© Borgis - New Medicine 3/2014, s. 89-91
*Konrad Wroński1, 2
Giant uterine leiomyoma – case report and review of literature
1Department of Oncology, Faculty of Medicine, University of Warmia and Mazury, Olsztyn, Poland
Head of Department: prof Sergiusz Nawrocki, MD, PhD
2Department of Surgical Oncology, Hospital Ministry of Internal Affairs with Warmia and Mazury Oncology Centre, Olsztyn, Poland
Head of Department: Andrzej Lachowski, MD
Summary
Uterine leiomyomata are the most common gynecological benign tumors arise from the smooth muscle cells of the myometrium. The pathogenesis of fibroids is still unclear. Leiomyomas are found in more than half of women over age 35. About 70% of Caucasian women and 80% of African American women have uterine leyomyomata above 50 years of age. Most of patients have small uterine leiomyoma. Giant uterine leiomyoma with cystic degeneration are exceedingly rare and can be mistaken for ovarian or retroperitoneal cysts and neoplasmatic tumor.
The author of this article presented a case of a 63-year-old Caucasian woman who was admitted to the hospital because of giant uterine leiomyomata which mimicking a huge ovarian malignancy and cause torsion. The patient underwent radical abdominal hysterectomy and bilateral salpingoophorectomy without complication. The author performed a literature review on giant uterine leiomyomata treatment.
INTRODUCTION
Uterine leiomyomata are the most common gynecological benign tumors arise from the smooth muscle cells of the myometrium (1-3). The pathogenesis of fibroids is still unclear (2, 3). Leiomyomas are found in more than half of women over age 35 (1-4). About 70% of Caucasian women and 80% of African American women have uterine leyomyomata above 50 years of age (5). Most of patients have small uterine leiomyoma (5, 6). Giant uterine leiomyoma with cystic degeneration are exceedingly rare and can be mistaken for ovarian or retroperitoneal cysts and neoplasmatic tumor (6, 7).
CASE REPORT
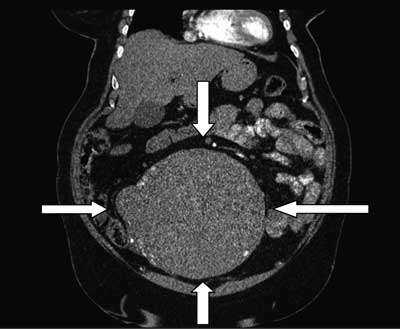
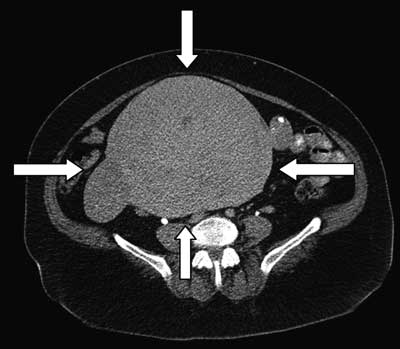
A 63-year-old Caucasian woman was referred to the Department of Surgical Oncology due to giant pelvic tumor diagnosed in computer tomography scan (fig. 1, 2). The computed tomography scan revealed cystic-solid polycyclic mass adherent to the stem of the uterus, which after intravenous injection of contrast agent underwent strengthening mainly within the peripheral solid tumors. The largest transverse dimension at the level of iliac was 242 x 173 millimeters. Tumor mass extended from the level of the lower edge of the right lobe of the liver to the upper wall of the bladder, the peripheral outline of polycyclic calcification were visible. In the adnexal revealed no changes. The bladder was thin-walled. In the other organs of the abdomen, there were no focal lesions. The lymph nodes were not enlarged during the scope examined. In bones, there were no lesions suspected of metastasis. The basal layer of both lungs were unchanged.
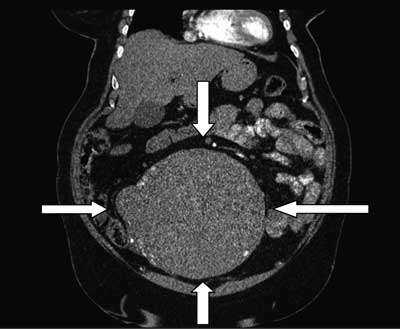
Fig. 1. The computed tomography scan showing cystic-solid polycyclic mass adherent to the stem of the uterus.
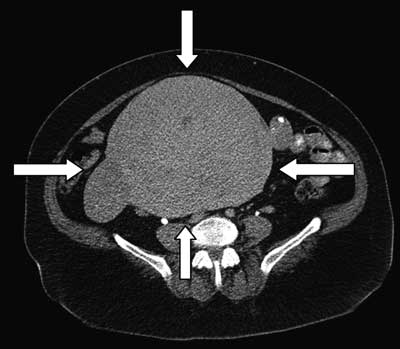
Fig. 2. The computed tomography scan showing giant uterine fibroid tumor which the largest transverse dimension at the level of iliac was 242 x 173 millimeters.
The patient suffered from abdominal pain located in the the mesogastric and the lower abdomen area, she had distension and constipation for a period of 16 months. Physical examination showed palpable tumor located in the mesogastric and the lower abdomen area. There were no peritoneal symptoms. The external genitalia and uterine cervix were normal. Her vital signs were all within normal limits. There was no histopathological examination of the fine-needle aspiration biopsy before planned surgery.
She had no any other symptoms, there was no history of weight loss and loss of appetite. The patient was treated chronically due to diabetes and arterial hypertension. She had no surgeries and there was no history of carcinoma in patient family. Blood test and other routine hematological examinations and biochemical tests were within normal limits.
Considering the size of the tumor and the possibility of malignancy, a radical abdominal hysterectomy and bilateral salpingoophorectomy was performed (Figure 3 and 4). The time of surgery was about 120 minutes. Patient after surgery felt good and did not complain of pain.

Fig. 3. Laparotomy material showing giant leiomyoma.

Fig. 4. Photo taken during surgery showing giant fibroid uterus.
Histopathology examination of a huge tumor showed uterine leiomyomata with cystic degeneration. The postoperative period was uncomplicated and the patient left the ward in the 6th day after surgery.
DISCUSSION
Leiomyoma of the uterus is the most common benign tumor of the female pelvis arise from the smooth muscle cells of the myometrium (1-3). The pathogenesis of fibroids is still unclear but it seems that hormonal stimulation by estrogen and possibly progesterone plays an important role (2, 3).
Leiomyomas are found in more than half of women over age 35 but also can be present in females under the age of 20 (8). Wisot and colleagues described the first case of bleeding from uterine myoma in a 13-year-old girl in 1969 (9). Augensen decribed myoma in 15-year-old girl who suffered from heavy menstruation, pain and uremia (10). The largest uterine fibroid ever reported in the medical literature weighed 63.3 kg and was removed postmortem in 1888 (11).
Based on leiomyomas location they are classified as submucosal, intramural or subserozal (12). Clinical symptoms of the large myoma are: pain, distension, constipation, occurring more often menstrual bleeding and micturation and reproduction affect (2-6). When uterine fibroids enlarge there are observed different types of degeneration such as hyaline, cystic, myxoid or red degeneration and dystrophic calcification (13). Hyaline degeneration is the most common and is observed in up to 60% cases of leiomyomas (14). Cystic degeneration is observed in about 4% of fibroids (14).
Typical appearances of leiomyomas are easily detected on ultrasound imaging. In the vast majority cases, transvaginal or through the abdomen ultrasound is usually the initial tool for diagnosis of uterine myoma (15). Magnetic resonance imaging accurately shows location and number of leimyomas (15). Chopra and colleagues reported that diagnostic accuracy for USG and MRI are 73% and 100% respectively (15). The computed tomography scan is useful tool to diagnose cases of fibroids with necrosis complication and malignant transformation (13, 15).
The treatment of uterine fibroids may involve one of the following approaches or a combination thereof: expectant management, surgical management, medical management, myolysis management and selective uterine artery embolization (11, 12). The chosen approach should be individualized for every patient. Nowadays a surgical management is the most frequent preferred. But it is important to treat women with large leiomyomas in high specialized gynecological or oncological surgery departments.
CONCLUSIONS
1. Giant uterine leiomyomas are exceedingly rare.
2. Clinical symptoms of the large myoma are: pain, distension, constipation, occurring more often menstrual bleeding and micturation and reproduction affect
3. Transvaginal or through the abdomen ultrasound is usually the initial tool for diagnosis of uterine myoma.
4. The chosen treatment should be individualized for every patient.
5. Women with large leiomyomas should be treated in high specialized gynecological or oncological surgery departments.
Piśmiennictwo
1. Cramer S, Patel A: The frequency of uterine leiomyomas. Am J Clin Pathol 1990; 94: 435-438. 2. Gupta S, Manyonda I: Acute complications of fibroids. Best Pract Res Clin Obstet Gynaecol 2009; 23: 609-617. 3. Tsai Y, Yeats S, Jeng C, Chen S: Torsion of a uterine leiomyoma. Taiwan J Obstet Gynecol 2006; 45: 333-335. 4. Tordera A, Bello T, Bouteiller J: Acute abdomen casued by calified pediculated myoma. Dia Med 1952; 24: 1523-1524. 5. Adams Hillard PJ: Benign diseases of the female reproductive tract. [In:] Berek JS, ed. Berek and Novak’s gynecology. 14th ed. Philadelphia: Lippincott and Williams, 2007: 463-469. 6. Vandermeer FQ, Wong-You-Cheong JJ: Imaging of acute pelvic pain. Clin Obstet Gynecol 2009; 52: 2-20. 7. Roy C, Bierry G, El Ghali S et al.: Acute torsion of uterine leiomyoma: CT features. Abdom Imaging 2005; 30: 120-123. 8. Fields KR, Neinstein LS: Uterine myomas in adolescents: case reports and a review of the literature. J Pediatr Adolesc Gynecol 1996; 9: 195-198. 9. Wisot AL, Neimand KM, Rosenthal AH: Symptomatic myoma in a 13-year-old girl. Am J Obstet Gynecol 1984; 105: 639-641. 10. Augensen K: Uterine myoma in a 15-year-old girl. Acta Obstet Gynecol Scand 1981; 60: 591. 11. Evans III AT, Pratt JH: A giant fibroid uterus. Obstet Gynecol 1979; 54: 385-386. 12. Novak ER, Woodruff JD: Myoma and other benign tumors of uterus. [In:] Novak ER, Woodruff JD editors. Novak’s gynecologic and obstetric pathology. Philadelphia: WB Saunders 1979: 260-267. 13. Preayson RA, Hart WR: Pathologic considerations of uterine smooth muscle tumors. Obstet Gynecol Clin North Am 1995; 22: 637-657. 14. Mayer DP, Shipilov V: Ultrasonography and magnetic resonance imaging of uterine fibroids. Obstet Gynecol Clin North Am 1995; 22: 667-725. 15. Chopra S, Lev-Toaff AS, Ors F, Bergin D: Adenomyosis: common and uncommon manifestations on sonography and magnetic resonance imaging. J Ultrasound Med 2006; 25(5): 617-627.