© Borgis - New Medicine 3/2003, s. 49-52
Marzenna Zielinska, Krzysztof Kaczmarek, Jan Krekora, Wlodzimierz Koniarek
Early clinical results of primary angioplasty and stenting in acute myocardial infarction in the elderly
Department of Cardiology, Institute of Cardiology, Medical University of Lodz, Poland
Head: prof. Halina Bolinska-Soltysiak, MD, PhD
Summary
Acute myocardial infarction (AMI) is one of the main causes of death in advanced age. Primary angioplasty (PTCA) is the best method of treatment in young patients. Its effectiveness in elderly patients is unclear.
The aim of this study was to compare early results of invasive treatment of AMI with conservative therapy, in elderly patients.
Study group and methods: We analysed 175 pts (=75 years old) hospitalised due to AMI. Patients were divided according to their treatment into: group I (92 pts) subjected to primary PTCA, and group II (88 pts) treated conservatively. We compared the clinical characteristics and early clinical outcomes in both groups.
Results: The baseline characteristics of the groups were comparable. Only the incidence of hypertension and history of previous myocardial infarction differed between groups. The hospital outcome in group II was more frequently complicated by heart failure (29.55% vs. 15.21%, p<0.001) or by cardiogenic shock (31.82% vs. 11.96%). The hospital death rate was significantly higher in group II (37.5% vs. 17.4%), and was associated first of all with cardiogenic shock. Atrio-ventricular conduction disturbances (21.59% vs. 7.6%) and reinfarction (6.81% vs. 3.26%) were also more frequent in the conservatively treated pts.
Hospital stay was significantly shorter in group I (10.7 vs. 17.0 days).
Conclusions: 1. Primary PTCA in the elderly seems to be a safer method and more effective than conservative therapy. 2. Primary PTCA significantly decreases mortality in the elderly in comparison to conservative therapy. 3. Cardiogenic shock remains the most important risk factor in predicting the outcome of AMI in the elderly.
INTRODUCTION
Acute myocardial infarction (AMI) is one of the main causes of death in advanced age. In addition to anterior myocardial infarction, a heart rate over 100/min, evident circulatory insufficiency, and systolic blood pressure below 100 mmHg, an age of over 70 years is a factor that puts patients (pts) into an increased risk group (1, 2). In-hospital as well as follow-up mortality is significantly higher in this group of patients than in lower risk groups, and is independent of the method of treatment (2, 3, 4).
In younger pts, the management of choice (confirmed by follow-up observations) in AMI seems to be primary coronary angioplasty (PTCA) with simultaneous stent implantation (1, 5, 6, 7, 8, 9, 10, 11). As defined studies have not been carried out in the elderly, there is no clearly defined optimal method of AMI management for them.
In this study, we report the clinical outcomes of primary PTCA in elderly pts (=75 years) with AMI, and compare these results with those of conservative treatment in similar series of pts.
METHODS
Study group: 180 patients, 75 years or older, hospitalised due to AMI, were subjected to retrospective analysis. The criteria for acute myocardial infarction diagnosis were: occurrence of typical chest pain lasting over 30 min, with accompanying typical changes on the electrocardiogram (ST segment elevation about 2 mm in at least two neighbouring leads) or acute left bundle branch block. If other changes were observed in the initial electrocardiogram (e.g. negative T waves, ST segment depression), pathological CK-MB and/or troponin elevation were the criteria for AMI diagnosis. The pts were divided into 2 groups according to their treatment. Group I included patients treated with PTCA of the infarct-related artery (IRA). Group II comprised patients treated conservatively.
Invasive therapy: Based on emergency coronarography, PTCA was most frequently undertaken with simultaneous stent implantation. PTCA was considered to be effective when TIMI 3 – flow with a residual stenosis of not greater than 30% was obtained. If there were no contraindications, the pts with stent implatantion were treated with Abciximab (Reo-Pro).
Conservative therapy: These pts received typical conservative treatment, including heparin if there were no contraindications. No pts were subjected to fibrinolytic treatment.
Clinical assessment: During hospital stay, pts were monitored for the occurrence of major cardiac events such as death, re-infarction, shock, stroke or symptoms of congestive heart failure. The occurrence of psychomotor disturbances connected with central nervous system hypoxia, pneumonia, or major bleeding were analysed. We also noted the length of stay in hospital, for members of both groups.
Statistical analysis: Continuous variables are expressed as mean±SD. Group comparisons used Student´s T-test or c?2 test, as appropriate. P=0.05 was considered to be statistically significant.
RESULTS
Ninety-two patients from Group I, aged 75-92 years (mean 78.82±3.32), were subjected to invasive treatment. Group II comprised 88 patients, aged 75-92 years (mean 80.37±4.22). The basic characteristics of the groups were comparable. Admission demographic and clinical characteristics are listed in Table 1. Note that in the PTCA group, ST segment elevation AMI (91.3% vs. 61.96%) and AMI with Q wave (79.35% vs. 68.21%) were diagnosed more often. PTCA was successful in 78 patients (84.8%) of group 1. A stent was used in 69 patients (88.5%).
Table 1. Demographic and clinical characteristics of elderly patients with AMI.
| | Group I (PCI patients)
N = 92 | Group II(patients on conservative therapy)N = 88 | |
| Age (years) | 78.82 ? 3.32 | 80.37 ? 4.22 | NS |
| Female | 47 (51.09%) | 50 (56.82%) | NS |
| ST elevation AMI | 84 (91.3%) | 54 (61.96%) | P < 0.001 |
| Q wave AMI | 73 (79.35%) | 60 (68.21%) | NS |
| Infarction location | | | |
| Antero-lateral | 49 (53.26%) | 45 (51.14%) | NS |
| Postero-inferior | 43 (46.74%) | 39 (44.32%) | NS |
| LBBB | | 4 (4.54%) | |
| Risk factors | | | |
| Hypertension | 55 (59.78%) | 42 (47.72%) | P < 0.05 |
| Diabetes | 33 (35.87%) | 26 (29.54%) | NS |
| Hyperlipidaemia | 41 (44.61%) | 36 (40.68%) | NS |
| Smoking | 21 (23.08%) | 27 (30.68%) | NS |
| Family history | 14 (15.28%) | 6 (6.82%) | NS |
| Previous infarction | 20 (21.73%) | 38 (43.18%) | P < 0.001 |
| Previous stroke | 12 (13.04%) | 11 (12.5%) | NS |
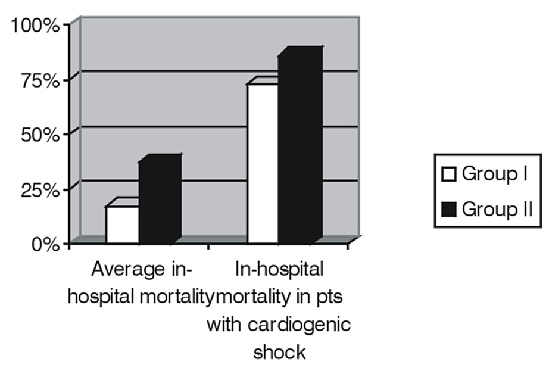
Clinical outcome: In-hospital mortality was significantly higher in the group with conservative treatment (37.5% in Group II vs. 17.39% in Group I). The difference (Fig.1) was less pronounced among patients with cardiogenic shock on admission (85.7% vs. 72.7%).
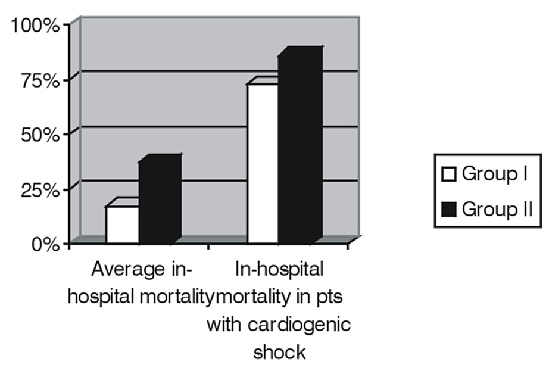
Fig. 1. In-hospital mortality in eldery patients with AMI.
Compared with patients who underwent primary PTCA, conservatively treated patients had a significantly higher incidence of heart failure symptoms such as pulmonary oedema and cardiac asthma (29.55% vs. 15.21%), or the occurrence of cardiogenic shock (31.82% vs. 11.96%). Atrio- ventricular conduction disturbances were observed more frequently in the conservatively treated group (21.59% vs. 7.6%). The incidence of in-hospital pneumonia (18.8% vs. 20.45%) and central nervous system hypoxia symptoms (13.04% vs. 14.77%) were similar in both groups. Detailed results are presented in tables 2 and 3.
The average duration of hospital stay was significantly shorter in the PCI group (10.7 vs. 17.0 days).
DISCUSSION
The elderly population is characterised by more advanced atheromatosis, and thus more frequent coronary disease. Moreover, this population is more severely burdened with risk factors. In PAMI I an age>65 years was believed to be an independent risk factor for increased mortality in AMI (3). Also, cardiogenic shock develops more frequently in this group (2, 12, 13, 14, 15). In PAMI I, ZWOLLE and Mayo Clinic meta-analyses, a significant decrease in mortality was observed among patients treated with primary angioplasty as compared to these treated with thrombolysis (12, 17). A similar mortality decrease in patients over 70 years of age was registered in GUSTO Iib (14). However, the inclusion criteria for these studies excluded patients with contraindications for the administration of fibrinolytic drugs. There been no randomised studies comparing PTCA with conservative therapy (to which the majority of patients are subjected, due to the impossibility of fibrinolytic treatment) (16).
Table 2. In-hospital clinical outcome in elderly patients with AMI.
| | Group I (PCI patients)N = 92 | Group II
(conservative therapy patients)N = 83 | |
| Duration of hospi-tal stay (days) | 10.6 ? 4.7 | 17.0 ? 9.3 | P < 0.001 |
| In-hospital mortality In-hospital mortality in patients with cardiogenic shock | 16 (17.39%)8/11 (72.7%) | 33 (37.5%)24/28 (85.7%) | P < 0.001NS |
| Complications of AMI | | | |
| Cardiogenic shock | 11 (11.96%) | 28 (31.82%) | P < 0.001 |
| Pulmonary oedema and/or cardiac asthma | 14 (15.21%) | 26 (29.55%) | P < 0.001 |
| Ventricular tachycardia in first 24 hours | 13 (14.12%) | 10 (11.36%) | NS |
| Atrio-ventricular block II/III degree | 7 (7.6%) | 19 (21.59%) | P < 0.001 |
| Re-infarction | 3 (3.26%) | 6 (6.81%) | NS |
| Other complications | | | |
| Pneumonia | 17 (18.48%) | 18 (20.45%) | NS |
| Stroke | 6 (6.52%) | 2 (2.27) | NS |
| Consciousness disturbances | 12 (13.04%) | 13 (14.77) | NS |
| Bleeding requiring transfusion | 3 (3.26%) | - | P < 0.001 |
Table 3. Results of primary PTCA in elderly patients with AMI.
| | Group I (N = 92) |
| Successful angiography | 91 (98.91%) |
| Effective PTCA | 78 (84.78%) |
| Stent implantation | 69 (75%) |
| Reo-Pro | 31 (33.69%) |
| Heparin | 37 (40.22%) |
| Early re-occlusion | 3 (3.26%) |
| Bleeding | 3 (3.26%) |
| Local haematoma | 4 (4.35%) |
The results of invasive treatment in elderly patients are often compared to those obtained from younger patients. All comparisons clearly emphasise higher mortality and more complications in elderly patients (14, 16, 18).
Our studies demonstrated a significantly lower mortality in the elderly group subjected to invasive treatment, compared to those on conservative therapy. In these patients, re-infarction and symptoms of heart failure were observed less frequently. PTCA patients did not have any further complications, such as pneumonia or consciousness disturbances, thus confirming the safety of the used procedure.
In the majority of studies made thus far, patients with cardiogenic shock have been distinguished as a subgroup at particularly increased risk. All over the world, primary angioplasty has resulted in a significant decrease of mortality (about 30%) in this subgroup, compared to patients subjected to conservative or fibrinolytic therapy (about 80%) (6, 19, 20). However, these observations do not concern advanced age patients. In our group only a slight decrease in mortality was observed in the subgroup of PTCA patients when compared to a similar group on conservative therapy. However, these observations concern a very small group. Cardiogenic shock seems to be the most serious prognostic complication of myocardial infarction in advanced age patients.
CONCLUSIONS
1. Primary angioplasty in patients of advanced age with acute myocardial infarction seems to be a safe method and more effective than conservative therapy.
2. Primary angioplasty significantly decreases mortality in elderly patients with acute myocardial infarction, as compared to conservative treatment.
3. No significant superiority of invasive treatment over conservative therapy was observed in patients with myocardial infarction complicated by cardiogenic shock. Cardiogenic shock remains the most serious prognostic factor affecting the outcome of myocardial infarction in advanced age patients.
Piśmiennictwo
1. Grines C.L. et al.: A randomized trial of transfer for primary angioplasty versus on-site thrombolysis in patients with high-risk myocardial infarction. The air primary angioplasty in myocardial infarction study. J. Am. Coll. Cardiol. 2002; 39:1713-9. 2. Batchelor W.B. et al.: Contemporary outcome trends in the elderly undergoing percutaneous coronary interventions: Results in 7,472 Octogenarians. J. Am. Coll. Cardiol. 2000; 36:723-30. 3. DeGeare V.S. et al.: Angiographic and clinical characteristics associated with increased in-hospital mortality in elderly patients with acute myocardial infarction undergoing percutaneous intervention (A pooled analysis of the primary angioplasty in myocardial infarction trials). Am. J. Cardiol. 2000; 86:30-34. 4. Lee K.L. et al.: Predictors of 30-day mortality in the era of reperfusion for acute myocardial infarction: results from an international trial of 41,021 patients. Circulation 1995; 91:1659-68. 5. Weaver W.D. et al.: Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction: a quantitative rewiev. JAMA 1997; 278:2093-2098. 6. Zahn R. et al.: Primary angioplasty versus intravenous thrombolysis in acute myocardial infarction: Can we define subgroups of patients benefiting most from primary angioplasty? Results from the pooled data of MITRA and MIR. J. Am. Coll. Cardiol. 2001; 37:1827-35. 7. Maynard Ch. et al.: Comparison of outcomes of coronary stenting versus conventional coronary angioplasty in the department of Veterans Affairs Medical Centers. Am. J. Cardiol. 2001; 87:1240-1245. 8. Antoniucci D. et al.: Relation of time to treatment and mortality in patients with acute myocardial infarction undergoing primary angioplasty. Am. J. Cardiol. 2002; 89:1248-1252. 9. Fibrinolytic Therapy Trialist (FTT) Collaborative Group. Indications for fibrinolytic therapy in suspected acute myocardial infarction; collaborative overview of early mortality and major morbidity results from all randomized trials of more than 1000 patients. Lancet 1994; 343: 311-322. 10. White H.B. et al.: Age and outcome with contemporary thrombolytic therapy: results from the GUSTO-1 trial. Global Utilisation of Streptokinase and TPA for Occluded Coronary Arteries Trial. Circulation 1996; 94: 1826-1833. 11. Thiemann D.R. et al.: Lack of benefit for intravenous thrombolysis in patients with myocardial infarction who are older than 75 years. Circulation 2000; 101:2239-2246. 12. De Boer M.J. et al.: Reperfusion therapy in elderly patients with acute myocardial infarction. A randomized comparison of primary angioplasty and thrombolytic therapy. J. Am. Coll. Cardiol. 2002; 39:1723-8. 13. Lee T.C. et al.: Emergency percutaneous transluminal coronary angioplasty for acute myocardial infarction in patients 70 years of age and older. Am. J. Cardiol. 1990; 66:663-667. 14. Matetzky S. et al.: Primary angioplasty for acute myocardial infarction in octogerians. Am. J. Cardiol. 2001; 88:680-683. 15. Klein L.W. et al.: Percutaneous coronary interventions in octogenarians in the American College of Cardiology – National Cardiovascular Data Registry. Development of a nomogram predictive of in-hospital mortality. J. Am. Coll. Cardiol. 2002; 40:394-402. 16. Devlin W. et al.: Comparison of outcome in patients with acute myocardial infarction aged> 75 years with that in younger patients. Am. J. Cardiol. 1995; 75:573-576. 17. O´Neill W.W. et al.: Lessons from the pooled outcome of the PAMI, Zwolle and Mayo clinic randomized trials of primary angioplasty versus thrombolytic therapy of acute myocardial infarction. J. Invasive Cardiol. 1998; 10: 4-10. 18. Kochman W. et al.: Ostry zawał serca u pacjentów powyżej 70 lat leczonych za pomocą pierwotnej angioplastyki. Folia Cardiol. 2002; 9:443-450. 19. Goldberg R.J. et al.: Cardiogenic shock after acute myocardial infarction. Incidence and mortality from a community – wide perspective, 1975-1988. N. Engl. J. Med. 1991; 325:1117-1122. 20. Webb J.G. et al.: Percutaneous coronary intervention for cardiogenic shock in the SHOCK Trial Registry. Am. Heart J. 2001; 141:964-70.