© Borgis - New Medicine 4/2006, s. 102-106
*Małgorzata Kołodziejczak, Iwona Sudoł-Szopińska1
The practical use of endosonography in the daily work of a surgeon
Department of General Surgery with Subdepartment of Proctology, Solec Hospital, Warsaw
Head of Department: Jacek Bierca, MD PhD
Head of Subdepartment: Małgorzata Kołodziejczak MD, PhD
1Central Institute for Labour Protection – National Research Institute, Warsaw
Director: Prof. Danuta Karadecka, MD, PhD and Department of Diagnostic Imaging, Medical School, Warsaw, Head of the Dept. Prof. Wiesław Jakubowski, MD PhD
Summary
Summary
The usefulness of endosonography before an operational diagnosis of proctological diseases is undeniable nowadays. This paper discusses the practical aspect of this diagnostic method, namely, in which situations a surgeon can take advantage of it, and what is more, to what degree the endosonography result can influence the decision about an operation as well as the type of procedure to be applied. The use of endosonography is presented for such diseases as: abscesses and fistulas of the anus, anal sphincter defects and narrowing of the anal canal.
Introduction
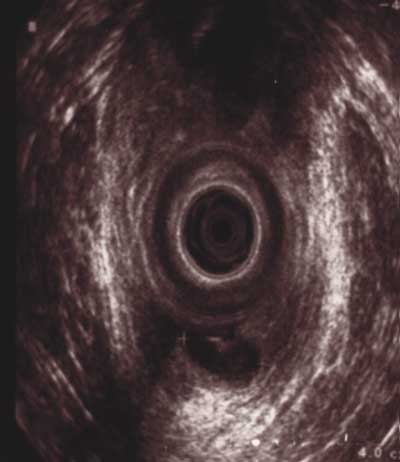
Introducing endosonography has become a breakthrough in the diagnosis of proctological diseases. Although the method has been known since 1956 [1, 2], for the first 30 years it was only used in the diagnosis of tumours of the rectum. Since 1989 it has been used in the diagnosis of inflammatory disorders of the anus and rectum as well as injuries of the anal sphincters [3, 4, 5, 6, 7]. That was when an anal probe with a plastic narrow cone was used for the first time. Thanks to the use of rotation of the probe in the transverse position in relation to the long axis of the anal canal, it was possible to obtain transverse cross-sections of the anal canal as well as the surrounding tissues that measured 360°, which made the morphological assessment of anal sphincters accurate [2, 3] (Fig. 1).

Fig. 1. Endorectal probe with a narrow (diameter 17 mm) plastic cone (BK Medical).
In order to examine the anal canal, different kinds of probes can be used such as: sector-sector, sector-linear and mechanical, also called rotating. The last ones emit waves of frequency measuring 7.0 MHz, which gives high resolution as well as deep penetration and good visualization of tissues surrounding the anal canal in the range of 4 cm from it [2]. Thanks to the insertion of the rotating probe one can get 360° transverse sections of the anal canal and the surrounding tissues, which is of great help in rating anal sphincter defects [8, 9].
The majority of reports connected with ultrasonographic diagnosis are written by specialists of pictorial diagnosis. The presented paper is the result of long-term cooperation of a surgeon with a radiologist. Its goal is to show to what degree endosonography can have an influence on a surgical procedure.
Below, the application of endosonography before operational diagnosis of abscesses and fistulas of the anus, injuries of it as well as narrowing of the anal canal is presented.
Anal abscesses
Patients who have anal abscesses do not have to have any special diagnosis before an operation. Abscesses located superficially (subcutaneous and ischiorectal) do not cause any diagnostic problems for a surgeon or proctologist. The clinical picture is clear and it includes: pain, high temperature, redness as well as fluctuation of skin and subcutaneous tissue near the anus. In such cases performing endosonography is useless. However, it is different when it comes to abscesses which are located suprasphincterically. The clinical picture is not straightforward. In connection with the anatomical structure of the anal canal, e.g. the lack of pain innervation above the dentate line, a patient with a suprasphincteric abscess does not feel any pain, except the feeling of distension in the anus and rectum. The local symptoms on the anus and anal canal´s side are slight. However, general symptoms dominate such as hectic temperature and the bad condition of the patient. It sometimes happens that the first doctor examining such a patient is a urologist, as the patient suffers from urinary obstruction. That is why a high rectal abscess is difficult to recognize in a clinical examination. It often happens that the final diagnostic checkup is the endosonography.
The examination shows the receptacle of fluid precisely, which is located above the anal sphincters, and it is an examination of choice in the diagnosis of high intrasphincteric (Fig. 2), suprasphincteric and pelvic-rectal abscesses [10, 11, 12].
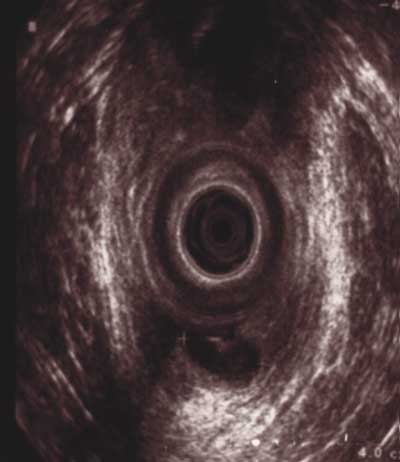
Fig. 2. High, posterior, intrasphincteric anal abscess.
Anal endosonography has been used during the diagnosis of abscesses and fistulas in the Proctology Department since 1996 and in most cases their endosonographic images coincided with the intra-operative diagnosis. However, looking through the literature, it is hard not to mention the discrepancy between the results. According to those who conducted the checkup, it is possible to reveal all of the abscesses while using endosonography [13]. However, Law et al. [14] describe some difficulties in endosonographic diagnosis of suprasphincteric and ischiorectal abscesses. In our own material endosonography shows high efficiency as all of the abscesses were detected by this method and then they were confirmed intraoperatively [15].
A good way of supporting anal endosonography is with transperineal sonography. Thanks to this method it is possible to confirm the presence of an ichiorectal abscess as well as other abscesses located more superficially. Ultrasonography through the perineum is another means of diagnosis among those patients who have strong, painful ailments in whom the insertion of a probe would be simply impossible without an anaesthetic [16, 17, 18, 19].
Comparing the diagnostic effectiveness of anal ultrasonography and transperineal sonography it is necessary to state that anal endosonography is more accurate when it comes to the rating of structures highly located. This is due to the possibility of better visualization of the anatomy of the region to be examined, and especially the interaction between an abscess or fistula of the anus and the anal sphincters. The importance of transperineal sonography increases in the diagnosis of any changes located very superficially, while in anal endosonography it is possible for artefacts to appear that are the result of the presence of air between the probe and anal canal walls shading the endosonographic image. Also, transperineal sonography can be performed by doctors who are not necessarily skilled in endosonography. In our practice these two kinds of approaches are combined, when necessary [20].
How important it is to recognise that a patient has got a suprasphincteric abscess properly is a fact that unrecognised and untreated can lead to septic complications, which may be life-threatening or in final cases may lead to Fournier´s necrosis of the perineum. It is the worst, although infrequent, sceptic complication of outstaying abscesses. It causes extensive necrosis of peritoneum tissues with recrement. It often coexists with necrosis of the scrotum, caused by bacterial embolisms in vessels. This complication concerns obese people who suffer form diabetes as well as patients with lowered immunity and people with other general illnesses such as tuberculosis, scattered, malignant process or HIV.
To sum up, endosonography enables one to recognise and describe precisely the location of an abscess. It allows a surgeon to decide whether a patient needs to be operated on and, thanks to the precise localisation, what operational tactics ought to be followed, namely, from what approach the operation should be conducted, that is, if an abscess should be opened from the skin side or the anal canal.
Unfortunately, it often happens that a patient with an abscess is taken to emergency during the night, when there is no possibility to perform endosonography. If the patient´s general state allows, it is worth waiting until morning, and then performing the endosonography before the procedure, as it helps in better preparation for the operation, namely, to define the localisation (the type) of the abscess, and to exclude the possible coexistence of a fistula and possible anal sphincter defects.
Anal fistulas
In the case of anal fistulas, anal endosonography has become a routine medical examination performed before an operation (Fig. 3). It is performed for three reasons: in order to define the anatomical course of a fistula precisely, i.e. its relation to the anal sphincters, to describe the location of its internal orifice, and to exclude its ramification (i.e. complex fistula) [21, 22, 23]. Visualization of the internal outlet of the fistula is not always easy to fulfil and endosonography is frequently elusive here. This method enables one either to confirm or exclude the connection of inflammatory changes (mainly fistulas) with the anal canal, which is crucial in differentiation of a fistula with Verney´s disease, which is the inflammation of apocrine glands of the skin and the subcutaneous tissue in the anus area.

Fig. 3. Complex, horseshoe anal fistula, on the posterior, right and left wall of the anal canal.
The second reason why anal endosonography ought to be performed before an operation is the necessity to diagnose precisely with regard to law. It is of a great importance when it comes to fistulas which are high, anterior or recurrent, where the possibility of complications after an operation is high. Endosonography should be definitely made when a patient makes claims against a doctor.
In addition, this medical examination ought to be conducted after an operation of an anal fistula (from our own experience it is three months after an operation), which enables the detection of the eventual recurrence in advance.
However, the most decisive is the result of a clinical, proctologic examination, as the endosonography image can be misleading. For instance, the image of a post-operational scar suggests the recurrence of a fistula repeatedly (both changes, i.e. a fistula and a scar, have low echogenicity) [23, 24]. The application of hydrogen peroxide through the fistula´s external orifice (if it is permeable) is of much help. After the application of it, the fistula, in contrast-enhanced endosonography, becomes hyperechoic [24, 25, 26].
Anal sphincter defects
Enables the differentiation of anal incontinency, i.e. mechanical or neurogenic. It is very substantial, especially in the diagnosis of obstetric defects, as it influences further therapeutic management: treatment of mechanical defects is often surgery, while in neurogenic ones patients are directed for treatment by a method called biofeedback. When it comes to mechanical defects, endosonography locates the defects precisely (that is, which sphincter is affected, and in which part of the anal canal, i.e. subcutaneous, superficial or high) and it defines how extensive the loss of muscles is, which enables a surgeon to plan anal sphincter reconstruction. If the loss is more than half of the anus circumference, the possibility of a reconstructive operation is unlikely.
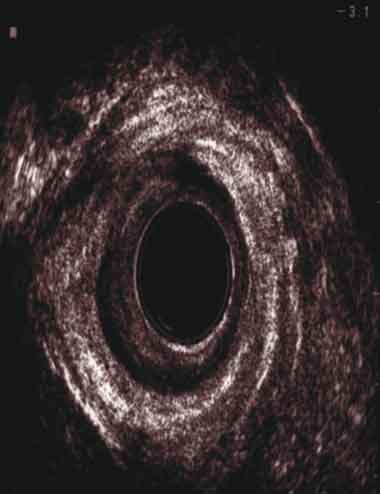
The sonographic diagnosis of defects of the external sphincter muscle and the puborectalis muscle (PR) is more difficult than the internal anal sphincter because of its heterogeneity, poorly visible external outlines and the oblique course of the PR. The disruption of the continuity of the external anal sphincter muscle or PR, which have the same and heterogeneous structure, is visible in anal endosonography as a hypoechoic area within hyperechoic muscles [1, 27]. When it comes to the muscle of the internal anal sphincter, which is hypoechoic, the image of a defect will present itself as a hyperechoic area (Fig. 4). If there are any doubts, it is possible to use a dynamic examination, asking the patient to squeeze the sphincters. Such a test enables recognition of the neurogenic type of incontinency (no contraction of strated muscles, i.e. external anal sphincter and PR), and it shows the disruption of the continuity more accurately.
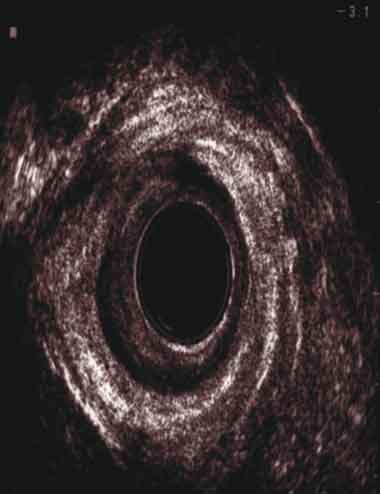
Fig. 4. External and internal anal sphincter defects on the right-anterior wall of the anal canal.
A surgeon while planning the reconstruction of anal sphincters, in every case, ought to conduct endosonography as well as functional examinations (anorectal manometry and electromyography), because only the whole evaluation of the anatomy and the function of the anal sphincters allows one to plan the type of procedure and predict the success of an operation. What ought to be remembered is to keep a patient informed about the potential risk of failure connected with an operation before conducting it.
Narrowing of the anal canal
The proper diagnosis before an operation has a basic meaning when planning the treatment of strictures of the anus, since the type and extent of an operation depend on aetiology and the level and length of the stricture. It is particularly substantial in secondary strictures following radiotherapy, since in those cases the changes can be connected with the rectum wall too and accurate evaluation before an operation determines the surgical approach (perineal or laparotomy). In widespread strictures after radiotherapy, application of a stoma is often indispensable. When there is a stricture of a big degree, there is no opportunity to use a rectoscope, or even perform a digital rectum examination. Even examination under anaesthesia can give insufficient information before dilatation of the anal canal. In addition, any information connected with the state of the sphincter muscles is of great importance for a surgeon.
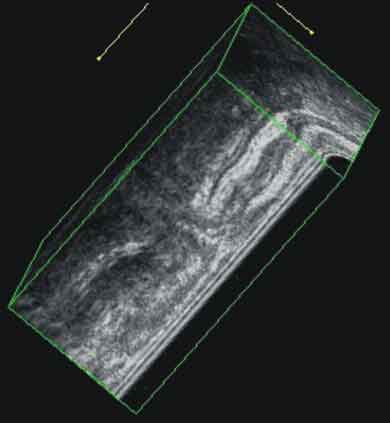
Strictures are made very clearly visible in anal endosonography by means of a probe which has the ability to visualize in an axial plane, or in 3D endosonography, which is currently an established method in evaluating pathology of the anal canal [28]. In such cases, 3D endosonography is performed from the transperineal approach. The images show the extent of the strictures precisely.
Apart from its use in diagnosis of strictures of the anal canal, 3D anal endosonography, due to imaging in many planes, is useful to diagnose complex abscesses and fistulas of the anus, including ano-vaginal fistulas [29] (Fig. 5). These are other examples of the practical use of anal endosonography, since there are many other indications in which a surgeon takes advantage of this non-invasive, widely accessible diagnostic method before surgery.
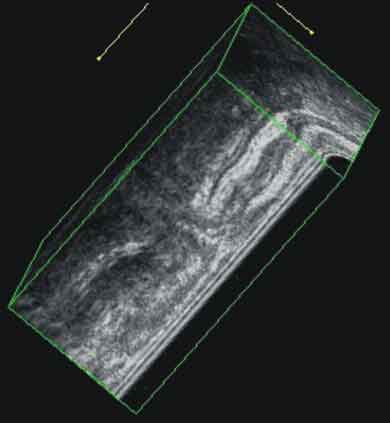
Fig. 5. 3D endosonography with a saggital presentation of the ano-rectal fistula (BK Medical).
To conclude, anal endosonography has been used by the authors of this paper for many years and appears to be a valuable diagnostic tool. We found that especially contrast-enhanced endosonography (i.e. endosonography with simultaneous contrast injection) in women frequently performed with simultaneous transvaginal finger examination significantly increases diagnostic accuracy of endosonography in defining the type of anal fistulas, differentiation between simple and complex fistulas and in location of internal opening of anal fistulas. In these cases standard, i.e. non-contrast, endosonography is not a reliable method in differentiation between scars and active recurrent anal fistula. Contrast-enhanced endosonography allows also for reliable diagnostics of anal abscesses and their differentiation with anal fistulas. In the case of high ischiorectal abscesses anal endosonography should however be supported by extended evaluation of suprasphincteric soft tissues in order to exclude extension of an abscess to the pelvirectal fossa. It should also be remembered that there is high coexistence of anal sphincter defects in patients with anal fistulas and abscesses. Interpretation of the endosonographic images in such cases should be careful because of similar image of the anal fistula and anal defect. Contrast-enhanced endosonography is very helpful here under the condition that the opening of the fistula is patent; if it is not the value of endosonography is limited. Nevertheless, our collected data concerning anal endosonography verified by surgery show that this imaging tool is a reliable method in preoperative diagnostics of anal fistulas, abscesses and anal sphincter trauma. The wide utility of endosonography in our everyday practice increases the effectiveness of the treatment, and especially allows postoperative complications such as fistula recurrence and insufficiency of anal sphincters to be limited.
Piśmiennictwo
1. Sudoł-Szopińska I., Jakubowski w. Endosonography of anal canal diseases. Ultrasound Q. 2002;18:13-33. 2.Sudoł-Szopińska I.: Przydatność endosonografii w diagnostyce przetok.i ropni odbytu. Rozprawa habilitacyjna. Warszawa 2003; Medical Communications. 3.Law P.J., Bartram C.J.: Anal endosonography: Technique and normal anatomy. Gastrointest Radiology 1989; 14: 349-353. 4.Schaffzin D.M.,Wong W.D.: Surgeon-performed ultrasound: endorectal ultrasound. Surg Clin North Am 2004 Aug; 84(4): 1127-49. 5.Rieger N., Tjandra J., Solomon M.: Endoanal and endorectal ultrasound: application in colorectal surgery. ANZ J Surg 2004 Aug; 74(8): 671-5. 6. Bartram C.I., DeLancey J.O.L. Imaging pelvic floor disorders. Springer -Verlag Berlin Heidelberg 2003. 7.Bartram C.I., Frudinger A. Handbook of anal endosonography. Wrightson Biomedical Publishig LTD, Petersfield UK, Bristol USA 1997. 8.Damon H., Henry L., Bretones S., Mellier G., Minaire Y., Mion F.: Postdelivery anal function in primiparous females: ultrasound and manometric study. Dis Colon Rectum 2000; 43: 472-477. 9.Damon H., Henry L., Barth X., Mion F.: Fecal incontinence in females with a past history of vaginal delivery: significance of anal sphincter defects detected by ultrasound. Dis Colon Rectum 2002; 45: 1445-1451. 10.Cataldo PA, Senagore A, Luchtefeld MA. Intrarectal ultrasound in the evaluation of perirectal abscess. Dis Colon Rectum 1993;36:554-558. 11.Kumar A, Scholefield JH. Endosonography of the anal canal and rectum. World J Surg 2000;24:208-215. 12.Law PJ, Talbot RW, Bartram CI, Northover JMA. Anal endosonography in the evaluation of perianal sepsis and fistula in ano. Br J Surg. 1989;76:752-755. 13.El-Mouaaouy A, Tolksdorf A, Starlinger M, Becker HD Endoskopische Sonografie des Anorektums bei entzudlichen Enddarmerkrankungen Z.Gastroenterol.1992;30/7/,486-494. 14.Law PJ,Talbot RW, Bartram C,J, Northower JMA Anal endosonography in evaluation of perianal sepsis and fistula in ano Br.J.Surg 1989;76,752-755. 15.Kołodziejczak M, Stefański R" Zastosowanie Ultrasonografii przezodbytniczej w diagnostyce wysokich ropni odbytu" Proktologia 2000; 1(1):70-76. 16.Kleinubing H,Jannini JF,Malafaia O,Brenner S,Pinho M. Transperineal ultrasonography. New method to image the anorectal region. Dis Colon Rectum 2000;43:1572-1574. 17.Roche B, Deleaval J, Fransioli A, Marti MC. Comparison of transanal and external perineal ultrasonography. Eur Radiol 2001;11:1165-1170. 18.Rumens DJ, Strang JG, Bogineni-Misra S, Wexler IE. Transperineal sonography of the rectum: anatomy and pathology revealed by sonography compared with CT and MR imaging. AJR 1998;170:637-642. 19.Stewart LK, MsGee J, Wilson SR. Transperineal and transvaginal sonography of perianal inflammatory disease. AJR 2001;17:627-632. 20. Stefański R, Kołodziejczak M, Kosim A Zastosowanie ultrasonografii przezkroczowej jako badania uzupełniającego ultrasonografię przezodbytniczą w diagnostyce chorób kanału odbytu i odbytnicy. Proktologia 2001; 4(5) : 358-367. 21.Halligan S. Review imaging fistula-in-ano. Clinical Radiol 1998;53:85-95. 22. Cho D-Y. Endosonographic criteria for an internal opening of fistula-in-ano. Dis Colon Rectum 1999;42:515-519. 23.Choen S, Burnett S, Bartram CI, Nicholas R.J.: Comparison between anal endosonography and digital examination in the evaluation of anal fistulae. Br J Surg 1991;78:445-447. 24.Cheong DMO, Nogueras JJ, Wexner SD, Jagelman DG. Anal endosonography for recurrent anal fistulas:image enhancement with hydrogen peroxide. Dis Colon Rectum1993;36:1158-60. 25.Kruskal JB, Kane RA, Morrin MM. Peroxide-enhanced anal endosonography: technique, image interpretation, and clinical applications. Radiographic 2001;21:51-73. 26.Poen AC, Felt-Bersma RJF, Eijsbouts QAJ, Cuesta MA, Meuwissen SGM. Hydrogen peroxide-enhanced transanal ultrasound in the assessment of fistula-in-ano. Dis Colon Rectum 1998;41:1147-1152. 27. Fitzpatrick M., O´Herlihy C.: The effects of labour and delivery on the pelvic floor. Best Practice and Research Clin Obstet Gynaecol 2001; 15: 63-79. 28.Slapa R.Z, Kasperlik-Zaluska A.A., Polanski J.A., Borowicz K., Serafin-Krol M., Jakubowski W.: Three-dimensional sonography in diagnosis of retroperitoneal hemorrhage from adrenocortical carcinoma. J Ultrasound Med 2004; 23: 1369-1373. 29.Hertzberg B.S., Bowie J.D., Weber T.M., Carroll B.A., Kliewer M.A., Jordan S.G.: Sonography of the cervix during the third trimester of pregnancy: value of the transperineal approach. AJR1991; 157: 73-76.