© Borgis - New Medicine 3/1999, s. 50-51
Jerzy Rak, Lucyna Pośpiech, Marek Bochnia, Agnieszka Jabłonka
Partial resection of tonsils - tonsillotomy; analysis of indications and assessment of treatment results in children in the Otolaryngology Clinic of the Medical University of Wrocław, 1989-1998
Otolaryngology Clinic of Medical University in Wrocław
Head: Prof. Pośpiech Lucyna, PhD
Summary
During the last 10 years our clinic has performed 432 partial resections of palatine tonsils - unilateral and bilateral tonsillotomy. The number of surgical interventions has been increasing significantly in line with the frequency of obstructive sleep apnoea diagnosis in small children. Hypertrophic pharyngeal and palatine tonsils (usually showing no symptoms of inflammation) are the cause of sleep apnoea in the majority of children. Surgical treatment with this method gives good results, and complications, such as bleeding in the early postoperative period or inflammation of the remaining tonsillar and peritonsilar tissue later are noted in very few cases, with a frequency comparable to that observed after tonsillectomy. Thus complications cannot provide an argument against this surgery which is deemed less radical when compared to tonsillectomy.
The purpose of the study was an analysis of the incidence of tonsillotomy and adenotonsillotomy, an assessment of the indications for this surgery, and the results obtained in the Otolaryngology Clinic of the Medical University in Wroclaw during a period of 10 years.
Results and discussion
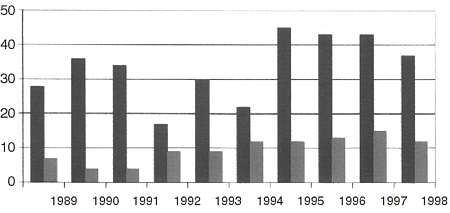
Within the last ten years in our clinic, tonsillotomy and adeontonsillotomy have been performed on 432 children, of which 228 were females and 204 males, aged 2-16 years. The surgery included 97 tonsillotomies and 336 adenotonsillotomies. In 17 patients, the adenoid was removed 6 months to 7 years before tonsillotomy. In the group of operated children, there were 13 individuals undergoing haematological treatment at the same time, because of haemorrhagic diathesis or anemia, 7 individuals with Down´s syndrome and 2 with infantile spinal paralysis. 305 procedures were conducted under general anesthesia and 127 under local anaesthesia. In the course of the first 5 years of the last decade, the annual number of cases for this mode of tonsil surgery was stable, while within the following 5 years both procedures increased significantly in frequency.
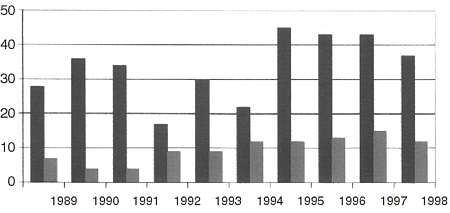
Fig. 1. Number of tonsillotomies and adenotonsillotomies in each year.
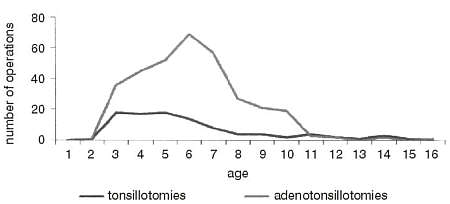
Surgery under general anaesthesia, amounting to 70% of our cases, seemed to rise in number between 1989 and 1998. Most of the interventions were performed on children from 3 to 7 years of age: 70% of the tonsillotomies and 65% of the adenotonsillotomies (Fig. 2)
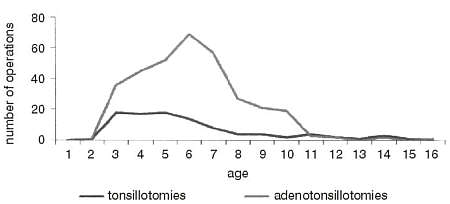
Fig. 2. Number of operations inrelation to the age.
The most common indications for the surgery included: hypertrophia of the pharyngeal or palatine tonsils with significant impairment in nasal patency, with snoring, breathing with open mouth, hearing loss, malocclusion and a history of frequent upper respiratory tract infections, otitis media incidents, tonsillitis and bronchitis. In recent years, a popular indication for the resection of tonsils has been an obstructive peripheral sleep apnoea. Since 1995, 97 children have been operated on for this reason, 41% in this period and 23% within the last ten years. Similar data are reported by Kukwa at al. (8) and Powejbo at al. (10). As a principle, the qualification for tonsillotomy in children was, as in other centre (5, 12, 14), based on a diagnosis of large tonsillar hypertrophy with no evidence of an inflammatory process. Nevertheless, in 32 cases (7.4%), a partial tonsil resection was performed, even though the patients were qualified for tonsillectomy, out of respect for the parents´ refusal of radical resection. Such refusals, with a tendency to choose partial tonsil resection, has been observed in recent years, which undoubtedly has resulted in a rise in the number of tonsillotomies.
In assessment of the treatment results, complications, occuring in 7% of our research group, must be discussed. Bleeding prevailed as a main complication, with incidence of 23 cases. 21 of these were early bleedings, directly after the surgery and within the first twenty-four hours. In 15 children, this was a consequence of the performed adenoidectomy and required posterior nasal packing and even erythrocyte mass and blood substitute transfusion due to symptoms of posthaemorrhagic anaemia. In 6 children after tonsillotomy, parenchymatous or venous bleeding occurred and was locally controlled. One patient presented a significant uncontrolled tonsil hemorrhage, so extirpation of the tonsil with its capsule was carried out, the vessels ligated and palatine arches sutured. Three children suffered from bleeding on the second and one on the fifth day after tonsil surgery. In these 3 children the bleeding was a consequence of remaining unresected adenoid tissue and stoped after the readenoidectomy, the latter patient presented prenchymatous bleeding from a tonsil after its partial resection in the course of scarlet fever revealed after the surgery. The majority of the haemorrhagic incidents occurred in older children (5-12 yrs) in relation to the size of the hypertrophic tonsils. Bleeding incidence as a postsurgical sequel, its character and the course, did not differ in our group in comparison to those reported by other authors, which varies between 0.5% and 10% (1, 2, 3, 4, 6, 7, 9, 11, 13). No significant difference has been observed between the incidence of the bleeding after tonsillotomy and after tonsillectomy. Another noted surgical complication was a local inflammatory reaction with a considerable edematous component, concering 19 patients. One child, due to a very acute attack of shortness of breath in the course of bronchial asthma, was transferred to the Pediatric Clinic for further management and soon after bilateral pneumonia was revealed. In the further follow-up examinations, neither pathomorphological nor functional complications were observed. The described complications did not show any relationship to the anaesthesia mode. It is worth mentioning that all the other children showed, after convalescence, full recovery in nasal patency, breathing, and an improvement in hearing, if hearing loss had been found before the surgery. The patients who were qualified for tonsillotomy due to breathing disturbances resulting in sleep apnoea showed a recession of the symptoms during about six months following the surgery. Similar favourable results are reported, among others, by Kukwa (8) and Powajbo (10).
The small number of complications after tonsillotomy, especially bleeding, which is regarded by opponents as the most serious risk, less radical resection of the lymphatic tissue (important for the immune system and child development) and the rapid improvement in general well-being could still make this surgery efficient and safe.
Conclusions
1. Within the last decade, the number of partial tonsil resections in our clinic showed an upward tendency.
2. A common indication for tonsillotomy, especially within the last 5 years, was sleep apnoea syndrome in children. 41% of the surgery was performed due to sleep apnoea.
3. The incidence of complications after the partial resection of tonsils, amounting to 7%, did not differ significantly from the number of complications after tonsillectomy
4. No relationship between the method of anaesthesia and the incidence of complications was observed.
Piśmiennictwo
1. Burczyński E.: Krwawienia po adenotomii u dzieci. Otolaryng. Pol., 1983, 37:3-148. 2. Capper J., Randall C.: Postoperative haemorrhage in tonsillectomy and adenoidectomy in children. J. Laryng. Otol., 1984, 98:4-363. 3. Chmielik M.: Analiza krwawień po adenotomii i tolsylotomii u dzieci. Otolaryng. Pol., 1983, 37:2-148. 4. Cymbarewicz-Powierza S. et al.: Krwawienia po tonsilektomiach. Otolaryng. Pol. 1983, 37:2-146. 5.Davidson T., Colloway C.: Tonsillectomy and adenoidectomy. Its indications, its problems. West. J. Med., 1980, 133:5-451. 6. Greczek-Harkawy J.: Przyczynek do zapobiegania krwawieniu po wyłuszczeniu migdałków podniebiennych. Otolaryng. Pol. 1983, 37:3-259. 7. Hayddon-Baillie M.: Aspects of treatment tonsilloadenoidectomy. Personal observations in 15 000 cases. Ann. Royal Col. Surg. Eng., 1977, 59-128. 8.Kukwa A. et al.: Diagnostyka i leczenie zaburzeń oddychania podczas snu u dzieci. Otolaryg, Pol. 1997, 50, suppl. 22, 467. 9. Łaciak J.: Powidłania po wyłuszczeniu migdałków podniebiennych na materiale Kliniki AM w Łodzi. Otolaryng. Pol., 1957, 11:3-259. 10. Powajbo K., Gryczyńska D.: Obturacyjny bezdech senny u dzieci - nowe aspekty kliniczne. Otolaryng. Pol., 1997, 50, suppl. 22, 471. 11. Soboczyński A. et al.: Porównanie częstości występowania krwawienia po wyłuszczeniu migdałków podniebiennych. Otolaryng. Pol. 1983, 37:2-149. 12. Witucki J.: Wskazania do operacji migdałków. Wiad. Lek. 1987, 40:14-975. 13. Witucki J.: Powikłania operacyjnego leczenia migdałków. Otolaryng. Pol., 1992, 46:1-46. 14. Witucki J.: Operacje migdałków w rejonie gdańskim w latach 1961-1985. Otolaryng. Pol. 1989, 43:4-333.