© Borgis - New Medicine 3/2010, s. 90-91
*Ewa Ogłodek, Aleksander Araszkiewicz
Application of the Short Evaluation Scale of Schizophasia (SESS) in a Female Patient with Paranoid Schizophrenia
Chair and Clinic of Psychiatry of the Nicolaus Copernicus University Collegium Medicum in Bydgoszcz, Poland
Head of Clinic: Prof. Aleksander Araszkiewicz, MD, PhD
Summary
Language disturbances, along with formal thinking disturbances, form one of the basic criteria of diagnosing schizophrenia. One of the language disturbances described in the literature is schizophasia, which is associated with disorders in the functioning of cerebral structures. The aim of this study was to analyse language disturbances in a 60-year-old female patient with paranoid schizophrenia. The examined patient achieved a score of 10 points on the Short Evaluation Scale of Schizophasia, which is proof of an acute phase of schizophasia. High intensity of schizophasia symptoms is often associated with a bad prognosis of a psychotic disease.
Introduction
Schizophrenia is a complex disorder with a wide range of symptoms. Formal thought disorder is one of the main symptoms of schizophrenia, and there is increasing evidence that it can be traced to abnormalities in specific brain regions (1). In particular, formal thought disorder is often interpreted as a complex dysfunction of the language system, involving executive function, semantic memory and spreading activation in semantic memory (2, 3). Formal thought disorder, defined by DSM-IV as "disordered speech or utterances", also known as schizophasia (language disorder in schizophrenia), has been treated as a core feature of psychosis since Kraepelin and Bleuler. The aim of this study was to analyse language disturbances in a patient with paranoid schizophrenia.
Case report
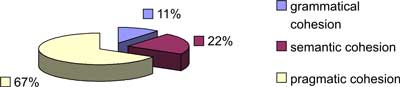
The aim of the study was to evaluate schizophasia in a 60-year-old female patient with paranoid schizophrenia. For the psychiatric examination of the patient, the DSM-IV classification was applied and paranoid schizophrenia was diagnosed. Next, using the Short Evaluation Scale of Schizophasia (SESS), the grammatical, semantic and pragmatic cohesion of the patient's linguistic utterances were evaluated (4). The total score of SESS was 9. An analysis of the Short Evaluation Scale of Schizophasia showed that the patient obtained the highest value for the "pragmatic cohesion" factor. Figure 1 presents the percentage distribution of factors of schizophasia in the patient with paranoid schizophrenia.
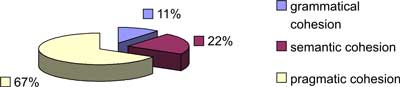
Fig. 1. Short Evaluation Scale of Schizophasia (SESS).
Discussion
In our investigation the 60-year-old female patient met the criteria of paranoid schizophrenia. The patient's score on the Evaluation Scale of Schizophasia revealed the highest value of the "pragmatic cohesion" factor, which may suggest that the subjective reality of auditory and verbal hallucinations is related to motor mechanisms of speech comprehension.
According to Walter H. et al. schizophrenic patients meeting the Diagnostic and Statistical Manual of Mental Disorders 4th Edition (DSM-IV) criteria for schizophrenia showed less activation in frontoparietal and subcortical regions compared to healthy subjects. The posterior part of this brain region has a major role in semantic memory. The most common disturbances of speech in schizophrenic psychoses are connected with defects in this region of the brain (5).
Kerns JG et al. described how specific neuropsychological defects are predictive of general functioning in schizophrenia. They found that the affected neuropsychological domains in schizophrenia patients included verbal memory, vigilance, and executive function. Furthermore, there are reports about the relationship between neurocognitive functioning and psychotic symptoms (especially negative ones) in terms of predicting social functioning in schizophrenia patients (6).
Stirling J et al. (7) investigated the relationship between symptoms, cognitive function, and the ability to perform basic activities of daily living in schizophrenia, and they found that cognitive function predicted both concurrent symptoms and basic activities of daily living.
Liddle et al. found decreased regional cerebral blood flow (rCBF) in the right Brodmann area (BA) 47/45, BA 44 and in the bilateral angular gyrus. Regional CBF was increased in the anterior cingulate cortex, BA 9/10, the dorsomedial thalamus and the left STG (8).
In a single photon emission computed tomography (SPECT) study, Ebmeier et al. observed increased tracer uptake in the anterior cingulate in the disorganisation syndrome.
Recently, Lahti et al. demonstrated a positive correlation between disorganisation syndrome and rCBF in the left posterior inferior frontal gyrus (IFG) extending into the anterior insula (9). Understanding the physiological function of the hyperperfused regions is essential to recognise their contribution to the dysfunctions in formal thought disorder. The most posterior part of the left STG and the left angular gyrus have a key role in providing access to semantic information. Lesions in the left posterior STG can cause informational disconnection between verbal and non-verbal domains of knowledge. The left angular gyrus is involved in higher-order conceptual knowledge and semantic processing (for a review see Vigneau et al. (10)). Lesions of this region have been related to severe semantic - but not phonological - impairments. Dysfunction of the left posterior STG and angular gyrus may, therefore, result in disorders of semantic processing, as found in formal thought disorder.
A high intensity of schizophasia symptoms is often associated with a bad prognosis of a psychotic disease. Early language disturbances can be predictors of schizophrenia. Symptoms of schizophasia disturb the everyday communication of patients with schizophrenia, thus disturbing the social functioning of these patients and causing their social isolation.
Piśmiennictwo
1. Dronkers NF et al.: Lesion analysis of the brain areas involved in language comprehension. Cognition 2004; 92: 145-77. 2. Heim S: The structure and dynamics of normal language processing: insights from neuroimaging. Acta Neurobiol Exp (Wars) 2005; 65: 95-116. 3. Horn H. et al.: Structural and metabolic changes in language areas linked to formal thought disorder. Br J Psychiatry 2009; 194(2): 130-8. 4. Woźniak T, Czernikiewicz A: Krótka skala oceny schizofazji. Badania nad schizofrenią 2002/2003, 569-76. 5. Walter H et al.: Working memory dysfunction in schizophrenia compared to healthy controls and patients with depression: evidence from event-related fMRI. Neuroimage 2007; 35: 1551-61. 6. Kerns JG, Berenbaum H: Cognitive impairments associated with formal thought disorder in people with schizophrenia. J Abnorm Psychol 2002; 111: 211-24. 7. Stirling J et al.: Thought disorder in schizophrenia is associated with both executive dysfunction and circumscribed impairments in semantic function. Psychol Med 2006; 36: 475-84. 8. Liddle PF et al.: Patterns of cerebral blood flow in schizophrenia. Br J Psychiatry 1992; 160: 179-86. 9. Lahti AC et al.: Correlations between rCBF and symptoms in two independent cohorts of drug-free patients with schizophrenia. Neuropsychopharmacology 2006; 31: 22-30. 10. Vigneau M et al.: Meta-analyzing left hemisphere language areas: phonology, semantics, and sentence processing. Neuroimage 2006; 30: 1414-32.