Małgorzata Badełek-Izdebska, *Lidia Zawadzka-Głos
Mediastinal emphysema as a complication of posterior pharyngeal wall injury – a case report
Odma śródpiersiowa jako powikłanie urazu tylnej ściany gardła – opis przypadku
Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Associate Professor Lidia Zawadzka-Głos, MD, PhD
Streszczenie
Odma śródpiersiowa to stan patologiczny, w którym powietrze obecne jest w śródpiersiu. Odma śródpiersiowa może powstać samoistnie lub być efektem zaistnienia zmian chorobowych albo urazów, w tym również urazów jatrogennych. Powietrze do śródpiersia może przejść z płuc, tchawicy, oskrzeli, przełyku, jamy otrzewnej lub pochodzić z zewnątrz ciała pacjenta. Może też przedostawać się ze śródpiersia do szyi lub jamy brzusznej. Śródpiersie komunikuje się z przestrzenią podżuchwową, przestrzenią zagardłową oraz osłonkami naczyniowymi w obrębie szyi. Czynniki sprzyjające wystąpieniu odmy śródpiersia to: próba Valsalvy, wysiłek fizyczny, wzmożony wysiłek oddechowy, kaszel, astma, infekcje dróg oddechowych, wymioty, zażywanie narkotyków. Pacjent z odmą śródpiersia może nie prezentować żadnych dolegliwości lub też mogą wystąpić objawy niewydolności oddechowej. Najczęstszymi obserwowanymi objawami są: ból zamostkowy promieniujący do barku lub pleców oraz narastający przy zmianie pozycji ciała, duszność, kaszel, ból lub dyskomfort w obrębie szyi, zaburzenia połykania, tachykardia, a także odma podskórna. Rozpoznanie stawiamy na podstawie obrazu klinicznego uwzględniającego przyczynę wywołującą oraz badań radiologicznych. Przedstawiono przypadek pacjenta, u którego odma śródpiersiowa wystąpiła w efekcie urazu tylnej ściany gardła.
Summary
Mediastinal emphysema is a pathological condition in which air is present in the mediastinum. Mediastinal emphysema may occur spontaneously or as a result of disease or trauma, including iatrogenic injury. Air into the mediastinum may pass from the lungs, trachea, bronchi, esophagus, peritoneal cavity, or come from outside the patient's body. It can also pass from the mediastinum into the neck or abdominal cavity. The mediastinum communicates with the submandibular space, the retropharyngeal space, and the vascular sheaths in the neck. Predisposing factors for mediastinal emphysema include the Valsalva test, physical exertion, increased respiratory effort, coughing, asthma, respiratory infections, vomiting, and drug use. A patient with mediastinal emphysema may present with no symptoms or may present with symptoms of respiratory distress. The most common symptoms observed are retrosternal pain radiating to the shoulder or back and increasing with changes in body position, dyspnea, cough, neck pain or discomfort, dysphagia, tachycardia, and subcutaneous emphysema. The diagnosis is made on the basis of clinical features including the underlying cause and radiological findings. A case of a patient with mediastinal emphysema due to trauma to the posterior pharyngeal wall is presented.
Introduction
Air emphysema is a pathological condition in which air is forced into soft tissues where it is not physiologically present. Mediastinal emphysema (pneumomediastinum) is the presence of free air within the connective tissue of the mediastinum. It is often accompanied by subcutaneous emphysema, characterised by palpable crepitations within the skin. In the case of mediastinal emphysema as a result of trauma to the posterior pharyngeal wall, the air in the retropharyngeal space passes into the parapharyngeal space and from there along the least resistance route along the neck fascia into the mediastinum. From there, it can pass further into the pleural cavity or even the pericardial cavity, thus posing an immediate threat to life. Mediastinal emphysema usually occurs in young patients with loose and flaccid mediastinal tissues compared to older patients with fibrotic tissues in this space, impeding air migration (1). The patient’s symptoms, general condition and possible complications may correlate with the extent of emphysema and the prevailing mediastinal pressure. The following is a case of a patient admitted to the Department of Pediatric Otolaryngology with mediastinal emphysema due to throat trauma
Case report
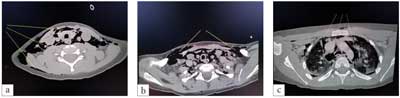
A 5-year-old boy with trisomy 21 was admitted to the Department of Pediatric Otolaryngology, Medical University of Warsaw, from a children’s hospital of a lower referral level because of posttraumatic mediastinal emphysema and subcutaneous emphysema of the neck and supraclavicular region found on CT examination. On the day of admission to the first hospital, the boy sustained injury to the posterior pharyngeal wall with a toothbrush held in the mouth during a fall. The injury caused throat bleeding, and the boy reported throat pain and difficulty swallowing saliva. Fiberoptic examination on admission did not show damage to the pharyngeal mucosa or active bleeding, only a protrusion/swelling of the posterior pharyngeal wall was visible. A CT scan of the neck and chest performed described: “Examination with administration of 15 ml contrast medium. Presence of increased subcutaneous emphysema of the neck and upper chest. Presence of air in pharyngeal space, perivascular space, upper mediastinum and vestigially subpleural. At the level of the lower pharynx, on the right side, a small tissue element of 5 mm in the pharyngeal space is visible, which may correspond to a fragment of pharyngeal tissue entered into the pharyngeal space. The larynx is undamaged, pear-shaped lobules and epiglottis are unchanged. The cervical venous and arterial vessels were properly patched, without lesions” (Fig. 1a-c). No pathological fluid reservoirs or haematomas or shadowing foreign bodies were found within the neck organs. The bony elements within the scope of the examination were not damaged.
Fig. 1a-c. CT scans of the neck and chest showing air in the mediastinum and soft tissues of the neck (arrows)
On the next day of hospitalization, due to the severity of emphysema and the possibility of its further development as well as the risk of nasopharyngeal flora infection, the patient was transferred by medical transport to the Children Clinical Hospital of the Medical University of Warsaw.
Until the nasopharyngeal swab for COVID-19 collected during the stay in the previous hospital was negative (test result – negative), the patient was isolated in the patient room and all nursing activities and medical examination were performed in personal protective equipment.
On admission to the Pediatric Otolaryngology Department of the Medical University of Warsaw, the boy was in good general condition, with efficient respiratory and circulatory systems. No respiratory disturbances in the form of stridor or dyspnoea were found. The boy’s voice was sonorous. No significant abnormalities were found in vital signs: saturation 96%, pulse 103/minute, blood pressure 110/79 mmHg, body temperature 36.9 degrees Celsius. The boy reported complaints of throat and neck pain.
On physical examination, swelling of the soft tissues in the anterior part of the neck and in the supraclavicular region was found; palpation showed marked crepitations in the swollen areas. Neck mobility was preserved in all directions. Auscultation was normal with alveolar respiratory murmur, numerous crackles were heard in the upper part of the chest from the front, and normal murmur from the back.
ENT examination of the posterior wall of the middle pharynx, in its lower part on the right side, revealed a small wound without the presence of active bleeding; the wound area with mucosal oedema was present. No other post-traumatic lesions were found within the oral cavity, palatal arches, palatine uvula and tonsils. There were also no features of upper respiratory tract infection. Due to the lack of laryngeal symptoms and examination performed the day before, repeat fibroscopy was not performed. The laboratory blood tests showed elevated CRP and slight leucocytosis; gasometry was normal. Due to short time since injury, the patient was fasted and started i.v. hydration. Constant monitoring of vital signs (saturation, HR, RR) and restriction of exercise were ordered. The treatment included analgesics and broad-spectrum intravenous antibiotic therapy (second-generation cephalosporin and clindamycin). On the 1st day of treatment, an i.v. corticosteroid was also continued.
On the next day of observation, the patient reported slight throat and neck pain, no fever, no respiratory disturbances or cough, saturation maintained at 96-97%, heart rate 92-117/min. Crepitations of the neck region were still palpable. Oral rehydration was started, followed by feeding with pureed diet, which the boy accepted reluctantly due to sore throat. In the following days, the patient’s vital signs were monitored, which remained within normal limits, and the decrease of neck tissue oedema was observed. The boy reported no more pain, his appetite improved, no respiratory disturbances were observed. On post-injury day 4, the chest X-ray was performed, which revealed slight mediastinal emphysema and air in the soft tissues of the neck and in the scapular projection (Fig. 2). Otherwise, the chest and neck organs were normal. There were no abnormalities on ECG.

Fig. 2. Fourth day after injury
On the 8th day after physical examination, discrete subcutaneous crackles were still felt in the neck tissues, the supraclavicular region was free from crepitation. A control chest X-ray was performed and described the presence of air in the neck tissues, otherwise the organ picture was normal (Fig. 3). Patient’s saturation was 98%, HR 110/min, respiratory rate 25/min, auscultatory breath sounds were normal bilaterally. The patient was consulted in pulmonology. In the absence of complaints, normal vital signs and significant improvement in imaging studies, the patient was discharged home.

Fig. 3. Eighth day after injury
Discussion
The presence of air in the mediastinum – mediastinal emphysema (pneumomediastinum) – is a rare condition first described by Simmons in 1783 following the Valsalva manoeuvre. The first description of mediastinal emphysema resulting from trauma was given by Laennec in 1819. The clinical manifestations of mediastinal emphysema were described in 1939 by Hamman. Hamman, and one of the characteristic auscultatory signs was named after him.
Air may be introduced into the mediastinal tissues as a result of lesions or trauma (secondary pneumomediastinum), or it may move spontaneously without an identifiable cause (primary pneumomediastinum), most commonly as a result of the application of appropriate pressure under favourable conditions such as the Valsalva test, coughing, defecation, labour or exercise.
In spontaneous pneumothorax air from alveoli bursting due to a sudden increase in airway pressure passes along the peribronchial and perivascular spaces to the mediastinum and from there through the interlobular route to the neck tissues. This situation occurs most frequently in patients with asthma, COPD and emphysema. Also, patients on positive pressure replacement ventilation or ventilated with high tidal volumes are at higher risk of developing this complication due to barotrauma. Over the past 12 months, as of February 2020, there have been an increasing number of reports of patients with pneumomediastinum ventilated due to respiratory failure in COVID-19 (2), and patients infected with COVID-19 without prior mechanical ventilation (3).
Intense cough associated with respiratory tract infection may also be a cause of mediastinal emphysema (4).
The most common traumatic cause of mediastinal emphysema is head injury (5) and neck (6).
Dental procedures such as tooth extraction, endodontic treatment, implant treatment, or apicectomy are relatively common causes of pneumothorax (7, 8).
Traumatic mediastinal emphysema can occur when there is a sudden crushing of the chest with an increase in pressure inside the chest, as well as during extensive trauma with rib or sternum fractures causing damage to the pulmonary parenchyma (4). The air then travels from the mediastinum to the subcutaneous spaces of the neck and may cause subcutaneous emphysema of the neck and face.
Mediastinal emphysema may accompany lung abscess, foreign body in the airway (9) or esophagus.
Air has also been reported to enter the mediastinum as a result of abdominal trauma (e.g. gastric injury) or surgical procedures within the abdomen, e.g. during laparoscopy or renal biopsy (airway to the thorax through the aortic foramen and periaphragmatic diaphragm).
Iatrogenic traumatic causes may include surgery of the thyroid gland, tonsils (10), nose (11), traumatic intubation, mediastinoscopy or sternal marrow trepanobiopsy. Mediastinal emphysema may also occur as a result of intense vomiting (12).
Rare causes of mediastinal emphysema include caeson disease, seizures, and metabolic acidosis in diabetes. Cases of mediastinal emphysema in patients with anorexia nervosa have also been reported in the literature (13).
Cases of patients taking psychostimulants and narcotics are also known and described in literature (14).
The most common clinical manifestations of mediastinal emphysema are, according to frequency: chest pain (retrosternal) and neck pain, dyspnoea, subcutaneous emphysema, cough and dysphagia (15-17).
Hamman’s sign or mediastinal crunch on auscultation of the patient is heard in the cardiac output, and the crunching or creaking sounds appear in a cyclic manner, consistent with the rhythm of the heart and (partly) with the phases of breathing. Usually the inspiratory phase is more accentuated and in the left side position. However, according to reports in the literature, this symptom occurs in only 11.6-30% of patients (18, 19).
Other symptoms that may occur in a proportion of patients include dysphonia, tachycardia, tachypnoe or just restlessness.
Mediastinal emphysema may be accompanied by pneumothorax, usually of minor severity.
A condition in which the accumulation of a significant amount of air in the mediastinum by its compression causes obstruction of the great vessels or trachea is considered life-threatening, and pneumothorax may cause symptoms of reduced venous return and cardiac tamponade. The patient may be febrile, which often indicates the potential for infection to enter the mediastinum. Mediastinal inflammation still has a high mortality rate.
Laboratory tests may show elevated inflammatory parameters and abnormalities in gasometry (20).
Our patient reported complaints of sore throat and swallowing discomfort resulting in decreased appetite and neck pain associated with tissue swelling due to air spaces.
Radiological diagnosis is crucial in the diagnosis. Chest X-ray in PA projection is not always sufficient to make the diagnosis with certainty – linear air shadows surrounding the narrow outline of the left ventricle and aortic arch and slit-like air reservoirs in the clavicular and neck regions may be poorly visible (16). On lateral radiographs, mediastinal air may be slightly more visible, but even this does not always confirm the diagnosis. Therefore, the definitive test is a chest CT scan, which has a sensitivity according to the literature of 100% and a specificity of 85% (21, 22). Tomography allows not only to assess the extent of mediastinal emphysema, but also to identify causative factors or coexisting other pathologies.
For mediastinal emphysema of traumatic aetiology, diagnostic bronchoscopy may be necessary if airway injury is suspected or esophagoscopy if esophageal injury is suspected. In cases of pharyngeal trauma, fibroscopy evaluating tissues from the nasopharynx down to the level of the vocal folds may be sufficient. In very urgent cases, mediastinal ultrasonography is used in the identification of pneumomediastinum (23, 24).
Once serious concomitant life-threatening pathology has been recognised and excluded, management is largely focused on symptomatic treatment. It is the treatment of spontaneous mediastinal emphysema that is most often conservative. The site of air leakage into the tissues is expected to heal and the air in the mediastinal and neck tissues is gradually absorbed spontaneously. Monitoring of vital signs allows continuous control of the patient’s condition. Appropriate management consists of limiting physical activity until air is absorbed, analgesics and antibiotic therapy (mediastinitis prophylaxis) (19). Oxygen therapy may also be used if necessary, but despite reports of rapid resolution of mediastinal emphysema with 100% oxygen, the efficacy of oxygen therapy is still inconclusive (16, 25).
In cases of mediastinal emphysema of post-traumatic aetiology, management also depends on clinical signs, patient condition and the severity of the emphysema (26). In traumatic emphysema, severe dyspnoea, hypotonia or even shock, mediastinal displacement is more common. If the symptoms of emphysema increase and, as a result, respiratory failure intensifies, then decompression of emphysema by puncturing the appropriate space or surgical closure of the air leakage site is considered (11). Obviously, during this period the patient requires control of saturation, pulse and blood pressure as well as restriction of physical activity. We use analgesics and antimicrobial drugs (27).
The prognosis of mediastinal pneumothorax depends on its etiology. The prognosis in spontaneous mediastinal empyema is usually good due to its ability to self-limit. However, complete absorption of air in the tissues takes some time.
Although the duration of hospitalisation is determined by the patient’s general condition, it is considered that hospitalisation until complete resolution of symptoms or confirmation of full recovery is not necessary.
In the case of our patient, the suspicion of mediastinal emphysema was raised on the basis of physical examination and clinical symptoms associated with the presence of air in the neck tissues. The diagnosis was made on computed tomography of the neck and chest, no previous chest x-ray was performed. Prophylactic antibiotic therapy was administered because of the risk of spread of nasopharyngeal bacterial flora through damaged tissues of the posterior pharyngeal wall to the mediastinal space. These bacteria could be a potential cause of mediastinitis and/or sepsis.
Conclusions
Suspicion of post-traumatic mediastinal emphysema may be raised by the presence of air (crepitations) in the neck tissues and reports of neck and chest pain.
On physical examination, the characteristic Hamman sign is not always heard.
A chest X-ray confirmed by a CT scan of the head, neck and chest is the decisive examination for diagnosis.
The appropriate management of post-traumatic emphysema is to assess the extent of the injury and its possible provision. If surgery is not necessary, the patient requires close observation with monitoring of vital signs, broad-spectrum antibiotic therapy, analgesics and glucocorticosteroids.
In the vast majority of cases, mediastinal emphysema resolves within about 7-10 days, sometimes air in the tissues may still be visible beyond this period (27).
Piśmiennictwo
1. Kobashi Y, Okimoto N, Matsushima T et al.: Comparative study of mediastinal emphysema as determined by etiology. Intern Med 2002; 41: 277-282.
2. Elhakim TS, Abdul HS, Pelaez Romero C, Rodriguez-Fuentes Y: Spontaneous pneumomediastinum, pneumothorax and subcutaneous emphysema in COVID-19 pneumonia: a rare case and literature review. BMJ Case Rep 2020; 13(12): 239489.
3. Quincho-Lopez A, Quincho-Lopez DL, Hurtado-Medina FD: Case Report: Pneumothorax and Pneumomediastinum as Uncommon Complications of COVID-19 Pneumonia-Literature Review. Am J Trop Med Hyg 2020; 103(3): 1170-1176.
4. Bartela E, Mikołajczak M, Prech M: Pneumomediastinum as a rare cause of retrosternal chest pain – report of two cases. Pol Merk Lek 2011; XXXI(186): 360.
5. López-Peláez MF, Roldán J, Mateo S: Cervical emphysema, pneumomediastinum, and pneumothorax following self-induced oral injury: Report of four cases and review of the literature. Chest 2001; 120: 306-309.
6. Kuniyoshi Y, Kamura A, Yasuda S et al.: Laryngeal Injury and Pneumomediastinum Due to Minor Blunt Neck Trauma: Case Report. J Emerg Med 2017; 52(4): 145-148.
7. Lee SW, Huh YH, Cha MS: Iatrogenic subcutaneous cervicofacial emphysema with pneumomediastinum after class V restoration. J Korean Assoc Oral Maxillofac Surg 2017; 43: 49-52.
8. Kaliszewski K, Cendal I, Krassowska M et al.: Pneumomediastinum and subcutaneous emphysema after dental extraction. Pol Arch Intern Med 2020; 130(3): 244-245.
9. Zieliński R, Piotrowska V, Zakrzewska A: Pneumomediastinum and emphysema in a case of a soft bronchial foreign body aspiration in a child. A case report. Otolaryngol Pol 2011; 65(1): 59-61.
10. Piotrowski S, Jesikiewicz D: Mediastinal emphysema as a complication of the tonsilloadenotomy in child. Otolaryngol Pol 2009; 63(6): 528-531.
11. Dubost J, Kalfon F, Roullit S et al.: Giant subcutaneous emphysema, pneumomediastinum and bilateral pneumothorax following rhinoseptoplasty. Cah Anesthesiol 1986; 34(2): 161-162.
12. Gulati A, Baldwin A, Intosh IM, Krishnan A: Pneumomediastinum, bilateral pneumothorax, pleural effusion, and surgical emphysema after routine apicectomy caused by vomiting. Br J Oral Maxillofac Surg 2008; 46: 136-137.
13. van Veelen I, Hogeman PH, van Elburg A: Pneumomediastinum: A rare complication of anorexia nervosa in children and adolescents: A case study and review of the literature. Eur J Pediatr 2008; 167: 171-174.
14. Tomczak M, Twardosz K, Szelerska-Twardosz H: Pneumomediastinum as a result amphetamin administration. Pneumonol Alergol Pol 2005; 73: 76.
15. Macia I, Moya J, Ramos R et al.: Spontaneous pneumomediastinum: 41 cases. Eur J Cardiothorac Surg 2007; 31: 1110-1114.
16. Caceres M, Ali SZ, Braud R et al.: Spontaneous pneumomediastinum: a comparative study and review of the literature. Ann Thorac Surg 2008; 86: 962-966.
17. Huon LK, Chang YL, Wang PC, Chen PY: Head and neck manifestations of spontaneous pneumomediastinum, Otolaryngol Head Neck Surg 2012; 146(1): 53-57.
18. Gasser CR, Pellaton R, Rochat CP: Pediatric Spontaneous Pneumomediastinum: Narrative Literature Review. Pediatr Emerg Care 2017; 33(5): 370-374.
19. Takada K, Matsumoto S, Hiramatsu T et al.: Spontaneous pneumomediastinum: an algorithm for diagnosis and management. Ther Adv Respir Dis 2009; 3: 301-307.
20. Takada K, Matsumoto S, Hiramatsu T et al.: Management of spontaneous pneumomediastinum based on clinical experience of 25 cases. Respir Med 2008; 102: 1329-1334.
21. Dissanaike S, Shalhub S, Jurkovich GJ: The evaluation of pneumomediastinum in blunt trauma patients. J Trauma 2008; 65(6): 1340-1345.
22. Zhang XY, Zhang WX, Sheng AQ et al.: Diagnosis and prognosis of spontaneous pneumomediastinum in eighteen children. Zhonghua Er Ke Za Zhi 2013; 51(11): 849-851.
23. Zachariah S, Gharahbaghian L, Perera P, Joshi N: Spontaneous pneumomediastinum on bedside ultrasound: case report and review of the literature. West J Emerg Med 2015; 16(2): 321-324.
24. Beason HF, Markowitz JE: Pneumomediastinum Diagnosed on Ultrasound in the Emergency Department: A Case Report. Perm J 2015; 19(3): 122-124.
25. Chalumeau M, Le Clainche L, Sayeg N et al.: Spontaneous pneumomediastinum in children. Pediatr Pulmonol 2001; 31(1): 67-75.
26. Muckart DJJ, Hardcastle TC, Skinner DL: Pneumomediastinum and pneumopericardium following blunt thoracic trauma: much ado about nothing? Eur J Trauma Emerg Surg 2019; 45(5): 927-931.
27. McGuinness G, Zhan Ch, Rosenberg N et al.: Increased Incidence of Barotrauma in Patients with COVID-19 on Invasive Mechanical Ventilation. Radiology 2020; 297(2): 252-262.