© Borgis - New Medicine 2/2014, s. 52-54
*Konrad Wroński1, 2
Male breast cancer – case report and review of literature
1Department of Oncology, Faculty of Medicine, University of Warmia and Mazury, Olsztyn, Poland
Head of Department: prof. Sergiusz Nawrocki, MD, PhD
2Department of Surgical Oncology, Hospital Ministry of Internal Affairs with Warmia and Mazury Oncology Centre, Olsztyn, Poland
Head of Department: Andrzej Lachowski, MD
Summary
Male breast cancer is rare malignant neoplasm. It accounts less than 1% of all types of cancer in male. The American Cancer Society calculate that the annual incidence rate of male breast cancer is 1.09 per 100.000 men compared with 68.73 per 100.000 women in the United States. Due to its low incidence and a limited number of men with breast cancer there have been no prospective randomized clinical trials and no clinical management target for male breast cancer.
In the following article the author described a case of a man who reported to the hospital because of male breast cancer. The patient underwent surgery and in the third day after operation left the ward. The author of this article has reviewed the literature on male breast cancer.
INTRODUCTION
Male breast cancer is rare malignant neoplasm. It accounts less than 1% of all types of cancer in male (1). The American Cancer Society calculate that the annual incidence rate of male breast cancer is 1.09 per 100.000 men compared with 68.73 per 100.000 women in the United States (2). Due to its low incidence and a limited number of men with breast cancer there have been no prospective randomized clinical trials and no clinical management target for male breast cancer.
CASE REPORT
A 57-year-old man, Caucasian race, was admitted to the Department of Surgical Oncology because of diagnosed breast male cancer. The patient suffer from hypertension which was effective treatment and under GP’s control. He had no history of alcohol consumption and he was no smoker. There was no familial history of breast cancer in patient’s family.
Blood examination tests were normal. On palpable examination of the left breast there was palpable tumor located in the subareolar region which diameter was about 3 cm. In the left axilla there were felt a few hard enlarged lymph nodes. The histopathological examination of the fine-needle aspiration biopsy of the tumor and lymph nodes showed cancer cells.
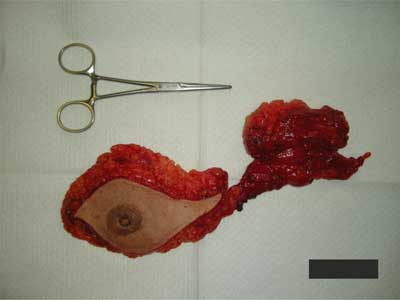
The patient was qualified for surgery. Taken surgery involving amputation of the left breast with neoplasm tumor and left axillary lymph nodes dissection in one block (fig. 1-5). The material was sent for routine histopathological examination (fig. 6). The time of surgery was about 110 minutes.

Fig. 1. Breast male cancer – photo taken during surgery.

Fig. 2. Cutting lines during surgery.

Fig. 3. Photo shows mastectomy due to breast male carcinoma.

Fig. 4. Photo shows the state after mastectomy and axillary lymph nodes dissection.

Fig. 5. The scar after left mastectomy with axillary lymph node dissection due to breast male cancer.
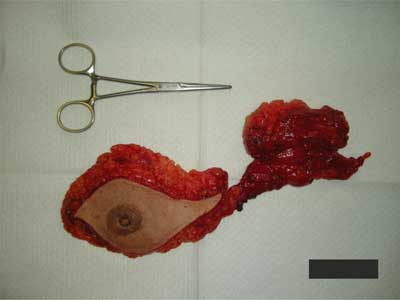
Fig. 6. Photo of the left breast with tumor and left axillary lymph nodes after dissection in one block.
Histopatological examination of postoperative material revealed: invasive ductal breast carcinoma G2, pT3 and 25 metastases in axillary lymph nodes. The stage of breast cancer according to pTNM classification was grade III c (pT2N3M0). Estrogen receptor positivity rate was 60% and progesteron positivity rate was 5%. HER2 was 0 and Ki-67 positivity rate was 40%.
Patient after surgery felt good and did not complain of pain. The postoperative period was uncomplicated and the patient left the ward in the third day after operation. The patient underwent chemotherapy and he is in the care of outpatient surgical oncology and clinical oncology.
DISCUSSION
The incidence of male breast cancer is still increase, but the reasons of this neoplasm is still unknown. Breast male cancer is observed often than normal in African, African-American and Ashkenazi Jewish population (3). In Sub-Africa region, breast male cancer is observed from 7% to 14% of all breast cancers (3). In whole male population, breast male cancer cases are less than 1% of all breast cancers (1). In population of Ashkenazi Jewish, the increased risk is due to a high incidence of BRCA1 and BRCA2 mutations (4).
15% to 20% breast male cancer patients have a family history of breast cancer (5). Familial mutation of BRCA plays important role in this cancer, but relations between mutation in breast male cancer in every country is different. In Southern California there are only 4% familial mutation of BRCA in male breast cancer but in Iceland there are 40% mutations (6).
Relation between endogenous estrogens and testosterone may increase risk of male breast cancer. Obesity causes imbalance between these two hormones. Men with body mass index higher than 30 kg/m2 have a higher risk of breast cancer (7).
Breast male cancer is more often observed in men who are exposure to ionizing radiation, high environmental temperature and chemicals (8, 9).
Male breast cancer is diagnosed at median age 68 years (10, 11). The majority of men feel palpable mass in the nipple area (10). The incidence of nipple involvement is observed in 40-50% patients and it is significantly higher than in female breast cancer (10, 11).
Diagnostic mammography in men has good sensitivity of 92-100% and specificity of 90% (2, 12). Mammography is ideal tool to diagnose male breast cancer and gynecomastia (12). Ultrasound is a good tool to diagnose small solid breast lesions (12). Axillar lymph node ultrasound is necessary to make preoperative staging and make decision for neoadjuvant therapy (2, 12).
The majority of breast male cancers are invasive ductal carcinomas. More than 50% men with breast carcinoma are admitted to treatment with stage III or greater of disease (13). The majority of men suffered from male breast cancer have mastectomy with axillary lymph node dissection (10). Due to small breast size, subareolar location and advanced stage of neoplasm disease mastectomy is the most often operation in male breast cancer (10). Breast-conserving therapy (BCT) composed with breast-conserving surgery and radiation therapy is well established in female breast cancer, but its role in male breast cancer is still unclear (14).
Adjuvant hormonal therapy plays important role in treatment male breast cancer because most of patients have estrogen and progesterone receptor positive (15, 16). The antiestrogen agent tamoxifen should be used in therapy for 5 years, and this information is based on date from studies of female breast cancer. In men, prior treatment involved orchidectomy and adrenalectomy which should be made surgical methods or medically by using aminoglutethimide (16).
There are no large randomized chemotherapy trials in male breast cancer. But it should be used to treat in metastatic male breast cancer (17). Postmastectomy radiation therapy reduces risk of local recurrence male breast cancer. The National Comprehensive Cancer Network guidelines recommend use postmastectomy radiation therapy for women with 4 or more positive lymph nodes and consideration of such in patients with 1-3 positive lymph nodes (4). The same criteria should be used in male breast cancer, but some institutions recommend radiation therapy for tumor sizes greater than 1 cm or for more than 1 metastatically lymph node in male breast cancer (18, 19). Such treatment should decrease recurrence rates in chest wall and axillar lymph nodes, however the influence on survival is unknown. Decision regarding postmastectomy radiation therapy should be taken after assessment of the general condition of the patient and his consent to such treatment.
Male breast cancer patients should be carefully monitored for the occurrence of second cancer (melanoma, prostate cancer and a second primary breast cancer) (20).
CONCLUSIONS
1. Male breast cancer is a rare disease.
2. Male breast cancer has been associated with worse prognosis than female breast cancer.
3. Pain, breast mass and nipple changes are the most common symptoms of male breast cancer.
4. Ultrasound and mammography are good tools to diagnose small solid breast lesions.
5. Stage and treatment of male breast cancer is based on the same principles that guide the treatment of female breast cancer.
Piśmiennictwo
1. Jemal A, Siegel R, Ward E et al.: Cancer statistics, 2008. CA Cancer J Clin 2008; 58: 71-96. 2. National Cancer Institute. Surveillance Epidemiology and End Results (SEER): Cancer Statistics. Bethesda (MD): National Cancer Institute 2011. http://seer.cancer.gov/statistics/. 3. Ravandi-Kashani F, Hayes TG: Male breast cancer: a review of the literature. Eur J Cancer 1998; 34(9): 1341-1347. 4. National Comprehensive Cancer Network. NCCN Flash Update: NCCN Guidelines Updated. Fort Washington, PA: National Comprehensive Cancer Network 2011. http://www.nccn.org/about/news/ebulletin/2011-05-31/guidelines_compendium.asp. 5. Korde LA, Zujewski JA, Kamin L et al.: Multidisciplinary meeting on Male Brest cancer: summary and research recommendations. J Clin Oncol 2010; 28(12): 2114-2122. 6. Thorlacius S, Sigurdsson S, Bjarnadottir H et al.: Study of a single BRCA2 mutation with high carrier frequency in a small population. Am J Hum Genet 1997; 60(5): 1079-1084. 7. Brinon LA, Richesson DA, Gierach GL et al.: Prospective evaluation of risk factors for male breast cancer. J Natl Cancer Inst 2008; 100(20): 1447-1481. 8. Mabuchi K, Bross DS, Kessler II: Risk factors for male breast cancer. J Natl Cancer Inst 1985; 74(2): 371-375. 9. Gray J, Evans N, Taylor B et al.: State of the evidence: the connection between breast cencer and the environment. Int J Occup Environ Health 2009; 15(1): 43-78. 10. Kiluk JV, Lee MC, Park CK et al.: Male breast cancer: management and follow-up recommendations. Breast J 2011; 17(5): 503-509. 11. Giordano SH, Buzdar AU, Hortobagyi GN: Breast cancer in men. Ann Intern Med 2002; 137(8): 678-687. 12. Gomez-Raposo C, Zambrana Tevar F, Sereno Moyano M et al.: Male breast cancer. Cancer treat rev 2010; 36(6): 451-457. 13. Ottini L, Palli D, Rizzo S et al.: Male breast cancer. Crit Rev Oncol Hematol 2010; 73(2): 141-155. 14. Cutuli B, Le-Nir CC, Serin D et al.: Male breast cancer: evolution of treatment and prognostic factors: analysis of 489 cases. Crit rev Oncol Hematol 2010; 73(3): 246-254. 15. Ribeiro G, Swindell R: Adjuvant tamoxifen for male breast cancer (MBC). Br J Cancer 1992; 65(2): 252-254. 16. Ribeiro GG, Swindell R, Harris M et al.: A review of the management of the male breast carcinoma based on an analysis of 420 treated cases. Breast 1996; 5: 141-146. 17. Patel 2nd HZ, Buzdar AU, Hortobagyi GN: Role of adjuvant chemotherapy in male breast cancer. Cancer 1989; 64(8): 1583-1585. 18. Fentiman IS, Fourquet A, Hortobagyi GN: Male breast cancer. Lancet 2006; 367(9510): 595-604. 19. Gennari R, Curigliano G, Jereczek-Fossa BA et al.: Male breast cancer: a special therapeutic problem: anything new? Int J Oncol 2004; 24(3): 663-670. 20. Satram-Hoang S, Ziogas A, Anton-Culver H: Risk of second primary cancer in men with breast cancer. Breast Cancer Res 2007; 9: R10.