*Lidia Zawadzka-Głos, Monika Jabłońska-Jesionowska
Assessment of efficacy of laryngotracheal reconstruction with autogenous rib cartilage graft
Ocena skuteczności zabiegów rekonstrukcyjnych krtani z użyciem wszczepu chrzęstnego
Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Associate Professor Lidia Zawadzka-Głos, MD, PhD
Streszczenie
Wstęp. Zwężenia podgłośniowe krtani są przyczyną niewydolności oddechowej, w szczególności u noworodków i małych dzieci. Są najczęstszym wskazaniem do wykonywania tracheostomii w celu utrzymania drożności dróg oddechowych w tej grupie wiekowej. Zwężenia te wymagają leczenia chirurgicznego. Jedną z wielu metod leczenia jest zabieg rekonstrukcji krtani z użyciem wszczepu chrzęstnego z żebra.
Cel pracy. Celem pracy była ocena skuteczności zabiegów rekonstrukcji krtani z użyciem wszczepu z żebra.
Materiał i metody. Poddano analizie przebieg leczenia operacyjnego 8 dzieci ze zwężeniem okolicy podgłośniowej krtani. Stopień zwężenia w badaniu endoskopowym oceniono, stosując skalę Myera?Cottona. Miarą skuteczności leczenia była możliwość wykonania skutecznej dekaniulacji pacjenta.
Wyniki. Wśród 8 pacjentów było 6 chłopców i 2 dziewczynki. Wszystkie dzieci były urodzone przedwcześnie pomiędzy 24. a 34. tygodniem ciąży i zostały zaintubowane we wczesnym okresie noworodkowym. W 5 przypadkach dokonano dekaniulacji, w 3 przypadkach leczenie nie było wystarczająco skuteczne, a u dzieci występowały dodatkowe problemy pediatryczne.
Wnioski. Do pointubacyjnych zwężeń okolicy podgłośniowej predysponowane są wcześniaki zaintubowane we wczesnym okresie noworodkowym. Leczenie chirurgiczne z użyciem wszczepu chrzęstnego z żebra jest skuteczną metodą leczenia. Wyniki leczenia są powiązane również ze stanem pediatrycznym pacjenta oraz ze współistniejącymi zmianami w obrębie krtani.
Summary
Introduction. Subglottic stenosis may lead to respiratory failure, especially in newborns and small children. It is the most common indication for tracheostomy in order to maintain airway patency in this age group. Subglottic stenosis requires surgical treatment. Laryngotracheal reconstruction with autogenous rib cartilage graft is one of the many treatment methods.
Aim. The aim of the study was to assess of efficacy of laryngotracheal reconstruction with autogenous rib cartilage graft.
Material and methods. Clinical data of 8 children operated for subglottic stenosis has been analysed. The severity of stenosis was assessed during the endoscopic examination with the Myer?Cotton Grading System. The efficacy of treatment was understood as a possibility of decannulation.
Results. The study group included 8 patients: 6 boys and 2 girls. All the children had been born prematurely between the 24th and 34th week of pregnancy and were intubated in the early neonatal period. In 5 cases, decannulation followed, and in 3 cases, the treatment proved to be not effective enough, as the children had additional health problems.
Conclusions. Prematurely born children intubated in the early neonatal period are at risk of post-intubation subglottic stenosis. Laryngotracheal reconstruction with autogenous rib cartilage graft is an effective treatment method. Treatment outcomes are also dependent on the overall health status of the patient and coexisting tracheal lesions.
Introduction
Airway stenosis in children is a serious health problem that frequently requires surgical intervention. Physiologically, subglottis remains the narrowest part of the larynx. It consists of a full cartilage ring called cricoid cartilage. It is this part of larynx that is most frequently associated with respiratory problems in children. Subglottis is easily affected by inflammatory or allergic edema, and it is also predisposed to post-intubation stenosis, as well as congenital defects (e.g. congenital cricoid stenosis). Sometimes differentiating congenital defects and post-intubation lesions may be difficult, especially in cases when the defect was diagnosed in a premature infant who was intubated directly after birth in order to maintain airway patency. Regardless of etiology, subglottic stenosis requires surgical treatment. The treatment method depends on the grade of stenosis and post-intubation lesions having an early or late character. In severe stenoses, tracheostomy is performed in order to maintain airway patency. There are many methods of surgical treatment, from endoscopic management to cricotracheal resection. Laryngotracheal reconstruction with autogenous rib cartilage graft is one of the many treatment methods (fig. 1).
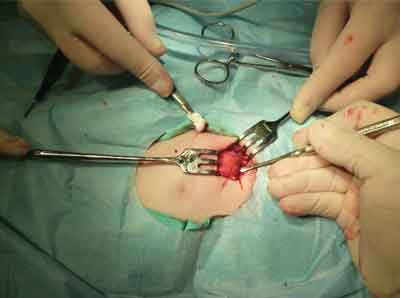
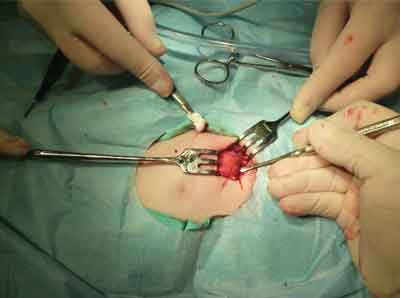
Fig. 1. Harvesting rib cartilage
Aim
The aim of the study was to assess the efficacy of laryngotracheal reconstruction with autogenous rib cartilage graft.
Material and methods
For the study, we selected patients of the Department of Pediatric Otolaryngology of the Medical University of Warsaw who had undergone laryngotracheal reconstruction with autogenous rib cartilage graft. Grade of stenosis, gestational age at delivery, and the result of endoscopic examination before and after the treatment have been analyzed. All the patients had undergone tracheostomy before the stenosis treatment in order to maintain airway patency. The treatment outcome was considered positive when the patient could be successfully decannulated or when their airways were sufficiently wide.
The severity of stenosis before and after the treatment was assessed with the Myer?Cotton Grading System. According to the adopted System, grade I stenosis is an obstruction that is less than 50%, grade II ? obstruction between 51% and 70%, grade III ? obstruction between 71% and 99% (fig. 2), and grade IV ? obstruction between 99% and 100%.

Fig. 2. Grade III subglottic stenosis according to Myer?Cotton Grading System
In our patients, laryngotracheal reconstruction with autogenous rib cartilage graft was performed. The cartilage was harvested from the 6th rib, and the harvested graft was processed and implemented in the subglottic region, enabling to expand its diameter (fig. 3).

Fig. 3. Rib cartilage graft introduced into the subglottic region
Results
Medical data of 8 patients, including 2 girls and 6 boys treated for post-intubation subglottic stenosis, were analyzed. The follow-up was 5 years. All the children had been born prematurely between the 24th and 34th week of pregnancy and were intubated in the early neonatal period. In 4 boys and 1 girl, grade III obstruction according to Myer?Cotton Grading System was diagnosed, and in 2 boys and 1 girl, grade IV obstruction was diagnosed. All the children were qualified for laryngotracheal reconstruction with autogenous rib cartilage graft. Endoscopic examination performed after the surgery revealed widened subglottic region in all the patients, however, the diameter had not returned to its physiological dimensions in any of the cases. In 5 patients, the outcomes enabled decannulation, and in 3 patients, tracheostomy was kept. In 1 decannulated child, retracheostomy was performed due to lower respiratory tract failure due to infection. After the surgery, grade I stenosis was observed in 5 patients, and grade II stenosis ? in 3 patients. In 5 children, the graft displaced in the direction of the airways, which required reoperation. In 1 child, adhesion between the anterior and posterior tracheal wall occurred. Three children could not be decannulated. Two of them had initially suffered from the grade IV obstruction, and all 3 had coexisting lesions of vocal cords and epiglottic region. In all 3, graft displacement occurred. All 3 children suffered from comorbidities, such as bronchopulmonary dysplasia and status post brain hemorrhage.
Discussion
Subglottic stenosis in children is a serious diagnostic and therapeutic problem. It is the most common indication for tracheostomy in children. The treatment is difficult and often multi-stage, and the effect is not always satisfactory. What causes the most problems is the diameter of the airways, which is 5-8 mm in the subglottic region in a healthy newborn, while the dimensions are adequately smaller in premature infants. Preterm delivery and its consequences are a serious problem in modern perinatology. In Poland, the incidence of preterm births is 4.5-12% of live births, depending on the country region (1). Premature birth is the main cause for perinatal mortality (2, 3). The greatest threat to life and development of a newborn is the overall underdevelopment of all the systems, in particular of the respiratory system (2, 3). In case of respiratory failure, prolonged intubation is applied, which may lead to subglottic stenosis. The results of our study support these conclusions ? all the patients included in our analysis were born prematurely and were intubated. The risk of post-intubation stenosis in children is estimated at 0.1-2% (4). Solvitzky et al. (5) hypothesized that in preterm infants, it is the autoimmune mechanisms associated with type II collagen that are responsible for subglottic stenosis after intubation injury. In the study, antibodies against type II collagen were detected in infants with post-intubation laryngeal stenosis, while the antibodies were not detected in children without post-intubation complications (5). Other concept regarding the predisposition for post-intubation laryngeal stenosis was presented by Lima et al. (6). Based on the performed morphometric studies, they have proven that the shape of subglottic region in preterm infants is, in fact, elliptical, thus significantly differing from the shape of an endotracheal tube, which may lead to the formation of pressure ulcers and secondary laryngeal obstruction. Monnier (7) have also drawn attention to the shape of the subglottic region, which contributed to the development of profiled separators.
Rib cartilage graft is an open surgical method that have been recognized for many years in the treatment of severe laryngeal stenosis. However, secondary stenosis after reconstructive surgery is often observed, which prevents decannulation and requires reoperation or endoscopic treatment (8-12). The basis for qualification for reconstructive surgery of the described patients was sever post-intubation laryngeal stenosis and no improvement after endoscopic treatment. The authors applied endoscopic treatment in 91 patients in total. Five of the 8 children who had undergone reconstructive surgery with rib cartilage graft were decannulated. Bakthavachalam (13) noted that in the group of 102 patients treated with open surgical techniques, as many as 56 patients required additional procedures due to restenosis.
Important complications observed by many authors in children who had undergone laryngotracheal reconstruction with autogenous rib cartilage graft include graft displacement and adhesions. In our material, 4 patients required reoperation due to graft displacement. Lesions of vocal cords and epiglottic region consist an additional obstacle in obtaining sufficiently wide airways and successful decannulation. Additional factors influencing the possibility of decannulation include coexisting respiratory disorders, such as bronchopulmonary dysplasia and lower respiratory tract dysfunction. In 3 patients who could not be decannulated, lower respiratory tract dysfunction and vocal cord lesions were observed in addition to laryngeal obstruction.
Conclusions
Prematurity consists a serious risk factor for the occurrence of post-intubation laryngeal stenosis in children. Laryngotracheal reconstruction with autogenous rib cartilage graft is an effective treatment method. In the course of treatment, complications, such as graft displacement or adhesions, may occur. The possibility of decannulation is affected by many factors, including airway diameter and general health condition of the patient. The patients with coexisting lower respiratory tract dysfunction and epiglottic lesions have poorer prognosis.
Piśmiennictwo
1. Pietrzak B, Kawka J: Zakażenia a poród przedwczesny. Nowa Med 1999; 6: 19-20.
2. Urban J, Lemancewicz A: Nowe spojrzenie na patomechanizm porodu przedwczesnego. Nowa Med 1999; 6: 24-27.
3. Karwan-Płońska A: Kliniczna analiza porodów przedwczesnych. Nowa Med 1999; 6: 21-23.
4. Walner DL, Loewen MS, Kimura RE: Neonatal subglottic stenosis ? incidence and trends. Laryngoscope 2001; 111(1): 48-51.
5. Stolovitzky JP, Todd NW: Autoimmune hypothesis of acquired subglottic stenosis in premature infants. Laryngoscope 1990; 100(3): 227-230.
6. Lima LF, Nita LM, Campelo VE et al: Morphometric study on the anatomy of fetal cricoid cartilage and comparison between its inner diameter and endotracheal tube sizes. Ann Otol Rhinol Laryngol 2008; 117(10): 774-780.
7. Monnier P: Airway stenting with the LT-Mold: Experience in 30 pediatric cases. Int Journal of Ped Otorhinolaryngol 2007; 71: 1351-1359.
8. Berkowitz RG: Failed paediatric laryngotracheoplasty. ANZ J Surg 2001; 71(5): 292-296.
9. Hartnick CJ, Hartley BE, Lacy PD et al: Surgery for pediatric subglottic stenosis: disease-specific outcomes. Ann Otol Rhinol Laryngol 2001; 110(12): 1109-1113.
10. Matute JA, Villafruela MA, Hernandez JM et al: Analysis of treatment failure in pediatric subglottic stenosis. Ann Esp Pediatr 2000; 52(3): 242-244.
11. Monnier P, Lang F, Savary M: Partial cricotracheal resection for pediatric subglottic stenosis: a single institution’s experience in 60 cases. Eur Arch Otorhinolaryngol 2003; 260(6): 295-297.
12. Younis RT, Lazar RH, Bustillo A: Revision single-stage laryngotracheal reconstruction in children. Ann Otol Rhinol Laryngol 2004; 113(5): 367-372.
13. Bakthavachlam S, McClay JE: Endoscopic management of subglottic stenosis. Otolaryngol Head Neck Surg 2008; 139(4): 551-559.