© Borgis - New Medicine 3/2012, s. 83-90
*István Barcs1, Anita Becker1, Barbara Sauer1, Gyula Domján2
Molecular laboratory tools for rapid diagnostics of systemic infections, and in clinical epidemiological practice
1Institute of Health Promotion and Clinical Methodology, Department of Epidemiology, Faculty of Health Sciences, Semmelweis University, Budapest, Hungary
Director of the Institute: prof. Gyula Domján, MD, PhD
2Institute of Health Promotion and Clinical Methodology, Faculty of Health Sciences, Semmelweis University, Budapest, Hungary
Dean of Faculty: prof. Judit Mészáros, PhD
Summary
The aims of a clinical microbiology laboratory are rapid demonstration of pathogens from clinical samples and providing a dependable base for managing infections. Three cases are discussed with aspects of rapid clinical diagnosis and application of molecular tools. Microscopic examination of positive blood cultures of septic patients demonstrated elongated bacterial forms which were identified as Escherichia coli within 4 hours by fluorescent in situ hybridization (FISH). Irregular shape was attributed to previous administration of cefuroxime. In the second case, blood and urine cultures of a cancer patient yielded identical strains of E. coli and Enterococcus faecalis, as well. Strains from blood were demonstrated and identified by the FISH method. Pulsed field gel electrophoresis (PFGE) demonstrated identity of isolates of different origin. We diagnosed sepsis provoked by pyelonephritis. In the third case, using a real time polymerase chain reaction (PCR) method, methicillin-resistant Staphylococcus aureus (MRSA) was detected from the wound infection of a patient who was infected by an MRSA during his former hospitalization. PFGE documented that these repeated isolates were different from all strains isolated in the same period from patients at the same ward, that is he was not re-infected after his second admission.
Introduction
Microbiology is the field of medical sciences which – through the in vitro examination of microorganisms and their effects on human health – is dedicated to supporting the management of infectious diseases including detection of pathogens either from clinical or screening samples, collection of data on antibiotic sensitivity, surveillance of epidemics, vaccination and the study of microorganisms for future exploitation. The aims of these studies are diagnostic investigations of the clinical specimens to identify infectious diseases and to ascertain their source, and particularly to establish an effective antimicrobial therapy. Clinical microbiology, confirming the previously stated clinical diagnosis, is closely related to the medical attendance. It aims to detect microorganisms that could be accepted as causative or participating agents of an actually manifested infection. This detection could be attained either directly (by culture or microscopically) or indirectly by demonstrating special products (i.e. antigens, toxins), components (individual nucleic acid sequences, protein fragments), or serologically detecting quality and quantity of antibodies produced against these compounds.
Microbiology examinations appear to establish activity of both infectology and clinical epidemiology, especially steps of infection control. Concerning diagnostic microbiology, the keystone remains detection of a living organism within another living organism, or in epidemiological application, also from the inanimate environment. For that reason, clinical microbiology cannot be automated completely and remains time-consuming. The importance of rapid identification of pathogens from septic patients is of utmost importance to allow the clinician to start appropriate antibiotic therapy or scale down the broad spectrum antibiotic treatment already in progress. Delay in reporting laboratory (including microbiology) results may have a fatal outcome, above all in diagnostics of hazardous infections. The development in technological background of laboratory sciences offers a more wide-ranging choice of molecular biology tools to help rapid and exact demonstration of several pathogens directly from clinical specimens or preliminary identification from the primoculture. A further responsibility of the microbiology expert is to evaluate the aetiological role of isolates before reporting. Typing and comparison of isolates of different patients, or of the same patients but from different samples, or from earlier periods of hospitalization, might clean nosocomial selection of several clones or permanent persistence of a strain within the patient. Comparison of molecular patterns of strains isolated from blood cultures, and from catheter tips (for example), is a rapid tool for the microbiologist to ascertain whether those were clinically relevant isolates or must be clarified as casual contaminants.
AIM
At Semmelweis University, due to centralization of diagnostic microbiology, operating a broad-spectrum clinical microbiology profile completed with multifunctional (i.e. rapid diagnostic and basic epidemiological) molecular biological service became practicable. Examples of the advantages of this complex laboratory background are presented in this paper.
Material and methodS
Culture
Miscellaneous clinical samples obtained from outpatients or patients admitted to university clinics, and, in addition, surveillance cultures and screening samples from admitted patients and staff members also were cultured on Bio-Rad culture media and were examined according to the latest pertinent methodology guidelines. Urine samples were cultured on UriSelect4 chromogenic agar plates (Bio-Rad) and were evaluated according to the manufacturer’s recommendations. Isolated bacteria were identified by the Micronaut (Merlin) system. Antibiotic sensitivity was determined by the disk diffusion method on Mueller-Hinton agar plates (Bio-Rad), according to the CLSI recommendations (1).
Every step of the microbiology examination was performed by the Central Clinical Microbiology Diagnostic Laboratory of Semmelweis University, Budapest.
Detection of methicillin-resistant Staphylococcus aureus (MRSA)
For MRSA screening, MRSASelect agar (Bio-Rad) was used. Isolates from blood agar or from Mueller-Hinton agar suspected MRSA were verified by Slidex MRSA Detection kit (bioMérieux). Directly from clinical samples, MRSA was detected by a real time PCR system using Xpert MRSA SSTI kits (Cepheid) within a 53-min running period, according to the manufacturer’s instructions.
Blood cultures
Blood culture flasks were incubated in Bact/Alert 240 system (bioMérieux). Flagged positive samples were examined microscopically after methylene blue and Gram staining, and were plated onto Columbia blood agar, Chocolate agar and Eosin-Methylene Blue agar plates (Bio-Rad). Streptococcal antigens, when it was indicated, were detected by Pastorex Strep latex agglutination kit (Bio-Rad) from supernatants of blood cultures.
Fluorescent in situ hybridization (FISH)
FISH-based bacterial identification (2) was performed directly on aliquots from positive specimens by the rapid BACTfish/BACTwave system (Izinta). Probes for identification were chosen based on the Gram staining result. A Eubacteria probe reactive to every bacterium served as the process control.
10 μl aliquots of ten-fold diluted blood cultures were transferred onto BACTfish Teflon covered slides and were dried at 45°C and fixed in a Bactwave microwave oven for 3 min. Permeabilization was carried out in cc methanol for 10 minutes.
In hybridization, tandem probes of a Gram negative sepsis kit (consisting of Enterobacteriaceae, Escherichia coli, Haemophilus influenzae, Klebsiella pneumoniae, Stenotrophomonas maltophilia, and Pseudomonas aeruginosa probes) and for identification of D group diplococci, Enterococcus faecalis and also E. faecium probes were used in ten-fold diluted solutions. A Eubacteria probe served as a positive (process) control. Incubation was completed in BACTwave for 16 min. Unbound probes were removed by washing plates in 30 ml of washing buffer at 47°C for 12 min, rinsed in tap water and methanol, and dried at 47°C for 5 min. Every field of plates was covered with 3 μl of antifade reagent, covered with a coverslip and examined with an epifluorescent microscope (Olympus) supplied with Cy3, and FITC filters.
Pulsed field gel electrophoresis (PFGE)
Isolates of the same species but different clinical source were compared by pulsed field electrophoresis (PFGE). PFGE of Enterococcus faecalis strains was performed in an agarose plug started from fresh blood agar cultures (3). Chromosomal DNA was digested by Sma I restriction endonuclease (BioLabs).
Lysis of Escherichia coli cells, setting off overnight cultures, was carried out in agarose blocks (4). DNA was digested with Xba I endonuclease (BioLabs).
For MRSA typing, genomic DNA was prepared (5) and digested with Sma I restriction enzyme (BioLabs).
Agarose gel electrophoresis of digested DNA samples was performed in the CHEF-DRII (Bio-Rad) system. Detection and evaluation was accomplished by the GelDoc 2000QuantityOne (Bio-Rad) gel documentation system. Lambda phage DNA and Staphylococcus aureus NCTC 8325 DNA were used as the molecular size control for E. faecalis, and digested Salmonella Branderup DNA for E. coli strains, as well.
Results
Case report 1
A 75-year-old female patient with previously diagnosed with Addison’s disease was admitted because of general deterioration, dyspnoea and weakness. Initial clinical, laboratory, and radiological investigations revealed no abnormal findings. Antibiotics were not administered. On the 3rd day of her hospitalization, the patient developed fever (38.6°C) and three pairs of blood cultures were obtained in twenty-minute intervals. Thorax X-ray performed on the same day was normal. Control X-ray on the 6th day after admission showed pneumonia in the right lower lobe.
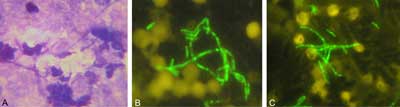
Both aerobic and anaerobic blood culture flasks turned out to be positive at the 10-12th hours of incubation. Microscopically, Gram negative, lengthened and swollen cells were observed with irregular form in size exceeding the bacterial range of size (fig. 1A). The internal control (Eubacteria probe) demonstrated bacterial infection (fig. 1B). The test performed with specific probes for sepsis pathogens showed a positive E. coli result (fig. 1C) within two hours after a positive signal of blood cultures was noticed. Based on this preliminary result, considering also the patient’s multiple antibiotic hypersensitivity, cefuroxime administration was initiated. The next day, the preliminary report was confirmed since coliform colonies were isolated and identified as E. coli. In the antibiotic sensitivity test, the isolate was sensitive to all tested antibiotics; the final result including antibiogram should be reported on the 3rd day of getting a positive signal.
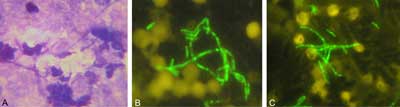
Fig. 1. Microscopic examination of positive blood culture of case 1. Light microscope, stained by methylene blue (A); Fluorescent in situ hybridization, reaction with Eubacteria probe (B) and Escherichia coli probe (C).
Due to the appropriate administration of intravenous cefuroxime, the patient’s condition significantly improved, having no fever. Although chest X-ray examination at the patient’s admission was negative, repeated image during the antibiotic treatment showed pneumonia in the right lower lobe. Seven days after the antibiotic initiation there were no infiltrates in lungs and the patient was discharged in a satisfactory condition.
Before taking blood cultures, antibiotics were not administered in the ward. According to the patient’s account, before her admission she had taken antibiotics sourced from a home reserve as she had done usually; therefore a prolonged post-antibiotic effect had to be considered. This assumption, namely formation of spheroplasts by the effect of a cell wall active antibiotic, would explain the irregular bacterial forms observed in microscopic slides from positive blood cultures.
Case report 2
A 64-year-old man, with a previous history of hypertension and type 2 diabetes mellitus, and of rectal cancer neoplasia, was admitted to the Department of Cardiology with the symptoms of a myocardial infarction for primary percutaneous coronary intervention (PCI).
During PCI, the right coronary artery was stented. The patient was in a satisfactory condition without signs of infection. On the third day of his hospital stay, extremely high temperature and shivering developed; serial blood cultures and urine cultures were obtained. Despite the combined antibiotic treatment (ceftriaxone and clarithromycin), the patient had septic shock with acute orthostatic hypotension, and kidney failure.
On the 3rd day, abdominal and pelvic ultrasound imaging were used to reveal the infection source. No abnormal findings on diagnostic imaging of liver, biliary tract, and pancreas were observed.
Size and structure of kidneys were average. On the right side, of the upper third, 7 mm echo-dense activity was detected. The pelvis showed a medium dilation.
The diagnosis of the ultrasound imaging was hepatosplenomegaly with presumptive nephrolithiasis and pyelectasis. The ultrasound performed one week later confirmed a medium-sized cavernous dilation.
The urologist indicated a right-sided ureter catheter implantation. Thereafter, strong diuresis was started. There was no stone, but debris was discharged through the catheter. Amoxycillin-clavulanic acid (3x 1.2 mg daily) was started after receiving the microbiology laboratory reports. Since he had no fever, leukocytosis and renal function parameters normalized and his condition was satisfactory after the ureteral catheterization and the antibiotic therapy, intravenous inotropic treatment was omitted.
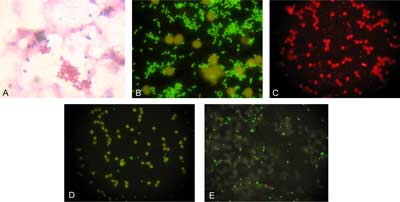
Gram positive diplococci and also Gram negative rods were observed in positive blood cultures. Supernatants of the flasks showed agglutination with Group D streptococcal reagent. The result of direct immunofluorescent microscopy suggested presence of both E. coli and E. faecalis (fig. 2 A, B, C, D, E). The preliminary result was immediately reported to the ward.
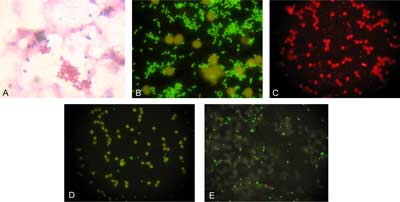
Fig. 2. Microscopic examination of positive blood culture of case 2. Light microscope (A); Fluorescent in situ hybridization (B-E). A: Gram staining; B: Eubacteria probe; C: Enterobacteriaceae probe; D: Escherichia coli probe; E: Enterococcus faecalis probe.
On the same day, E. coli and E. faecalis with 106 cfu/ml were isolated from urine culture of the patient. Comparing isolates of two sources by their antibiotic susceptibility patterns, they seemed to be identical: E. coli isolates were sensitive to semisynthetic penicillins, carbapenems, cephalosporins, fluoroquinolones, doxycycline, co-trimoxazole and also to aminoglycosides; and E. faecalis isolates were sensitive to amoxycillin, imipenem, vancomycin, ciprofloxacin, and intermediately to doxycycline, besides demonstrating a low rate of resistance to gentamicin. During the judicious amoxycillin/clavulanic acid therapy started with knowledge of the microbiology results, the patient’s parameters normalized and on the fifth day his sepsis was cured.
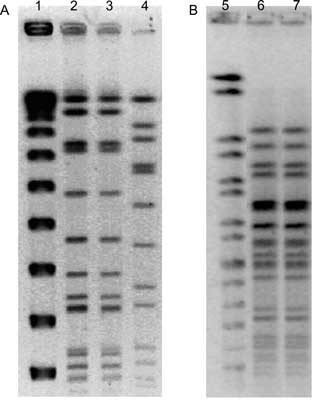
By molecular comparison of DNA, samples served for clearing the hypothetical relation between isolates sourced from blood and urine (fig. 3). DNA fingerprints of strains originating from different clinical specimens proved to be identical. Results of molecular typing of isolates confirmed acute pyelonephritis as the focus of sepsis.
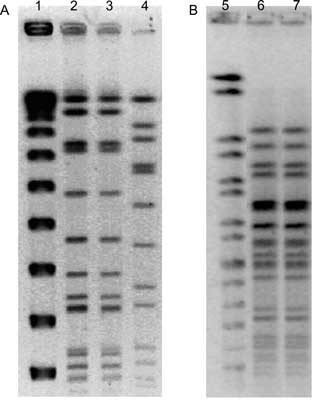
Fig. 3. Comparison of macrorestriction profiles of Enterococcus faecalis (A) and Escherichia coli (B) strains sourced from blood and urine cultures. Pulsed field gelelectrophoresis.
Legends: 1. Lambda phage DNA (control); 2. Enterococcus faecalis (urine); 3. Enterococcus faecalis (blood); 4. Staphylococcus aureus NCTC 8325 (control); 5. Salmonella Branderup DNA (control); 6. Escherichia coli (urine); 7. Escherichia coli (blood).
Case report 3
A 63-year-old male patient was readmitted to the Department of Vascular and Cardiac Surgery with a postoperative wound infection. In his previous history, he underwent aorto-bifemoral (Dacron) bypass surgery 3 months earlier. After the positive MRSA report, the graft was removed; the patient was discharged without signs of infection. As he had fever 5 weeks after discharge he was re-admitted. MRSA screening tests (throat, nose) by a conventional (culture) method were negative. During his observation, he had no fever but inflammatory parameters were high and he complained of growing back pain. The periaortic abscess was surgically debrided. His conditions stabilized in the postoperative period. On the 6th postoperative day, MRSA was detected from the abdominal abscess by RT-PCR, and also by simultaneous culture, E. coli, Klebsiella pneumoniae and Candida albicans were isolated. On the 10th postoperative day he suddenly died. The most probable cause of death was gastrointestinal bleeding originating from gastric ulcer of aorto-enteral fistula.
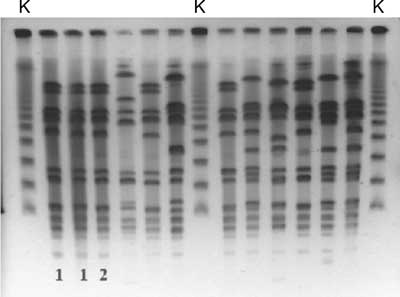
Genetic fingerprinting
Comparison of MRSA strains isolated from his abdominal abscess and graft two months earlier, and of that obtained during his second hospitalization at the teaching hospital, was carried out by PFGE technique. Figure 4 demonstrates that patterns of the two isolates of the patient are identical but they differ from the MRSA isolates sourced from other patients in the same period.
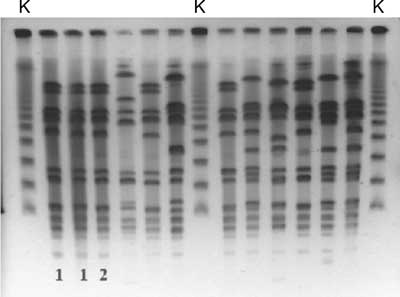
Fig. 4. Pulsed field gelelectrophoretic (PFGE) image of methicillin resistant Staphylococcus aureus strains isolated from inpatients of the Department of Vascular and Cardiac Surgery, Semmelweis University, Budapest.
Legends: 1: BM wound, 20/07/2007; 2: BM wound, 14/09/2007; K: molecular mass control.
Discussion
Diagnosis of sepsis
As an extreme manifestation of a blood stream infection sepsis is a serious clinical condition, associated with high mortality, greater in patients with septic shock (40-70%) than in those with sepsis alone (25-30%) (6-8). According to the consensus conference description, sepsis is defined as systemic inflammatory response syndrome (SIRS) due to presumed or confirmed infection (7). In most cases, sepsis is a consequence of a local infection, giving pathogens an opportunity to enter the bloodstream, and cause systemic disease, with tachypnoea, tachycardia, fever or hypothermia.
Septic patients may present with a variety of signs and symptoms. Diagnosis of sepsis requires complex approaches, including physical examination, search for signs of organ dysfunction and the possible source of infection, along with various laboratory tests, defining serum levels of biomarkers indicating serious inflammation, such as leucocyte count and acute phase reactants. Blood cultures have a central role in diagnosis of bloodstream infections and confirmation of the microbial origin of the SIRS.
Rapid diagnosis of sepsis is of utmost importance, reducing mortality and length of hospitalization (8, 9). Because of the need for quick determination possibilities, several biomarkers, such as the acute-phase protein CRP (C-reactive protein), the level of which rises in the blood in response to inflammation, procalcitonin and activated partial thromboplastin time, are studied extensively as well (10, 11). These markers can indicate patients with sepsis among critically ill patients. However, blood cultures still remain the gold standard for detection of the causative pathogen and determination of the antibiotic sensitivity of the isolate, eventually for choosing a judicious therapy. A recent article underlined the importance of early adequate therapy versus empirical treatment: the mortality rate was 67.8% for those patients who received inadequate therapy at admission to the intensive care unit, in contrast with 28.7% mortality of the matched control group (12).
Microbiology testing of blood
In the past years, new molecular techniques have emerged for the detection of bloodstream infections, based on identification of bacterial and fungal antigens or nucleic acid fragments of the pathogens by various amplification and hybridization methods (13). However, these methods have some drawbacks, such as excessive specificity: most of the molecular techniques will only detect a narrow spectrum of pathogens, determining only the presence (or absence) of the questioned bacterium in the blood. In contrast, blood cultures have low specificity, and high sensitivity, allowing detection of all microorganisms which may be present in the patient’s blood, and able to grow under the given conditions. By combining the two approaches their advantages add together: examination of flagged positive blood cultures with specific molecular techniques based on the microscopic morphology of the detected microorganisms enables rapid and specific determination of sepsis pathogens, enhancing early adequate therapy and improving prognosis of the disease.
Microbiology testing of blood samples is extremely sensitive to both clinical and laboratory conditions. If the patient received antimicrobial treatment before the sample for culture was taken, due to the presence of the drug the result of culture would be misleading: antibiotics might kill or repress microorganisms, or especially in the presence of cell wall active antibiotics such as beta-lactam or glycopeptide derivatives irregular forms – protoplasts or spheroplasts – would be produced. These bacterial forms surrounded by only cell membrane are extremely sensitive to the milieu; due to the osmotic pressure lysis of the cell occurs. These forms were detectable in blood cultures of our first patient. The early report followed only one hour after noticing positive a signal resulted not only in immediate administration of adequate therapy but it would be possible that lysis of spheroplasts yielded a false negative culture result on solid media for a longer incubation period.
Blood cultures have been indicated on the occasion of serious, life-threatening infections such as sepsis, pneumonia and meningitis. This underlines the significance of development of rapid diagnostic tools. The FISH method utilizes specific binding of fluorescent labelled oligonucleotide probes to target sequences situated on ribosomal RNA (2). While ribosomes exist in high copy numbers in dividing bacterial cells, during the logarithmic period, an amplification step – as in PCR – is not required for FISH. Ten microorganisms in a field is regarded as a practical limit of detection in this test. The Eubacteria probe applied as an internal (positive) control is specific to highly conservative sequences of rRNA; therefore they can detect every bacterium. Because dead bacterial cells contain no detectable ribosomal RNA, in contrast to PCR, here only living (dividing) cells show a positive reaction which yields low incidence of false positivity.
The FISH method has been used in pathology, oncology, genetic diagnostics and for examination of structural chromosome aberrations, but for microbiology, DeLong and colleagues adapted it first (14). It is used more extensively to diagnose patients with sepsis, meningitis, wound infections or cystic fibrosis – especially when the need for rapid diagnosis is increased (15, 16). Detection time has been markedly (to only one hour) reduced using a special microwave oven for the hybridization step (2).
In our experience, the FISH method proved to be a helpful complementary test when identification determines the choice of therapy, when culture is not quick enough or is problematic, or the result is doubtful. Results of immunofluorescence have been reported only as preliminary information and culture as a gold standard is not replaceable.
Source of sepsis
Multibacterial sepsis, i.e. presence of more than one relevant bacterial strain in one blood culture, occurs rarely, usually in an immunocompromised situation or in samples from patients who are in the final stage. In case 2, diabetes and antitumour chemotherapy, as immunosuppressive factors, might contribute to the development of the septic stage. Blood and urine cultures yielded identical strains of E. coli, and E. faecalis, as well. The simultaneous incidence of two bacterial pathogens in his blood cultures was ascribed to this clinical situation.
Approximately 20-30% of hospital acquired sepsis cases are estimated to originate from the urogenital tract (17). The concept of urogenital sepsis expands from asymptomatic bacteriuria to acute pyelonephritis related sepsis (18). In more than 50% of cases E. coli is the pathogen; in development and also in outcome of infection, virulence factors of the species, namely hemolysin production, adhesive fimbriae, iron binding systems, K-capsular antigen and toxins, are decisive.
Urosepsis developing from pyelonephritis, in particular due to E. coli, occurs relatively frequently. Age (19) and primary biliary cirrhosis (20, 21) may contribute to the development of infection as predisposing factors in most cases. On the other hand, it is very rare that more than one bacterium is responsible for the infection, and etiological clarification of these cases is not free of difficulties.
To appreciate the clinical significance of urinary isolates is subjective. In ascending lower tract infections, Enterobacteriaceae species, most frequently E. coli, and also enterococci derived from enteral flora, predominate (18). They usually cause monoinfection in cases of cystitis, and quantitatively, more than 105 cfu occur in millilitres of the spontaneously evacuated urine. On the other hand, the same species would contaminate urine samples collected without keeping the rules of specimen collection and personnel hygiene sourced from outer genitals. If more than one microorganism of possible enteral origin appears in high colony number in a urine culture it is usually regarded as contamination.
The phenomenon that the same species were isolated from blood and urine samples collected on the same day of the second patient indicated detailed comparison of the isolates. Molecular biological comparison is considered the “gold standard” in this respect. PFGE yields an individual pattern characteristic of every cell line; identical “fingerprint” means unambiguous identity of the tested strains (22-24). It was documented in our case comparing isolates from blood and urine. Over and above that, this method can be used for propping up clinical relevance of occasional isolates: an identical pattern of coagulase negative staphylococcal isolates from blood cultures and intravascular catheter tips confirms their pathogenic role but a difference in fingerprints precludes it (22, 24).
Advantages of molecular techniques
Application of molecular methods in clinical microbiology practice facilitates rapid and exact detection and identification of pathogens either in culture or directly in specimens, and helps in detecting foci of infections or in verifying the clinical relevance of isolates by comparing them. For these reasons they are valuable accessories of the efficient diagnostic background of infectious diseases.
To treat systemic S. aureus infections only cell wall active antibiotics, i.e. penicillins or glycopeptides, would be administered. In management of MRSA sepsis, because of the complete cross-resistance between beta-lactams, there is no choice but to take glycopeptides (25). Because of the double mortality observed by glycopeptide treated patients compared to the oxacillin treated control group (26), early information on MRSA colonization or infection falls under the most considerable demands of the microbiology laboratory.
Spread of MRSA would be limited by hand hygiene regulations but its emergence can be prevented only by systemic and regular screening of both staff and newly admitted patients (27, 28). For forestalling horizontal transmission of an MRSA clone, a combination of traditional and molecular biology methods has been used. Performing screening tests by traditional culture methods or using chromogenic agar plates yields results within 48-72 hours. To confirm the suspected MRSA colonies, application of PBP2’ specific tests, detecting altered transpeptidase in penicillin-resistant cell wall is recommended. Likewise, detection of the mecA gene encoding for PBP2’ production by PCR could be used to verify MRSA identification as a reference method (29, 30) but is insufficient to apply for direct detection of MRSA in swabs (31). For manifestation of methicillin resistance in the phenotype, functioning of fem factors (factor essential for methicillin resistance) is also essential. Accordingly, simultaneous detection of mecA and fem yields a more exact detection (32, 33). As these genes appear also in methicillin-resistant coagulase negative staphylococci, validation of MRSA should be completed with detection of the nucA gene responsible for S. aureus-specific heat stable deoxyribonuclease production (33). This combination of amplification tests is not applicable for direct identification of MRSA from clinical samples or from screening tests because simultaneous presence of a methicillin-susceptible S. aureus (nucA) and a methicillin-resistant CNS (mecA) results in positivity with both tests and would be interpreted as a positive (false positive) test (34).
The most efficient tools for direct detection of MRSA are considered real time PCR or immunomagnetic separation of methicillin-resistant cells following a short pre-incubation in an enrichment broth selective for MRSA (27, 35). In our practice, GeneXpert (Cepheid) has been used for direct identification of MRSA in clinical samples when it was indicated. GeneXpert is dedicated to demonstrating SCCmec (staphylococcal cassette chromosome mec) in a real time PCR cartridge with a sensitivity of 95% (36, 37). Reaction time is 53-75 min, depending on the test chosen.
Indications of the test are estimated as follows (38-40):
– Screening for MRSA carrier in high-risk patient groups, before admission to intensive care units;
– Rehospitalization of a patient with an anamnestic MRSA infection;
– Ventilator-associated pneumonia; S. aureus bacteraemia, catheter related sepsis, prosthetic valve endocarditis;
– Presumably S. aureus caused soft tissue infection in non-immunocompromised host;
– Infections developed in connection with an MRSA endemic;
– Every other situation indicated by an infectious disease specialist.
Efficacy of rapid diagnostic and screening test as well as molecular biology applications in clinical laboratory practice is well documented (27, 38, 41, 42). Considering the whole costs of hospitalization, cost-benefit calculations show rapid economic benefit of molecular methods because judicious therapy can be started earlier.
The raison d’être of simultaneous performance of classical microbiology examinations and also rapid tests needs no explaining. Traditional culture methods are cheaper but yield results in days; therefore they are used for MRSA screening of occupational indication (labour hygiene) or before vascular or elective orthopaediatric surgery. PCR based tests are indicated in associated cases with critical care admission, cardiac surgery, and emergency orthopaedic surgery, as well (42).
Good examples for the beneficial scope of molecular methods and rapid diagnostics are provided by the results of case 3. The patient was earlier found to be MRSA positive as MRSA was isolated from his wound sample during his hospital stay in July 2007. Following a judicious vancomycin treatment, he was discharged in a stage apparently cured. Two months later, at the time of his readmission, a PCR screening test was performed, according to the recent protocol, which yielded a positive result. Antibiogram of the S. aureus strain isolated from the simultaneous culture was identical to those of the previous one. Comparing these isolates by PFGE, they proved to be identical but both differed significantly from all of the MRSA isolates existing in the same period at the hospital. By molecular typing it could be demonstrated that there was no direct infection of the patient by a new strain but he was re-infected by his own former pathogen, which involves different epidemiological and legal consequences.
Molecular tools have been indispensible elements of the recent clinical microbiology. In situ performed hybridization and PCR tests directly from the specimen or from the blood culture flask provide a preliminary report through identification of the pathogens, and this could be a guide to start an appropriate anti-infective therapy (9, 43-45). The multifactorial comparison of bacterial and fungal isolates gives no prompt answer but in absence of typing tests, microbiology results could not be or could not unequivocally be interpreted occasionally. Accordingly, every microbiology department should endeavour to provide for prompt availability of examinations of this sort either on the spot or in partnership.
CONCLUSION
It is indispensable that a diagnostic laboratory maximally fulfils its responsibility in the management of infectious diseases. Quick and accurate demonstration of pathogens from clinical specimens must be a duty of the same significance as prediction or identification of health care associated epidemiological events is. Traditional microbiology methods such as microscopy, culture, manual identification by visually evaluated tests and antibiotic sensitivity testing methods could not be or only partially be done by automated (instrumented) tools. However, the scope of (automated) molecular methods could be set even in daily diagnostic applications if the accuracy of laboratory activity and also cost-effectiveness of the medical attendance could be extended. It is self-evident that a laboratory department applies all diagnostic tools and examination profiles which are claimed and are beneficial for patients’ management because running costs are covered from the same budget. A problematic situation occurs when a diagnostic supplier does not organizationally or financially belong to the hospital or institute directly responsible for the patients’ care. In this case, reimbursement of the diagnostic services is reached between the supplier and the owner/operator realized by a bilateral agreement. It follows that preferences would differ and financing would be realized with a strong influence of health insurance and moderated by local interests, namely implicitly must keep thrift in view, i.e. should be profitable.
In an effective health care system, the indicator of the effectiveness is the efficiency of healing. This could be converted into practice by contracts with health insurance companies, and, on the other hand, result in a decrease of functioning charges, by reducing antibiotic costs, hospitalization days and the frequency of suing for damages.
Acknowledgements
The authors are indebted to doctors Jeannette Molnár, Ildikó Adler (2nd Department of Internal Medicine, Semmelweis University) and Gábor Kerecsen (Department of Cardiology, National Medical Center, Budapest) for their help in compiling case reports, to Dr. Andrea Horváth (Institute of Medical Microbiology, Semmelweis University, Budapest) for her assistance in immunofluorescent microscopy, and to Dr. Ivelina Damjanova (Department of Bacteriophage and Molecular Typing, National Institute for Epidemiology, Budapest) for her advice in pulsed field electrophoresis.
Piśmiennictwo
1. Clinical and Laboratory Standards Institute: Performance Standards for Antimicrobial Susceptibility Testing 2007; Seventeenth Informational Supplement: M100-S17, CLSI, Wayne PA. 2. Peters RPH, van Agtmael MA, Simoons-Smit AM et al.: Rapid identification of pathogens in blood cultures with a modified fluorescence in situ hybridization assay. J Clin Microbiol 2006; 44: 4186-4188. 3. Leonard RB, Carroll KC: Rapid lysis of Gram-positive cocci for PFGE using acromopeptidase. Diagn Mol Pathol 1997; 5: 288-291. 4. Gautom RK: Rapid pulsed-field gel electrophoresis protocol for typing of Escherichia coli O157:H7 and other Gram-negative organisms in 1 day. J Clin Microbiol 1997; 35: 2977-2980. 5. Matthews KR, Jayarao BM, Oliver SP: Restriction endonuclease fingerprinting of genomic DNA of Staphylococcus species of bovine origin. Epidemiol Infect 1992; 109: 59-68. 6. Lever A, MacKenzie I: Sepsis: definition, epidemiology and diagnosis. Brit Med J 2007; 335: 879-883. 7. Bone RC, Balk RA, Cerra FB et al.: Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992; 101: 1644-1655. 8. Daniels R: Surviving the first hours in sepsis: getting the basics right (an intensivist’s perspective). J Antimicrob Chemother 2011; 66 (Suppl 2): ii11-ii23. 9. Beekmann SE, Diekema DJ, Chapin KC Doern GV: Effects of rapid detection of bloodstream infections on length of hospitalitalization and hospital charges. J Clin Microb 2003; 41: 3119-3125. 10. Moreira VG, Prieto B, San Martín Rodrígez J, Álvarez FV: Usefulness of cell-free plasma DNA, procalcitonin and C-reactive protein as markers of infection in febrile patients. Ann Clin Biochem 2010; 47: 253-258. 11. Riedel S, Melendez JH, An AT et al.: Procalcitonin as a marker for the detection of bacteremia and sepsis in the emergency department. Am J Clin Pathol 2011; 135: 182-189. 12. Garnacho-Montero J, Ortiz-Leyba C, Herrera-Melero I et al.: Mortality and morbidity attributable to inadequate empirical antimicrobial therapy in patients admitted to the ICU with sepsis: a matched cohort study. J Antimicrob Chemother 2008; 61: 436-441. 13. Wellinghausen N, Siegel D, Winter J, Gebert S: Rapid diagnosis of candidaemia by real-time PCR detection of Candida DNA in blood samples J Med Microbiol 2009; 58: 1106-1111. 14. DeLong EF, Wickham GS, Pace NR: Phylogenetic stains: ribosomal RNA-based probes for the identification of single bacterial cells. Science 1989; 243: 1360-1363. 15. Hogardt M, Trebesius K, Geiger AM et al.: Specific and rapid detection by fluorescent in situ hybridization of bacteria in clinical samples obtained from cystic fibrosis patients. J Clin Microb 2000; 38: 818-825. 16. Peters RPH, van Agtmael MA, Danner SA et al.: New developments in the diagnosis of bloodstream infections. Lancet Inf. Dis 2004; 4: 751-760. 17. Naber KG: Urogenital infections: The provital role of the urologist. Eur Urol 2006; 50: 657-659. 18. Rouschop K, Florquin S: CD44 in renal disease: friend or foe. PhD thesis, the Academic Medical Centre in Amsterdam, the Netherlands, 2006; http://www.nieronline.org/index.php?title=CD44_in_renal_disease:_friend_or_foe 19. Kojima C, Yumura W, Itabashi M et al.: A case of microscopic polyangitis with sepsis due to pyelonephritis. Nippon Jinzo Gakkai Shi 2005; 47: 876-881. 20. Rocha E, Soares M, Valente C et al.: Outcomes of critically ill patients with acute kidney injury and end-stage renal disease requiring renal replacement therapy: a case-control study. Nephrol Dial Transplant 2009; 24: 1925-1930. 21. Ohno N, Ota Y, Hatakeyama S et al.: A patient with E. coli-induced pyelonephritis and sepsis who transiently exhibited symptoms associated with primary biliary cirrhosis. Intern Med 2003; 42: 1144-1148. 22. Krediet TG, Mascini EM, van Rooij E et al.: Molecular epidemiology of coagulase-negative staphylococci causing sepsis in a neonatal intensive care unit over an 11-year period. J Clin Microbiol 2004; 42: 992-995. 23. Murono K, Hirano Y, Koyano S, Ito K, Fujieda K: Molecular comparison of bacterial isolates from blood with strains colonizing pharynx and intestine in immunocompromised patients with sepsis. J Med Microbiol 2003; 52: 527-530. 24. Worthington T: Is hospital-acquired intravascular catheter-related sepsis associated with outbreak strains of coagulase-negative staphylococci? J Hosp Infect 2002; 46: 130-134. 25. Rahman M: Alternatives to vancomycin in treating methicillin-resistant Staphylococcus aureus infection. J Antimicrob Chemother 1998; 41: 325-328. 26. Kim S-H, Kim K-H, Kim H-B et al.: Outcome of vancomycin treatment in patients with methicillin-susceptible Staphylococcus aureus bacteremia. Antimicrob Agents Chemother 2008; 52: 192-197. 27. Paule SM, Pasquariello AC, Hacek DM et al.: Direct detection of Staphylococcus aureus from adult and neonate nasal swab specimens using real-time polymerase chain reaction. J Mol Diagn 2004; 6: 1 91-196. 28. Raboud JR, Saskin A, Simor M: Modeling transmission of methicillin-resistant Staphylococcus aureus among patients admitted to a hospital. Infect Control Hosp Epidemiol 2005; 26: 607-615. 29. Brakstad OG, Maeland JA, Tveten Y: Multiplex polymerase chain reaction for detection of genes for Staphylococcus aureus thermonuclease and methicillin resistance and correlation with oxacillin resistance. Acta Path Micro I M B 1993; 101: 681-688. 30. Brown DF, Edwards DI, Hawkey PM: Guidelines for the laboratory diagnosis and susceptibility testing of methicillin-resistant Staphylococcus aureus (MRSA). J Antimicrob Chemother 2005; 56: 1000–1018. 31. Olsson-Liljequist B, Larsson P, Walder M, Miöner H: Antimicrobial susceptibility testing in Sweden. III. Methodology for susceptibility testing. Scand J Infect Dis Suppl 1997; 105: 13-23. 32. Jonas D, Grundmann H, Hartung FD: Evaluation of the mecA femB duplex polymerase chain reaction for detection of methicillin-resistant Staphylococcus aureus. Eur J Clin Microbiol Infect Dis 1999; 18: 643-647. 33. Louie L, Goodfellow J, Mathieu P, Glatt A, Louie M, Simor AE: Rapid detection of methicillin-resistant staphylococci from blood culture bottles by using a multiplex PCR assay. J Clin Microbiol 2002; 40: 2786–2790. 34. Levi K, Towner KJ: Detection of methicillin-resistant Staphylococcus aureus (MRSA) in blood with the EVIGENE MRSA detection kit. J Clin Microbiol 2003; 41: 3890–3892. 35. OHara S: Novel rapid culture-based detection method for methicillin-resistant Staphylococcus aureus. J Clin Microbiol 2008; 46: 3181–3182. 36. Hanssen A-M, Sollid JUE: Multiple staphylococcal cassette chromosomes and allelic variants of cassette chromosome recombinases in Staphylococcus aureus and coagulase-negative staphylococci from Norway. Antimicrob Agents Chemother 2007; 51: 1671-1677. 37. Wren MWD, Carder C, Coen PG et al.: Rapid molecular detection of methicillin-resistant Staphylococcus aureus. J Clin Microbiol 2006; 44: 1604-1605. 38. Granato PA: The impact of same-day tests versus traditional overnight testing. Diagn Micr Infec Dis 1993; 16: 237-243. 39. Brown DF, Edwards DI, Hawkey PM et al.: Guidelines for the laboratory diagnosis and susceptibility testing of methicillin-resistant Staphylococcus aureus (MRSA). J Antimicrob Chemother 2005; 56: 1000-1018. 40. Henderson DK: Managing methicillin-resistant staphylococci: a paradigm for preventing nosocomial transmission of resistant organisms. Am J Med 2006; 119(Suppl. 1): S45-S52. 41. Bootsma MC, Diekmann O, Bonten MJ: Controlling methicillin-resistant Staphylococcus aureus: quantifying the effects of interventions and rapid diagnostic testing. Proc Natl Acad Sci USA 2006; 103: 5620-5625. 42. Cunningham R, Jenks P, Northwood J, Wallis M, Ferguson S, Hunt S: Effect on MRSA transmission of rapid PCR testing of patients admitted to critical care. J Hosp Infect 2007; 65: 24-28. 43. Kempf VA, Trebesius K, Autenrieth IB: Fluorescent in situ hybridization allows rapid identification of microorganisms in blood cultures. J Clin Microbiol 2000; 38: 830-838. 44. Peters RPH, van Agtmael MA, Danner SA, Savelkoul PHM, Vandenbroucke-Grauls CMJE: New developments in the diagnosis of bloodstream infections. Lancet Inf Dis 2004, 4: 751-760. 45. Tsalik EI, Jones D, Nicholson B et al.: Multiplex PCR to diagnose bloodstream infections in patients admitted from the emergency department with sepsis. J Clin Microbiol 2010; 48: 26-33.