complications in the course of sinusitis. A frequent complication arising during the process of subperiosteal abscess formation in due to the presence of innate dehiscence in the wall bones, mainly in the orbital lamina of ethmoid bone of incompletely closed sutures of the thinner bone walls (1). This condition requires intensive intravenous antibiotic therapy and surgical intervention. Orbital abscess occurs most often in the area of superior medial orbit, located between orbital lamina of ethmoid bone and the periosteum of the orbit. It is a displacement of the eye upward and laterally and eye movement disorders might be observed (2, 3).
CASE REPORT
An 11-year-old boy, with a fever lasting 3 days, left eye pain, oedema of the eyelids and the exophthalmos of the left eye, was admitted urgently to the Clinic of Pediatric Laryngology. In medical history taking the patient was hospitalized between 18-19.05.2009 in the Department of Ophthalmology, Centre for Postgraduate Education, in Warsaw because of the inflammation of the left orbital tissues. Physical examination revealed – OP – no change, OL – palperbral oedema and oedema of the orbital tissues, eyeball set in exophthalmos downward and externally, purulent discharge in the conjunctival sac, and the posterior cornea with multiple and linear epithalial defects, without evidence of inflammation in anterior part. The X-ray showed total shading of the left maxillary sinuses, poorly visible edge of the left eye socket, paranasal sinuses unchanged. Sol. Oftaquix, ung. Gentamycini was incorporated for local treatment. After consulting ENT biotraxon was included in the intravenous treatment of sinusitis, and the patient was transferred to the Clinic of Pediatric Otolaryngology. Upon admission to the hospital the boy in generally average condition, suffering, somnolent, complained of pain in the area of the left eye socket increasing when trying to verticalize. On physical examination, oedema of the eyelids and tissues of the left eye socket, eyeball set in exophthalmos, a large amount of abscess discharge in the conjunctival sac.
Limited left eye movements a lack of abduction to the outside. A neurological consultation was held – neurological examinations result was normal. A CT of the paranasal sinuses subperiosteal orbital revealed the inflammation of the orbital and exophthaloms of the eyeball and the displacement of the left ethmoid and maxillary sinuses.
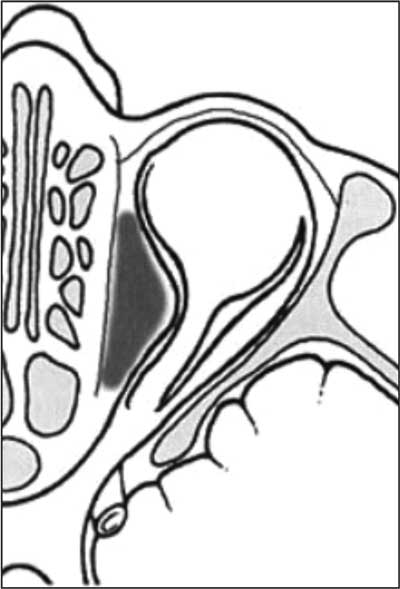
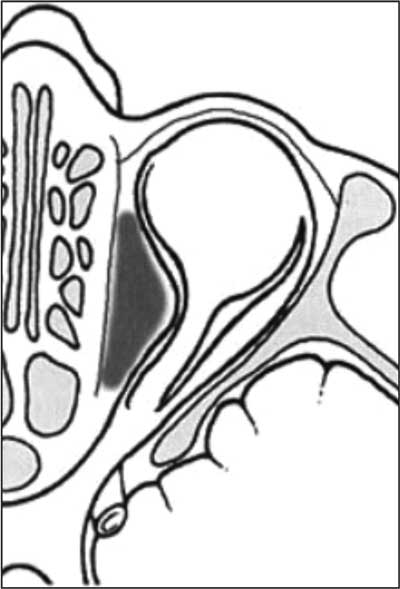
Fig. 1. Subperiosteal abscess (2).
Intravenous antibiotic therapy (Biotraxon, Dalacin) was included in the treatment and local therapy. Qualified for emergency surgery. The left maxillary sinus puncture was conducted – contents were purulent, which were sent for a bacteriological examination. Further, the ethmoidectomy of the left side of the cut content was found Escata – purulent a foreign body (rubber) was removed from the intranasal concha, and granulation tissue was removed from the natural outlet of the sinus, drainage was put. During the first day after surgery still limited mobility of the eyeball was diagnosed, no external abduction. Periodic horizontal nystagmus was found. After neurological consultation check-up CT scan of the head was performed head. The spread of intracranial process was excluded, brain tissue without focal lesions. On the second day after the operation the boy’s condition improved, the study of the ophthalmic left eye movements revealed that they were a little limited upward, movements of the eyeball in the other correct. During the 9-day hospitalization, eyelid oedema subsided, exophthaloms was reduced to the correct eye movements. It was recommended appear for the checkup at the ENT Clinic in two weeks.
Complications of sinusitis result from spreading the disease process of the paranasal sinusesinto the surrounding tissue structures. They are formed as secondary to the acute sinusitis or the exacerbation of chronic sinusitis. Foreign bodies, inserted randomly into nasal cavities might also be the cause of sinusitis in children (4, 5). Initially asymptomatic course, after a few days there is a purulent discharge unilaterally, nasal blockage and nasal odour. A foreign body packed into the nasal cavity for a prolonged period of time might become encrusted with calcium salts eventually manifest as rhinolith – distincly visible considerably saturated shadow on X-ray (6-10).
In our case, the foreign body obstructing in the intranasal concha resulted in the dysfunction of the nasal vantilation and obliterating the drainage of the sinusses, causing the maxillary and ethmoid sinusitis and further, the orbital soft tissue infection with suoeroeriosrali abscessus. Before the surgery the anterior rhinocopy revealed no foreign body due to massive oedema of the mucous membrane and purulent discharge in the nasal cavities. The X-ray and CY of the sinuses revealed no residual foreign body, because it was a non-shadowing foreign body (eraser). It was only during the ehtmiodectomic surgery that the foreign body (rubber) was removed from the medial nasal concha.
Piśmiennictwo
1. Gryczyńska D, Kotecki M: Zapalenie zatok przynosowych u dzieci. Zakażenia 2007; 5. 2. Krzeski A, Galewicz-Zielińska A: Powikłania oczodołowe zapalenia zatok przynosowych. Probl Laryng Codz Praktyce 1999; 14. 3. Kukwa A, Sobczyk G, Kizler-Sobczyk K: Ostre zapalenie zatok – klasyfikacja i leczenie. Przew Lek 2000; 1: 64-69. 4. Webb BD, Pereira KD, Fakhri S: Nasal foreign body as the cause of a subperiosteal orbital abscess in child. Ear Nose Throat J 2010; 89(2): E11-13. 5. Yu L, Li N, Jiang Y, Han M: Clinical analysis of orbital complications of acute pediatric sinusitis. Zhonhhua Er Bi Yan How Tom Jingb Wai Ka Za Zhi 2012; 47(4): 314-316. 6. Szmeja Z: Ciała obce ucha, nosa, gardła, krtani, dolnych dróg oddechowych i przełyku, Przew Lek 2002; 5, 9: 94-96. 7. Spires IR, Smith RJH: Bacterial infections of the orbital and periorbital soft tissue in children. Laryngoskope 1985; 96: 763-767. 8. Kelesidis T, Osman S, Dinerman H: An unusual foreign body as cause of chronic sinusitis: a case report. J Med Case Rep 2010; 26; 4: 157. 9. Calmes MN, Berges C: ENT foreign bodies in children. Arch Pediatr 2009; 16(6): 956-958. 10. Kayhan FT, Sayin I, Yazici ZM, Erdur O: Managment of orbital subperiosteal abscess. J Craniofac Surg 2010; 21(4): 1114-1117.