© Borgis - New Medicine 3/2003, s. 45-48
Andrzej Walczak1, Janusz Zaslonka1, Alicja Iwaszkiewicz1, Ryszard Jaszewski1, Marzenna Zielinska2, Slawomir Jander1, Leszek Markuszewski1, Stanislaw Ostrowski1
Valvular heart disease and comorbid ischemic heart disease in patients over 65 years old
1 Department of Cardiac Surgery, Institute of Cardiology, Medical University of Lodz, Poland
Head: prof. Janusz Zaslonka, MD, PhD
2 Department of Cardiology, Institute of Cardiology, Medical University of Lodz, Poland
Head: prof. Halina Bolinska-Soltysiak, MD, PhD
Summary
Background: Aging of societies is a worldwide tendency which concerns also the Polish population. Thus, patients referred to the surgery are older and older.
Material and methods: All valve replacements performed in the Department of Cardiac Surgery, Medical University of Łódź, between 1999 and 2002, were analyzed in the study. Patients older than 40 years, who were qualified to valve replacement under cardiopulmonary by-pass, underwent routine coronary angiography in order to assess their coronary circulation. Two groups of patients, under and over 65 years of age were compared from the point of view of an incidence of coronary arteries lesions and a need of myocardial revascularization. Totally, 1117 patients with valve replacement were analyzed
Results: In 15% (172 patients) of the whole analyzed group, simultaneous surgical myocardial revascularization was performed. In the subset of patients in whom it was necessary to perform CABG, persons over 65 made up 51%. Revascularization procedures more frequently accompanied AVR than MVR (60% vs. 40%). In the subset of patients over 65 who underwent combined procedures of valve replacement and CABG, women were twice as numerous as in the subset of younger patients.
Conclusions: Along with aging, an incidence of comorbid ischemic heart disease increases, what significantly rises a risk of the surgery (especially of mitral valve). It should be emphasized that some of the patients with advanced valvular disease do not suffer from typical sings of ischemic heart disease (angina) what is connected with their poor exercise tolerance.
Background
The worldwide population rapidly ages and this process concerns especially highly developed countries. In 1990, more than 31 million Americans were > 65, nearly twice as many as in 1960. This number is estimated to reach> 53 million by 2020, and> 75 million by 2040. The proportion of the total population > 65 is projected to grow from about 12.5% in 1996 to about 20% by 2040. On the other hand it is known that the incidence of ischemic heart disease increases along with aging. Post mortem data show that in 60% of people who died at the age of 60 or older, there are significant (stenosis of 75% or greater) lesions in coronary arteries. Besides, elderly patients often suffer from an asymptomatic form of the ischemic heart disease (1, 2).
Patients who undergo valve replacements are also older and older. A mean age of patients operated upon because of valvular heart disease which in 1986 had been 58.6 years, in 2000 reached 66 years – the data from United Kingdom Heart Valve Registry (UKHVR) (3).
In the study, we tried to analyze an incidence of comorbid ischemic heart disease in the population of patients over 65 who were operated upon due to valvular heart disease.
Material and methods
All cases of valve replacement (1117) performed in the Department of Cardiac Surgery, Institute of Cardiology, Medical University of Łódź, between 1999 and 2002, were analyzed. This group of patients consisted of 603 women (53.98%) and 514 men (46.02%) at a mean age of 58.13 ± 10.78 years (range from 21 to 79 years). Aortic valve replacement (AVR) was performed in 496 patients, mitral valve replacement (MVR) in 529 patients and tricuspid valve replacement (TVR) in 10. Eighty patients underwent double valve replacement and 2 patients had triple valve replacement performed. Clinical data of these patients are shown in Table 1. All valvular prosthesis implanted were mechanical ones. Bileaflet valves were used most frequently (in 89.79% of cases). All patients over 40 (and all patients with a coronary history independently of age) who had been qualified to any valve replacement, underwent coronary angiography before the operation. When significant lesions in coronary arteries (75% or greater and 50% or greater in left main stem) were observed, the patients were referred to simultaneous myocardial revascularization. The procedures were performed through median sternotomy, with routine cannulation of ascending aorta and right atrium, under cardiopulmonary by-pass. Cold crystalloid cardioplegia St. Thomas Hospital was administered to aortic bulb or directly to coronary ostia when aortic valve was replaced. A routine initial dose of cardioplegia was 1000 ml, and it was replenished if necessary every 30 minutes with another 200-300 ml. Valvular prostheses were implanted with interrupted mattress sutures with Teflon pads. Myocardial revascularization was performed using coronary artery by-pass grafting (CABG). When there was a significant lesion in left anterior descending (LAD) artery, a pedunculated left internal thoracic artery (LITA) was used as a graft of choice. Other coronary grafts were performed using a section of saphenous vein.
Table 1. The clinical characteristics of the operated patients.
| | n (%) | female n (%) | male n (%) | age range - years | mean age years ? SD | % pts = 65 years |
| AVR | 496 (44.40) | 179 (36.09) | 317 (63.91) | 21 - 78 | 58.97 ? 11.47 | 38.27 |
| MVR | 529 (47.36) | 376 (71.08) | 153 (28.92) | 21 - 79 | 57.49 ? 10.08 | 29.90 |
| TVR | 10 (0.90) | 5 (50) | 5 (50) | 35 - 75 | 55.00 ? 13.66 | 30.00 |
| A + MVR | 79 (7.07) | 40 (50.63) | 39 (49.37) | 25 - 75 | 57.20 ? 10.30 | 28.21 |
| A + TVR | 1 (0.09) | 1 | - | - | 68 | 100 |
| A + M + TVR | 2 (0.18) | 2 (100) | - | 62 - 73 | 67.50 ? 7.79 | 100 |
| Total | 1117 | 603 (53.98) | 514 (46.02) | 21 - 79 | 58.13 ? 10.78 | 33.67 |
AVR – aortic valve replacement, MVR – mitral valve replacement, TVR – tricuspid valve replacement, A + MVR – aortic and mitral valve replacement, A + TVR – aortic and tricuspid valve replacement, A + M + TVR – aortic, mitral and tricuspid valve replacement
Results
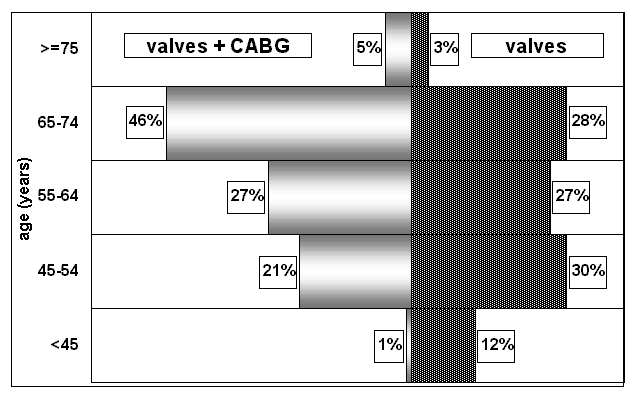
In the analyzed group of 1117 patients who underwent valve replacement, 172 (15%) had simultaneously myocardial revascularization performed. Clinical data of patients operated upon with and without simultaneous CABG are shown in Table 2. A mean age of the patients with valve replacement and CABG was 62.36 ± 8.28 years (range from 35 to 78 years) and it was higher than a mean age of the patients with valve replacement alone (57.38 ± 11.0, range from 21-79 years). Distributions of age in both above mentioned groups are shown in Figu-re 1. Elderly patients (over 65 years) made up 31.43% of the patients who underwent valve replacement alone, and as many as 52% of the patients with simultaneous revascularization. In the group of 172 patients with CABG following valvular procedures were performed: AVR in 104 patients (60.46%); MVR in 64 (37.21%) and AVR+MVR in 4 (2.33%). A mean number of grafts per one patient in this group was 1.89 ± 1.0 what is a lower value than mean number of grafts in patients undergoing CABG alone (2.8 in our center in 2002). One graft was performed in 45% of the patients – two, three, four and five grafts were made in 28%, 19%, 6% and 1% of the patients, respectively. Detailed data on performed grafts are shown in Table 3. When it was necessary to graft left anterior descending artery LITA was used in 97% of the cases. In the group of patients over 65, a mean number of grafts per one patient was 1.86 ± 1.08.
Table 2. The characteristics of the patients operated upon due to valvular disease alone and due to valvular disease with comorbid ischemic heart disease.
| | n (%) | female n (%) | male n (%) | age range - years | mean age years ? SD | % pts = 65 years |
| Valve replacement | 945 (84.60) | 548 (57.99) | 397 (42.01) | 21 - 79 | 57.38 ? 11.00 | 31.43 |
| CABG and valve replacement | 172 (15.40) | 55 (31.98) | 117 (68.02) | 35 - 78 | 62.36 ? 8.28 | 51.74 |
| Total | 1117 (100) | 603 (53.98) | 514 (46.02) | 21 - 79 | 58.13 ? 10.78 | 33.67 |
CABG – coronary artery bypass grafting
Table 3. The data on coronary grafts performed in the patients below and over 65.
| | ł
65 | < 65 | całość |
| Number of pts | 89 | 83 | 172 |
| anastomoses/pts | 1.86 ? 1.08 | 1.91 ? 0.92 | 1.89 ? 1.00 |
| LAD | 61.84% | 58.43% | 60.00% |
| RM | 1.32% | 1.12% | 1.21% |
| Dg | 13.16% | 15.73% | 14.55% |
| Mg | 51.32% | 51.69% | 51.52% |
| RCA and branches | 46.05% | 60.67% | 53.94% |
LAD – left anterior descending, RM – ramus medianus, Dg – diagonal branches, Mg – marginal branches, RCA – right coronary artery
Discussion
Aging of societies is a worldwide tendency especially well seen in the developed countries of our globe. It is expected that by 2050 a number of the elderly will for the first time in the history of human race exceed a number of the youth. In the past decades, most cases of valvular heart disease was caused by rheumatic disease, but in spite of a significant reduction in its prevalence (especially in the developed countries) an incidence of valvular procedures did not decrease. It is mostly a result of changes in valvular disease etiology. Currently, one of the most important reasons of the disease are degenerative changes of valves (especially aortic one) – a process directly connected with life prolongation (4, 5). At present in the developed countries, aortic valve with degenerative changes is the one the most frequently replaced – according to UKHVR: 75% in 2000 compared with 55% in 1986 (3). In the third world countries, rheumatic disease remains the most frequent reason of valve replacement (4). Some differences can also be observed between the European Union countries. A comparison of valvular procedures in 1995, between the south (France, Italy, Spain) and the north (Germany, Sweden, Finland, Great Britain) of the continent, showed that patients operated in the southern countries are younger (62.2 vs. 64.5 years), more often undergo MVR (34.6% vs. 28.0%) and less frequently undergo AVR (64.4% vs. 72.7%). Simultaneous valvular and CABG procedures are also significantly less frequently performed in the southern countries than in the northern countries (15.7% vs. 30.7%) (6). A mean age of patients operated upon due to valvular heart disease in our center (58.13 years) is lower than in the European Union countries. We also more often perform MVR (47.64%), whereas our rate of simultaneous revascularization (15%) is similar to this of the southern European countries.
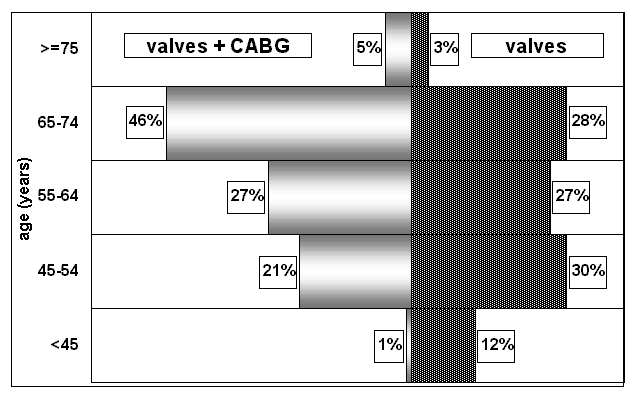
Fig. 1. The distribution of age in the patients operated upon due to valvular disease alone and due to valvular diseases with comorbid ischemic heart disease.
In all centers, patients referred to cardiac surgery are older and older, and on the other hand it is well known that a prevalence of ischemic heart disease increases along with age (1, 7).
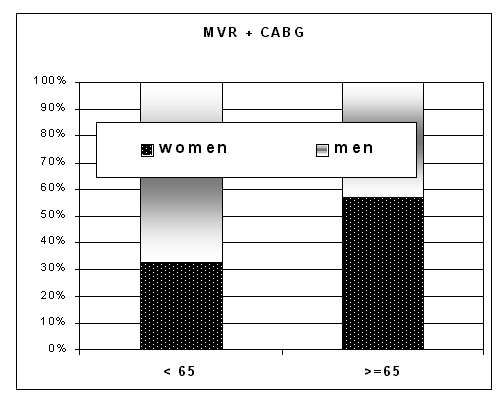
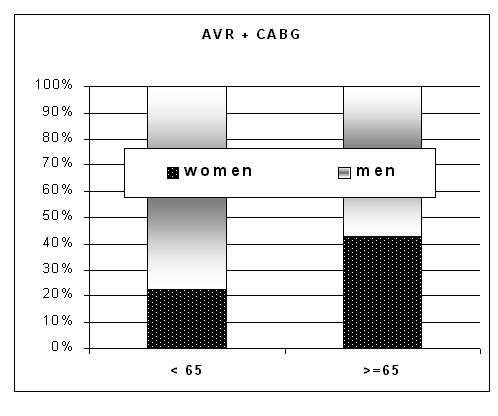
In the analyzed material, the patients in whom it was necessary to perform simultaneous revascularization were older than those with valvular replacement alone (62.36 vs. 57.38 years). Revascularization procedures more frequently accompanied AVR than MVR (60.46% vs. 37.21%). We also observed that in the subset of patients over 65 there were two-times more women who needed simultaneous CABG than in the subset of younger patients (Fig. 2).
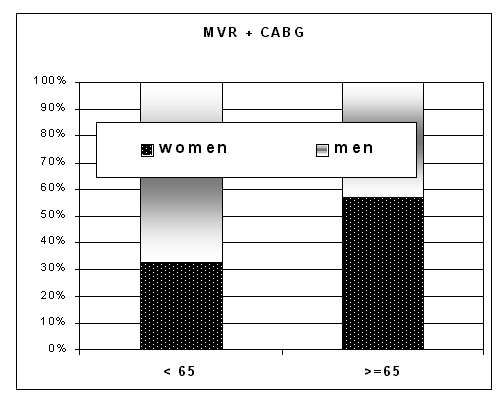
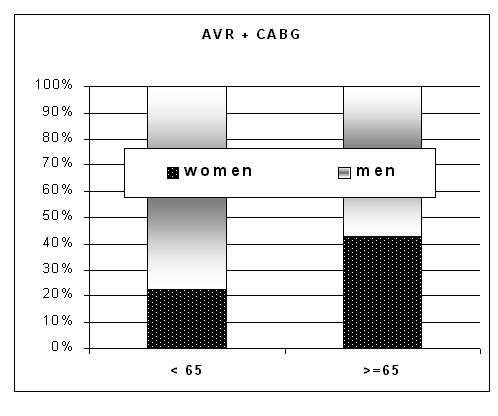
Fig. 2. The number of women (%) below and over 65 undergoing aortic valve replacement with simultaneous myocardial revascularization and mitral valve replacement with simultaneous myocardial revascularization.
Most of authors are concordant that when AVR is performed simultaneously with CABG a risk of such a procedure is similar to a risk of AVR alone (8, 9).
Combined mitral valve replacements and CABG are burdened with significantly higher mortality rate than above mentioned procedures performed alone (10, 11). One must to remember that elderly patients undergoing cardiac surgery are usually burdened with comorbid diseases, thus a risk of the operation is higher. Because of their limited exercise tolerance, patients with advanced valvular heart disease often do not suffer from typical symptoms of ischemic heart disease. In the analyzed clinical material, in 18% of the patients without a typical history of angina we found in coronary angiography significant lesions of coronary arteries which needed by-pass grafting. A necessity of performing coronary angiography prior to cardiac surgery in patients qualified to valvular replacement who are burdened with risk factors of ischemic heart disease (including age) is emphasized in ACC/AHA guidelines (12).
Analyzing mechanical prostheses used in our group, we found that 90% of them were bi-leaflet valves. Currently, such prostheses are the most frequently used by cardiac surgeons all around the world. For example, similar high rate of bi-leaflet valves implanted was reported in Great Britain (UKHVR) (3).The high rate of grafting LAD artery with use of LITA in our material (97%) is concordant with other authors´ reports. Analyzing valve replacement procedures with simultaneous myocardial revascularization, Gall et al. did not find an increase of operative risk while using LITA grafts compared with using saphenous vein grafts and they emphasized better long-term survival in patients with arterial revascularization (63% vs. 42% after 5 years) (13). Similar data were published by Bauer et al. who also did not observe differences in early outcome with and without using LITA in combined valve replacement/revascularization procedures (14).
Due to increasing number of elderly people and rising along with age prevalence of ischemic heart disease and degenerative heart valve disease, this group of patients is going to be more and more numerously qualified to cardiac surgery. This is going to become a real challenge for a whole team of cardiologists and cardiac surgeons.
Conclusions
Along with aging, an incidence of comorbid ischemic heart disease increases, what significantly rises a risk of the surgery (especially of mitral valve).
It should be emphasized that some of the patients with advanced valvular disease do not suffer from typical sings of ischemic heart disease (angina) what is connected with their poor exercise tolerance.
Piśmiennictwo
1. Melvin D.,Cheitlin M.: Cardiovascular physiology– changes with ageing. Am. J. Geriatr. Cardiol. 2003; 12:9-13. 2. Pretre R., Turina M.I.: Valve disease: cardiac valve surgery in the octogenarian. Heart 2000; 83:116-121. 3. Taylor K.: Trends in mortality after heart valve replacement surgery – data from the United Kingdom Heart Valve Registry (UKHVR). Cardiac Surgery Today 2003; 1:2-10. 4. Soler-Soler J., Galve E.: Worldwide perspective of valve disease. Heart 2003; 83:721-725. 5. Rahimtoola S.H., Frye R.L.: Valvular heart disease. Circulation 2000; 102:24IV-33. 6. Roques F. et al.: Regional differences in surgical heart valve disease in europe: comparison between northern and southern subsets of the EuroSCORE database. J. Heart Valve Dis. 2003; 12:1-6. 7. Iung B.: Interface between valve disease and ischaemic heart disease. Heart 2000; 84:347-352. 8. Hilton T.C.: Aortic valve replacement for patients with mild to moderate aortic stenosis undergoing coronary artery bypass surgery. Clin. Cardiol. 2000; 23:141-147. 9. Brunvand H. et al.: Coronary artery bypass grafting combined with aortic valve replacement in healthy octogenarians does not increase postoperative risk. Scand. Cardiovasc. J. 2002; 36:297-301. 10. Thourani V.H. et al.: Influence of concomitant cabg and urgent/emergent status on mitral valve replacement surgery. Ann. Thorac. Surg. 2000; 70:778-783. 11. Ruvolo G. et al.: Combined coronary bypass grafting and mitral valve surgery: early and late results. Thorac. Cardiovasc. Surg. 1995; 43:90-93. 12. Bonow R.O. et al.: ACC/AHA guidelines for the management of patients with valvular heart disease: a report of the American college of cardiology/American heart association task force on practice guidelines (Committee on Management of Patients with Valvular Heart Disease). J. Am. Coll. Cardiol. 1998; 32:1486-1588. 13. Gall S. Jr et al.: Efficacy of the internal mammary artery in combined aortic valve replacement-coronary artery bypass grafting. Ann. Thorac. Surg. 2000; 69:524-530. 14. Bauer E.P. et al.: Valve surgery combined with coronary artery operation: is the use the of internal mammary artery a predictor for early complications? Eur. J. Cardiothorac. Surg. 1996; 10:248-252.