© Borgis - New Medicine 4/2004, s. 105-108
Małgorzata Kaczorowska, Lidia Mikołajewska, Agnieszka Woźniak, Juliusz Piotrowski, Zuzanna Łukaszewicz-Moszyńska, Kazimierz Niemczyk
Cochlear implants: qualification procedure in the paediatric population
ENT Department, Medical University of Warsaw, Poland
Head: Prof. Kazimierz Niemczyk MD, PhD
Summary
Children with profound deafness who obtain no benefit from hearing aids become candidates for cochlear implantation. Lack of acoustic stimulation in these patients results in irreversible inhibition of speech development and sound perception abilities. In the present paper the authors discuss the qualification procedure, current indications and contraindications for cochlear implantation in children.
INTRODUCTION
The prevalence of hearing loss>50 dB hearing level (HL) is about 1:1000 live births (2). In Poland, hearing impairment affects approximately 0.5% to 2% of children under 7 years of age (7).
Most children with impaired hearing can recognize speech through acoustic hearing aids. Nevertheless, some patients with profound deafness obtain no benefit from amplification devices. Additionally, lack of acoustic stimulation results in irreversible inhibition of speech development and sound perception abilities in infants and young children. Cochlear implantation is a well-recognized and effective option in the treatment of profound, bilateral deafness in these patients.
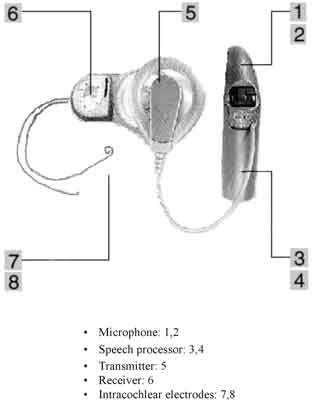
A cochlear implant is an electronic device which provides direct electrical stimulation to the auditory nerve, bypassing the nonfunctional cochlea. It consists of two main elements: an intracochlear electrode and a speech processor. A multi-electrode array is inserted into the cochlea, or, in the case of a malformed labyrinth (common cavity), it is applied to the surface of the inner ear. The speech processor converts sounds into electrical stimuli. CI devices may differ in the number and shape of electrodes, the mode of stimulation and speech-coding methods (7).
Implantation surgery consists of mastoidectomy, posterior tympanotomy to achieve an access to the labyrinth, drilling a cochleostomy and inserting the electrode array into the scala tympani. The operation requires general anesthesia. Four to six weeks after the surgery, the CI device is activated, and the first speech processor parameter fitting is done.
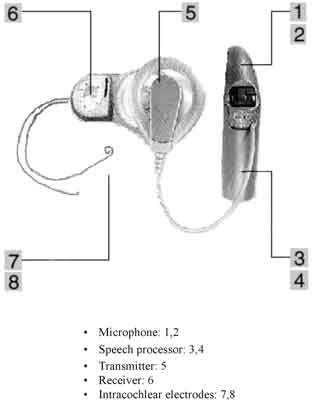
Fig. 1. Cochlear implant: a schematic representation of the device.
THE DIAGNOSIS OF DEAFNESS
The diagnosis of a profound sensorineural hearing loss should be established immediately after its onset. It is believed that congenital deafness should be recognized within the first 6 months of life (2, 7). At that time the child should be supplied with hearing aids. Early identification of children with congenital hearing impairment can be achieved by introducing a neonatal screening programme. The lack of response to environ-mental sounds and inhibition of speech development after the age of 6 months are strongly suggestive of hearing impairment. It is necessary to remember that the parents´ impression that their child does not hear is an indication to perform hearing tests.
Candidacy for CI implantation should be established as early as possible. Implanting young children immediately after the onset of profound hearing impairment enhances their achievements in hearing, speech and language development.
INDICATIONS FOR COCHLEAR IMPLANTATION
A severe-to-profound, bilateral sensorineural hearing loss of cochlear localization, and no or minimal speech perception which benefit from best-fitted hearing aids are an indication for cochlear implantation (6, 7).
QUALIFICATION FOR COCHLEAR IMPLANTATION
Preoperative assessment should entail otolaryn-gological, audiological, language speech pathology and rehabilitation as well as psychological evaluation. Prior to surgery, selected patients may require ophthalmo-logical and neurological consultations.
AUDIOLOGICAL EVALUATION
Audiological examination should address two issues: determination of the degree and type of hearing impairment and evaluation of the benefit from hearing aids.
The hearing status in young children is determined with the following two methods:
1. behavioural assessment
2. objective audiological tests:
– otoacoustic emission (OAEs)
– auditory brain stem response (ABR)
– acoustic immittance tests, including tympanogram and acoustic reflex thresholds.
The behavioural assessment of the hearing status evaluates the infant´s response to various types of sounds. The objective audiological tests do not require the child´s cooperation: each ear is tested individually, and the degree and localization of hearing impairment is precisely determined.
In older children, additional subjective audiological tests are used:
– play audiometry
– pure tone audiometry (PTA)
– free-field aided PTA
– free-field aided speech audiometry.
The subjective methods require the patient´s co-operation. However, in contrast to the objective exami-nations, those are functional tests which assess hearing (not an electrical response of the auditory system to a particular stimulus) (6).
AUDIOLOGICAL INCLUSION CRITERIA FOR COCHLEAR IMPLANTATION
Currently, the candidates for CI are recruited from among the children with a severe-to-profound (>90dB HL) bilateral sensorineural hearing loss of cochlear localization within the speech frequencies of 500-4000Hz. Additionally, no or minimal speech perception benefit obtained from the best-fitted hearing aids should be established (in older children, discrimination in open-set sentence or one-phoneme word tests should be <30%) (6).
Audiological evaluation represents only one stage in the decision-making process.
EVALUATION OF SPEECH PATHOLOGY AND REHABILITATION
Depending on whether the hearing impairment occurred before, during or after learning the language, the terms pre-, peri- or post- lingual deafness are used respectively. The language status correlates with the type of deafness. In children with the post-lingual deafness, the language development has been completed. The peri-lingual hearing impairment is related to different stages of language development and lack of speech automatism. In the pre-lingual deafness, the language has not been yet developed. Therefore, children with pre- and peri-lingually acquired deafness must not only make sense of auditory signals delivered by CI devices, but they must also use this information to develop speech and linguistic skills. Hearing training and speech rehabilitation are necessary conditions to accomplish effective postoperative performance.
Prior to cochlear implantation, the patient´s abilities to understand and produce speech are evaluated. The degree of hearing impairment, benefit from hearing aids and lip-reading skills are assessed in all patients. Similarly, the degree of language development is determined.
Pre- and peri- lingually deaf children require additional evaluation of such aspects as:
– development of communication skills
– readiness to communicate
– mode of communication (verbal or visual).
Since the rehabilitation process depends exclusively on parents, preoperative qualification assesses their attitude towards the problem. Accepting the child´s deafness by the parents and having realistic expectations are good prognostic factors. Intensive hearing training and speech rehabilitation provided immediately after the diagnosis has been established, are the necessary qualification conditions (9).
PSYCHOLOGICAL EVALUATION
On psychological consultation the children´s cognitive disability and behavioural disorders should be assessed. Autism is generally considered to be a contraindication for cochlear implantation. Behavioural and attention deficit disorders may have a significant impact on the auditory rehabilitation process (9).
IMAGING TECHNIQUES
The preoperative assessment consists of two visualization techniques of the inner ear and related structures, i.e. computed tomography (CT) and magnetic resonance imaging (MRI). CT shows bony structures of the inner ear most accurately, while MRI differentiates soft tissues. Both techniques are included in the qualification process to obtain two purposes:
1. to diagnose an inborn deformity or ossification of the inner ear, which helps choose an appropriate surgical access;
2. to confirm or exclude a presumed retrocochlear lesion (auditory nerve aplasia, NF2, posttraumatic injury).
It is worth remembering that a bony cochlear malformation has been reported to occur in 3% up to 20% of children with congenital sensorineural hearing loss. Ossification is usually a complication of meningitis and should be ruled out in all patients with a positive past medical history of meningitis (9).
AGE LIMITATION
Previously, the age of 3-2 years was believed to be the safe age limit for cochlear implantation. Nowadays, in many centers, the procedure has been performed in children under one year of age.
The mean performance correlates significantly with the child´s age at the implantation surgery. The best auditory results are achieved in patients implanted under one year of age, and the outcome is less satisfactory in older children. This may be interpreted as a reduction in the effect of auditory deprivation. However, an early cochlear implantation carries a higher risk in terms of anaesthetic exposure. Related to an underdeveloped respiratory system and inefficient thermoregulation, the complication rate shows a rise in very young children (4, 5, 9).
MENTAL RETARDATION
In the past, mental retardation was seen as an exclusion criterion in the selection procedure. Currently, mentally handicapped children are candidates for cochlear implantation. Although they benefit from cochlear implants in terms of sound awareness, sound identification and gradual language development, postoperative performance is significantly poorer as compared with that in children with normal cognitive development. Therefore the importance of realistic expectations of their parents and professional care providers toward this group of children is crucial (4, 9).
PROGNOSTIC PERFORMANCE FACTORS FOLLOWING COCHLEAR IMPLANTATION
Many studies have shown that implanted children achieve a wide range of hearing and speech abilities. Auditory performance ranges from the awareness of environmental sounds to understanding a conversation without lip-reading, and using a telephone.
Table 1. Speech perception score.
| Awareness of environmental sounds |
| Response to speech sound |
| Identification of environmental sounds |
| Discrimination of environmental sounds |
| Understanding common phrases without lip-reading |
| Understanding conversation without lip-reading |
| Use of telephone with a known speaker |
Three major predictive factors are related to the extent of the auditory experience gained in the so-called "sensitive period”:
– the age at implantation,
– the age at onset of deafness,
– duration of deafness.
It seems that the "sensitive period”, i.e. the time critical for language development, covers the first 6 years of life. Experimental researches have shown that lack of acoustic stimulation results in degenerative changes in the auditory system. Electrical stimulation with a CI device may partially prevent these abnormalities. Thus, the patient´s age at fitting a hearing aid and at cochlear implantation is crucial in successful language development.
Cochlear implantation in children under two years of age results in a better mean speech perception, speech production and language development. However, outstanding results may be achieved by children implanted at an older age. Nevertheless, even the best results gained by the CI patients fall behind the hearing level of their normal peers.
An early onset of hearing impairment results in pre- or peri- lingual deafness and inhibits the formation of auditory nerve pathways. Like long-term deafness, it is also a poor predictive factor. The majority of studies have shown a significant positive correlation between residual hearing and implant performance. Factors adversely affecting the language development and rehabilitation include concomitant mental or physical retardation and using the sign language by the patient (1, 3, 5, 9).
Nevertheless, the factors affecting the language development and the way they influence the outcome, are still not clearly understood. In each case, the so called "individual factors” may exert the main impact on hearing and speech abilities.
CONTRAINDICATIONS
Cochlear implantation is not a treatment option either in unilateral deafness or hearing impairment which may be effectively managed with hearing aids. Due to bilateral damage to the auditory nerve, deafness is a contraindication for cochlear implantation. The implan-tation is also contraindicated in autistic children. Neither is this mode of treatment recommended if the disabled child´s parents are not compliant and will not follow the rehabilitation programme after the operation since the patient will gain no or a very limited benefit from the CI surgery (9).
AUDITORY BRAIN STEM IMPLANT
Auditory brain stem implant (ABI) is an auditory implant which stimulates directly the cochlear nucleus in the brain stem. The electrode array is placed over the cochlear nucleus within the lateral recess of the fourth ventricle of the brain stem. Like a conventional CI device, an ABI also cooperates with a speech processor. The brain stem implant is suitable only in patients with bilateral damage to/complete dysfunction of the auditory nerve in which cochlear implantation is not effective. Therefore, ABI may not be an alternative option to hearing aids or cochlear implants. Indications for the auditory brain stem implantation include:
– bilateral 8 th nerve aplasia,
– bilateral acoustic neuroma; neurofibromatosis type 2 (NF2),
– bilateral posttraumatic 8 th nerve injury,
– acoustic neuropathy, unsuccessfully treated with a CI implant (9).
Piśmiennictwo
1. van Dijk J.E., Olphen A.F., Langereis M.C.: Predictors of Cochlear Implant Performance. Audiology 1999; 38:109-116. 2.Gelfan S.A.: Essentials of audiology. Thieme, New York, Stuttgart, 2001. 3.Gordon K.A., Daya H., Harrison R.V. et al: Factors contributing to open-set speech perception in children who use a cochlear implant. International Journal of Pediatric Otorhinolaryngology 2000; 56:101-111. 4. Lenarz T.: Cochlear implants: selection criteria and shifting borders. Acta Oto-Rhino-Laryngologica Belgica 1998; 52(3):183-99. 5.Osberger M.J., Zimmerman-Philips S., Koch D.B.: Cochlear implant candidacy and performance trends in children, Annals of Otology. Rhinology and Laryngology 2002; supplement. 189:62-5. 6.Piotrowska A., Lorens A., Szuchnik J.: Procedura diagnostyki przedoperacyjnej w leczeniu całkowitej głuchoty za pomocą implantu ślimakowego. Instytut Fizjologii i Patologii Słuchu, 2002. 7.Pruszyński A.: Zarys audiologii klinicznej. Wydawnictwa Akademii Medycznej im. Karola Marcinkowskiego w Poznaniu, Poznań, 2000. 8.Sanderson G., Nash L.S.: Outcomes beyond technology, Cochlear, 2001. 9.7th European Symposium "Paediatric Cochlear Implantation", 2-5 May 2004, Geneva, Switzerland - abstracts.