*Aneta Obcowska1, Małgorzata Kołodziejczak2
The limitations and difficulties of anal ultrasonography in diagnosis of anal fistulae
Ograniczenia i trudności ultrasonografii przezodbytniczej w diagnostyce przetok odbytu
1Department of General and Oncological Surgery with the Subunit of Vascular Surgery, Lord’s Transfiguration Hospital, Warsaw
Head of Department: Professor Mariusz Frączek, MD, PhD
2Warsaw Proctology Centre, Saint Elizabeth’s Hospital, Mokotów Medical Centre
Head of Centre: Associate Professor Małgorzata Kołodziejczak, PhD
Streszczenie
Klasyczne leczenie operacyjne przetoki odbytu związane jest nie tylko z dużym odsetkiem nawrotów, ale także z gorzej tolerowanym przez pacjentów powikłaniem, jakim jest pogorszenie trzymania stolca i gazów.
Anatomiczny przebieg kanału w stosunku do mięśni zwieraczy w połączeniu z wynikami badań czynnościowych stanowią najważniejsze elementy decydujące o wyborze techniki operacyjnej. W realiach polskich bardziej dostępna niż rezonans magnetyczny pozostaje ultrasonografia przezodbytnicza. Dla właściwego zaplanowania rozległości operacji i ograniczenia ryzyka inkontynencji istotne jest określenie wysokości przetoki oraz tego, czy jest przednia, czy tylna. Inne istotne cechy anatomiczne, mające wpływ na wybór metody operacyjnej, obejmują liczbę i rodzaj rozgałęzień, umiejscowienie ujścia wewnętrznego i współistnienie zbiorników ropnych. EUS, jak każde badanie ultrasonograficzne, posiada swoje ograniczenia, a obrazowanie przetok nie jest pozbawione trudności. W artykule autorki przedstawiły problemy diagnostyczne związane z ultrasonografią transrektalną oraz wprowadzane na przestrzeni lat próby ulepszeniach metody. Podkreślenia wymaga znaczenie współpracy między ultrasonografistą a chirurgiem. Poza danymi odnoszącymi się do samej przetoki chirurg oczekuje informacji o ewentualnych uszkodzeniach zwieraczy i innych widocznych patologiach. Pomimo że EUS nie jest badaniem czynnościowym, opisanie zobrazowanego podczas badania skurczu dowolnego zwieracza zewnętrznego jest cenną wskazówką dla operatora. Dobrą praktyką jest uzupełnianie opisu EUS schematycznym rysunkiem, który szczególnie w przypadkach złożonych przetok ułatwia operatorowi wyobrażenie sobie przebiegu kanału. Chirurdzy natomiast powinni wymagać od siebie odpowiedzialnego i skrupulatnego wypełniania skierowania do pracowni EUS.
Summary
Conventional surgical treatment of anal fistula is associated not only with a high recurrence rate, but also with a complication that patients find very difficult to tolerate, namely deterioration of fecal and gas continence.
The anatomical course of the fistulous tract with regard to the sphincter muscles in combination with the results of function tests constitute the most important elements which decide about the selection of the surgical technique. In Poland, endoanal ultrasonography (EUS) is much more readily available than magnetic resonance imaging (MRI). In order to plan properly the extent of the surgical field, and limit the risk of incontinence, it is essential to determine the height of the fistula and whether it is anterior or posterior. The other significant anatomical features that have an impact on the choice of the surgical method include the number and the kind of branching, the location of the internal opening, and presence of purulent cisterns. Like every diagnostic procedure, endoanal ultrasonography (EUS) has its limitations, and imaging of fistulae is not free of difficulties. The article discusses the diagnostic problems related to endoanal ultrasonography, and the improvements of the method introduced over the years. Close cooperation between the ultrasonographer and the surgeon is essential. Besides details with regard to the fistula itself, the surgeon expects information if any damage of the sphincter muscles or any other visible pathologies are present. Despite the fact that EUS is not a function test, a contraction of the external sphincter muscle imaged during this procedure provides the surgeon with valuable information, hence relevant description should always be provided. Attaching the EUS description with a schematic drawing also helps the surgeon to understand the course of the fistulous tract better, especially in the case of especially complex fistulae. The surgeon, on the other hand, should provide the ultrasonographer with reliable, conscientiously filled in information when formally referring the patient to the EUS laboratory for the test.

Anal fistula is a long-known condition, with multiple surgical techniques developed to treat it. Even though not life-threatening, it remains a therapeutic and surgical challenge. Its conventional surgical management is not only associated with a high recurrence rate (0-26.5%), but also with another complication, especially unpleasant to the patients, namely deteriorated fecal and gas continence (9.7-40%) (1-5). Various surgical procedures have been developed over the recent years, utilizing fibrin glues (sealants), bioprosthetic plugs, devices such as a fistuloscope (video assisted anal fistula treatment – VAAFT) or laser, as well techniques allowing to avoid cutting the sphincter muscles (e.g. ligation of intersphincteric fistula tract – LIFT) to prevent postoperative incontinence. Apart from the availability of the abovementioned novelty therapies, the choice of the optimal surgical technique for any given patient naturally relies on the anatomical features of the fistula. The anatomical course of the fistulous tract in relation to the sphincter muscles combined with the results of function tests are major factors influencing the selection of the course of management.
To properly plan the extent of the operation, and limit the incontinence risk, it is essential to determine the height of the fistula and its location (posterior/interior). A high fistula is one where more than 1/3 of the external sphincter muscle’s length is involved. According to Tylicki’s classification, posterior fistulas are limited to 1/3 of the posterior circumference of the anus. This is a region ”protected” by the puborectal muscle, allowing the surgeon to extend sphincterotomy without risking postoperative incontinence in the patient. Anterior fistulas, however, involving the remaining periphery of the anus require more conservative and careful approach. For anterior, high fistulas, particularly in female patients, surgeons frequently apply conservative treatment methods, allowing to preserve the sphincters intact, such as excision of extrasphincteric fissure tract, excision and management of the internal opening with one of the methods available).
Other significant anatomic characteristics that have an impact on the choice of the surgical method include the number and the type of branching, the location of the internal opening, and presence of purulent cisterns. Not treated surgically, these elements will almost invariably lead to a recurring fistula.
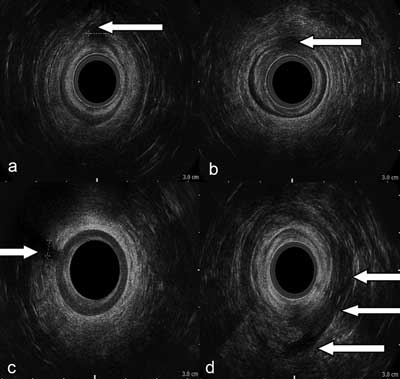
A thorough clinical exam by an experienced colorectal surgeon is extremely informative, yet deciding on a given course of operative management requires also the results of an imaging examination. In Poland, endoanal ultrasound (EUS) is much more readily available than magnetic resonance imaging (MRI), with numerous studies available to confirm its high diagnostic value. Since the late 1980s, EUS has found its application not only in the diagnostics of anal fistulae, but also for the diagnosis of damaged sphincter muscles, or rectal and anal cancer. As it facilitates accurate imaging of the anal anatomy (as opposed to fistulography or CT), EUS enables a detailed description of the fistula’s course and determining its height (fig. 1a-d).
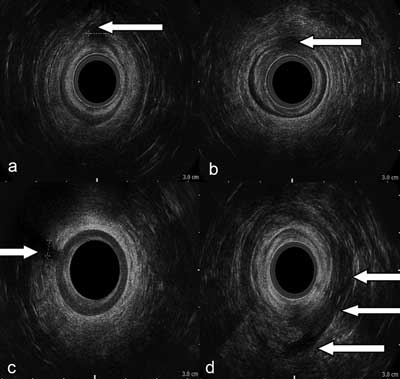
Fig. 1a-d. 2D EUS scans of anal fistulae: a) transphincteric, low, anterior, b) intersphincteric, low, anterior, c) transphincteric, low, anterior, d) horseshoe (sciatic-rectal), posterior
The high efficiency of EUS in the diagnostics of fistulae has been confirmed by numerous studies and publications (tab. 1).
Tab. 1. The efficiency of 2D EUS in evaluating selected features of anal fistulae (9-12)
| Evaluated element | Consistence with intraoperative evaluation |
| Primary tract | 36-100% |
| Branching present | 23-92% |
| Location of internal opening | 28-94% |
| Anal abscess | 55-100% |
Like every type of US examination, EUS has limitations, and imaging fistulae is not without its difficulties. The diagnostic problems, the improvements of the method introduced over the years and their significance for the diagnosis of anal fistulae are discussed henceforth.
EUS difficulties in the diagnostics of fistula tracts
Fistula tract is visible in EUS picture as a band-like structure of low echogenicity, sometimes even anechogenic. If gas is found in its lumen, the tract’s picture contains hyperechogenic elements. Postoperative scar has echogenicity similar to fistula, making it difficult to differentiate from a recurrent fistula, especially if its tract is narrow and does not contain any gas. A fistula misdiagnosed as a postoperative scar where clinical symptoms of fistula are scarce or nonexistent, adversely affects the decision to pursue operative treatment. A contrary misdiagnosis, where a postoperative scar is mistakenly identified as recurrence leads to unnecessary surgical intervention and puts the patient at a risk of iatrogenic fistula. When diagnosing first-time fistulas, it is possible to overlook suprasphincteric or extrasphincteric tracts, or suprasphincteric branching due to the limited imaging range (2-4 cm) characteristic for high frequency arrays used for EUS. Determining accurately the fistula’s type may also pose problems. It is challenging to differentiate low transphincteric tracts from intersphincteric ones due to the presence of hyperechogenic artifacts in EUS image, owing to the presence of air in the space between the probe and the distal portion of the anal canal. The artifacts make it difficult or impossible to accurately evaluate the further portion of the external sphincter, potentially leading to a misdiagnosis. Differential diagnosis between high transphincteric tracts and suprasphincteric ones is challenging due to the oblique course of the fibers of the pubic rectal muscle and the difficulties in evaluating the location of the fistula in relation to the muscle.
In most cases, neither of the above mistakes affects the choice of the surgical therapy, hence their limited clinical significance. Typically, the surgeon decides to pursue fistulotomy or fistulectomy to treat low fistulas, whereas in patients with a high transphincteric or suprasphincteric fistula a sphincter-preserving or staged procedure is more common.
Powyżej zamieściliśmy fragment artykułu, do którego możesz uzyskać pełny dostęp.
Mam kod dostępu
- Aby uzyskać płatny dostęp do pełnej treści powyższego artykułu albo wszystkich artykułów (w zależności od wybranej opcji), należy wprowadzić kod.
- Wprowadzając kod, akceptują Państwo treść Regulaminu oraz potwierdzają zapoznanie się z nim.
- Aby kupić kod proszę skorzystać z jednej z poniższych opcji.
Opcja #1
29 zł
Wybieram
- dostęp do tego artykułu
- dostęp na 7 dni
uzyskany kod musi być wprowadzony na stronie artykułu, do którego został wykupiony
Opcja #2
69 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 30 dni
- najpopularniejsza opcja
Opcja #3
129 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 90 dni
- oszczędzasz 78 zł
Piśmiennictwo
1. Nwaejike N, Gilliland R: Surgery for fistula in ano: an audit of practice of colorectal and general surgeons. Colorectal Dis 2007; 9(8): 749-753. 2. Lunnis DJ, Kamm MA, Phillips RKS: Factors affecting continence after surgery for anal fistula. Br J Surg 1994; 81: 1382-1385. 3. Garcia-Aquilar J, Davey CS, Le CT et al.: Patient satisfaction after surgical treatment for fistula in ano. Dis Colon Rectum 2000; 43(9): 1206-1212. 4. Rosa G, Lolli P, Piccinelli D et al.: Fistula in ano: anatomoclinical aspects, surgical therapy and results in 844 patients. Tech Coloproctol 2006; 10(3): 213-215. 5. Wadare IJ: Sphincter-preserving techniques for anal fistulas in Japan. Dis Colon Rectum 2000; 4(10): 69-77. 6. Law PJ, Talbot RW, Bartram CI, Northover JM: Anal endosonography in the evaluation of perianal sepsis and fistula in ano. Br J Surg 1989; 76(7): 752-755. 7. Choen S, Burnett S, Bartram CI, Nicholls RJ: Comparison between anal endosonography and digital examination in the evaluation of anal fistulae. Br J Surg 1991; 78(4): 445-447. 8. Toyonaga T, Tanaka Y, Song JF et al.: Comparison of accuracy of physical examination and endoanal ultrasonography for preoperative assessment in patients with acute and chronic anal fistula. Tech Coloproctol 2008; 12(3): 217-223. 9. Deen KI, Williams JG, Hutchinson R et al.: Fistulas in ano: endoanal ultrasonographic assessment assists decision making for surgery. Gut 1994; 35(3): 391-394. 10. Cataldo PA, Senagore A, Luchtefeld MA: Intrarectal ultrasound in the evaluation of perirectal abscesses. Dis Colon Rectum1993 Jun; 36(6): 554-558. 11. Hussain SM, Stoker J, Schouten WR et al.: Fistula in ano: endoanal sonography versus endoanal MR imaging in classification. Radiology 1996; 200(2): 475-481. 12. Navarro-Luna A, García-Domingo MI, Rius-Macías J, Marco-Molina C: Ultrasound study of anal fistulas with hydrogen peroxide enhancement. Dis Colon Rectum 2004; 47(1): 108-114. 13. Sudoł-Szopińska I, Szczepkowski M, Panorska AK et al.: Comparison of contrast-enhanced with non-contrast endosonography in the diagnostics of anal fistulas. Eur Radiol 2004; 14(12): 2236-2241. 14. Bernstein MA, Nogueras JJ, Weiss EG, Wexner SD: The use of endoanal ultrasonography in identifying fistula-in-ano. Coloproctol 1997; 19(2): 72-76. 15. Ratto C, Gentile E, Merico M et al.: How can the assessment of fistula-in ano be improved? Dis Colon Rectum 2000; 43(10): 1375-1382. 16. Nagendranath C, Saravanan MN, Sridhar C, Varughese M: Peroxide-enhanced endoanal ultrasound in preoperative assessment of complex fistula-in-ano. Tech Coloproctol 2014; 18(5): 433-438. 17. Obcowska A, Kołodziejczak M, Sudoł-Szopińska I: Przydatność przedoperacyjnego badania endosonograficznego w różnicowaniu przetok odbytu niskich z wysokimi. Post Nauk Med 2013; 8: 543-547. 18. Ratto C, Grillo E, Parello A et al.: Endoanal ultrasound-guided surgery for anal fistula. Endoscopy 2005; 37(8): 722-728. 19. Buchanan GN, Bartram CI, Williams AB et al.: Value of hydrogen peroxide enhancement of three-dimensional endoanal ultrasound in fistula-in-ano. Dis Colon Rectum 2005; 48(1): 141-147. 20. Kim Y, Park YJ: Three-dimensional endoanal ultrasonographic assessment of an anal fistula with and without H2O2 enhancement. World J Gastroenterol 2009; 15(38): 4810-4815. 21. West RL, Dwarkasing S, Felt-Bersma RJ et al.: Hydrogen peroxide enhanced three-dimensional endoanal ultrasonography and endoanal magnetic resonance imaging in evaluating perianal fistulas: agreement and patient preference. Eur J Gastroenterol Hepatol 2004; 16: 1319-1324. 22. West RL, Zimmerman DD, Dwarkasing S et al.: Prospective comparison of hydrogen peroxide-enhanced three-dimensional endoanal ultrasonography and endoanal magnetic resonance imaging of perianal fistulas. Dis Colon Rectum 2003; 46: 1407-1415. 23. Cho DY: Endosonographic criteria for an internal opening of fistula-in-ano. Dis Colon Rectum 1999; 42(4): 515-518. 24. Santoro GA, Ratto C, Di Falco G: Three-dimensional reconstructions improve the accuracy of endoanal ultrasonography in the identification of internal openings of anal fistulas. Poster European Association of Coloproctology 5th Scientific and Annual Meeting September16?18, 2004, Geneva, Switzerland. 25. Sudoł-Szopińska I, Kołodziejczak M, Szopiński TR: The accuracy of a postprocessing technique volume render mode in three dimensional endoanal ultrasonography of anal abscesses and fistulas. Dis Colon Rectum 2011 Feb; 54(2): 238-244. 26. Stewart LK, McGee J, Wilson SR: Transperineal and transvaginal sonography of perianal inflammatory disease Am J Roentgenol 2001; 177: 627-632. 27. Kołodziejczak M, Stefański R, Sudoł-Szopińska I, Jakubowski W: Transrectal and transperineal sonography in the diagnosis of hydradenitis suppurativa. Radiol Oncol 2003; 37(3): 161-165.