*Monika Jabłońska-Jesionowska, Lidia Zawadzka-Głos
295 children’s bronchoscopy due to choking episode with suspected foreign body in the of pediatric ent department – analysis of choking risk factors
Ocena czynników ryzyka krztuszenia na podstawie wyników 295 bronchoskopii wykonanych u dzieci z podejrzeniem ciała obcego dróg oddechowych
Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Associate Professor Lidia Zawadzka-Głos, MD, PhD
Streszczenie
Wstęp. Epizod zakrztuszenia ciałem obcym przez dzieci jest częstą przyczyną niewydolności oddechowej i wskazaniem do pilnej bronchoskopii. Zabieg ten jest bardzo trudny, stresujący i niebezpieczny u dzieci ze względu na małą średnicę dróg oddechowych oraz często towarzyszące objawy duszności. Skłonność do wkładania wszystkiego do ust w celach poznawczych, niepełne uzębienie, niedojrzały mechanizm połykania to czynniki ryzyka zadławienia u małych dzieci. Na przestrzeni lat wciąż toczą się dyskusje, jak ograniczyć liczbę wykonywanych bronchoskopii u dzieci.
Cel pracy. Autorzy niniejszej analizy starają się znaleźć odpowiedź na pytanie, czy i w jaki sposób można ograniczyć liczbę bronchoskopii dolnych dróg oddechowych u dzieci.
Materiał i metody. 295 dzieci poddano bronchoskopii w Klinice Otolaryngologii Dziecięcej Warszawskiego Uniwersytetu Medycznego w latach 2015-2020 po epizodzie zadławienia z podejrzeniem obecności ciała obcego dolnych dróg oddechowych. Zabieg wykonano po odpowiednim badaniu pediatrycznym i rtg klatki piersiowej. W analizie szczególną uwagę zwrócono na rodzaj ciał obcych oraz wyniki badań dodatkowych.
Wyniki. U 295 pacjentów wykonano sztywną bronchoskopię w znieczuleniu ogólnym. Wskazaniem do tego zabiegu był pojedynczy epizod zadławienia. U wszystkich dzieci stwierdzono patologię w badaniu pediatrycznym lub RTG klatki piersiowej. Tylko u 142 (48%) pacjentów znaleziono i usunięto ciało obce. Stwierdzono 110 (77,5%) organicznych i 32 (22,5%) nieorganiczne ciała obce. Spośród wszystkich 142 przypadków tylko 9 (6%) ciał obcych było widocznych na zdjęciu rentgenowskim. Najczęstszymi ciałami obcymi zidentyfikowanymi u 81% pacjentów były orzechy i nasiona. Najczęściej stwierdzono je u dzieci poniżej 3. roku życia. Mediana wieku tych dzieci wynosiła 2 lata.
Wnioski. W badaniu klinicznym po epizodzie zadławienia nie stwierdza się charakterystycznych objawów obecności ciała obcego w drogach oddechowych. Podejrzenie aspiracji jest nadal głównym wskazaniem do pilnej bronchoskopii u dzieci. Wydaje się, że tylko odpowiednia profilaktyka może zmniejszyć liczbę wykonywanych bronchoskopii. Szeroko prowadzona edukacja młodych rodziców powinna informować ich o ryzyku dławienia się dzieci. Szczególną uwagę należy zwrócić na fakt, aby nie podawać dzieciom małych, twardych pokarmów pochodzenia organicznego, zwłaszcza orzechów i ziaren. Należy również zwrócić uwagę rodziców na zabawki dla maluchów, które muszą być pozbawione małych, ruchomych części. Firmy produkujące żywność i zabawki dla dzieci powinny być zobowiązane do umieszczania na swoich produktach informacji o ryzyku zadławienia się u dzieci w pewnym wieku.
Summary
Introduction. Aspiration of foreign body by children is a common cause of respiratory failure and an indication for urgent bronchoscopy. This procedure under general anesthesia is very difficult, stressful and dangerous in children due to their small diameter of the respiratory tract with a symptom of dyspnea. The tendency to put everything in to the mouth for cognitive purposes, incomplete dentition, immature swallowing mechanism are all the factors of high risk of choking episodes in very young children. Over the years still has been discussions on how to limit the number of bronchoscopies performed in children.
Aim.The authors of this analysis try to find an answer to the question of whether and which way the number of bronchoscopy of the lower respiratory tract in children can be limited.
Material and methods. 295 children underwent a bronchoscopy in the Department of Pediatric Otolaryngology of the Medical University of Warsaw in 2015-2020 after an episode of choking with suspected foreign body of the lower respiratory tract. The procedure was done after an appropriate pediatric examination and X-ray of the chest. In the analysis, particular attention was paid to the type of foreign bodies, pathology in clinical examination and tests.
Results. 295 patients underwent rigid bronchoscopy under general anestesia. The indications for this procedure was single episode of choking. All children presented some patology in physical examination or on chest X-ray. Only in 142 (48%) patients a various foreign bodies were found and removed. That were 110 (77.5%) organic and 32 (22.5%) inorganic foreign bodies. Among all 142 cases only 9 (6%) were visible on X-ray. Peanuts and seeds were the most common foreign bodies, identified in 81% patients. The median age was 2 years.
Conclusions. There are not characteristic symptoms of foreign body in respiratory tract in clinical investigation after single episode of choking. The suspicion of aspiration is still the main indicates for urgent bronchoscopy in children. It seems that the number of performed bronchoscopies could be reduced by prevention. Extensive education for young parents should be providing to inform them about choking hazard. We should pay special attention to them not to give small hard organic food to their children; especially nuts and grains. Parents’ attention should also be paid to toys, which for toddlers must be free of small, moving parts. Also companies producing food and toys for children should be obliged to place information on the risk of chocking on their products.
Introduction
Bronchoscopy of the lower respiratory tract is a diagnostic and therapeutic method that allows for an accurate assessment of the respiratory tract with the possibility of collecting material for histopathological, microbiological examination or removal of pathologies from the respiratory tract. The world’s first bronchoscopy was performed in 1897 by the Viennese laryngologist Gustav Killian, who removed the bone from the bronchus. In the case of removing foreign bodies, it is a procedure performed under general anesthesia with the use of a rigid bronchoscopic tube with a diameter appropriate for the patient’s age. The bronchoscope is inserted through the mouth and larynx into the trachea and bronchi. At each stage of the procedure, a patient with an existing pathology in the lower respiratory tract may additionally develop respiratory disorders related to e.g. bronchospasm, bleeding or trauma to the airway wall, which will result in respiratory distress. That is why it is so important to carefully qualify the patient for bronchoscopy and avoid it in unnecessary situations. There have always been attempts to find the characteristic features of a foreign body retention in the lower respiratory tract, which are an absolute indication for bronchoscopy. Prophylaxis and procedures that can minimize the risk of choking with a foreign body are equally important.
Aim
The authors of this analysis try to find an answer to the question of whether and which way the number of bronchoscopy of the lower respiratory tract in children can be limited.
Material and methods
The retrospective analysis involved 295 children who were hospitalized in the Department of Pediatric Otolaryngology of the Medical University of Warsaw in 2015-2020 after an episode of choking with suspected foreign body of the lower respiratory tract. All these children underwent a bronchoscopy of the lower respiratory tract under general anesthesia with a STORZ rigid bronchoscope of an appropriate diameter depending on the age. The procedure was done after a precise pediatric examination and X-ray of the chest. In the analysis, particular attention was paid to the type of foreign bodies that were removed from the children’s lower respiratory tract and the abnormality found in the diagnostic tests.
Results
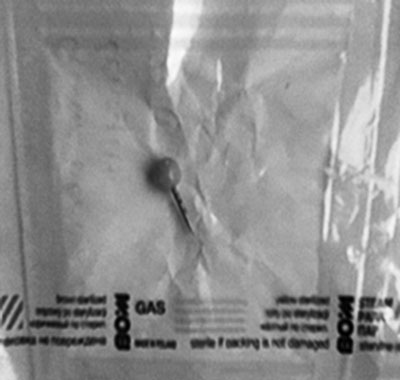
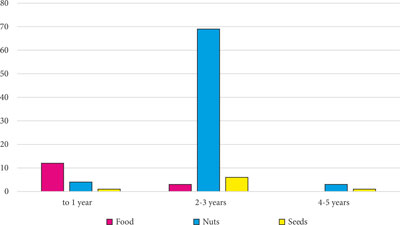
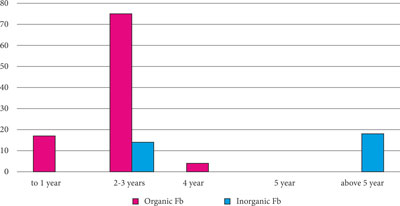
In the period of 6 years, 295 rigid bronchoscopies under general anesthesia were performed; in following years respectively: 2015 – 59; 2016 – 47; 2017 – 42; 2018 – 47; 2019 – 47; 2020 – 53. This were over 49 treatments each year, once a week on average. The analyzed group consisted of 295 children aged 6 months to 16 years; mean age 3 years, median 2 years. There were 159 boys and 136 girls among the children. All 295 (100%) children experienced an episode of choking. In 277 children, which is about 94% of cases, episode took place in the presence of another person and occurred during: eating, playing or physical activity of the child. Choking episodes occurred most often at homes or in the shops. There has been no case of choking in educational institutions such as a nursery, kindergarten. In older children, the episode happened as well at school. Usually it was an accidental choke that occurred when you deliberately held a piece of a writing instrument or a pushpin in your mouth. Older school-age children often hid the choking episode on a foreign body for fear of the consequences of this fact. Carefully collected medical history together with clinical symptoms allowed to determine the cause of the symptoms in this group of children. As part of the clinical investigation, all children had a pediatric examination with auscultation of the chest and an X-ray of the chest. Abnormalities in these tests or a history of choking was the reason for bronchoscopy. All 295 children underwent rigid bronchoscopy under general anesthesia, in which 142 patients (48%) had a foreign body in the airways, and no foreign body was found in 153 (52%) children. In 142 patients who had a foreign body removed, it was found: organic foreign bodies in 110 (77.5%) children and inorganic foreign bodies in 32 (22.5%). Among organic bodies, food fragments were found in 15 (13.5%) cases, nuts in 83 (75.5%) and other seeds, such as sunflower, pumpkin and corn in 12 (11%). The food rests were mainly pulp of groats, apples and cauliflower, which were sucked from the respiratory tract. In 2 cases, fragments of hard sausage were removed which was given to teething children to massage their sore gums. Among 32 inorganic foreign bodies, only 9 (28%) shading, i.e. visible on X-rays, were found: pin in 6 children, a small metal circle in 1, a small bulb also in 1 and part of ceramics in 1. In 23 children (72%) inorganic non-shading (not visible on X-ray) foreign bodies were found: plastic elements of toys removed in 9 children, plastic pen plugs in 11 and fragments of foil packaging in 3 children. Finally inorganic visible on X-ray foreign bodies accounted for only 6% of all foreign bodies removed. A detailed analysis of the age of patients who had a foreign body removed showed that in children under 1 year of age, food’s fragment was the dominant foreign body in 12 out of 17 cases, the rest 5 was nuts and seeds. Between the ages of 2-3 years, organic foreign bodies dominated in 75 out of 89 cases, and the most common of these was the peanuts, occurred in 72 children, which accounts for 81% of all foreign bodies in this age range. Among inorganic foreign bodies in 2-3-year-old children, small fragments of toys and foil packaging were removed in 14 cases. Only in 2 cases it was a shading (visible on X-rays) foreign body (bulb and metal circle). Organic foreign bodies were found only in the group of children aged 4-5 in 4 cases and it was also a nut or a grain. In older children from the age of 5, no organic foreign bodies were found in the respiratory tract. No inorganic foreign bodies were found in 4-year-olds. In children from 5 to 16 years of age, 18 inorganic foreign bodies were found in the respiratory tract, including 11 plastic fragments of writing instruments, 1 fragment of ceramics and 6 metal pins or thumbtacks. The last visible on the X-ray as a linear brightening in the airways often turned out to be much larger due to the plastic ending as shown in the figure 1. Such thumbtacks found in 4 children were difficult to remove due to their size; the plastic part obstructs the bronchi and the metal one sticks and hurts to the wall of the airways. In this group of children, choking was usually a random aspiration of an element held in the mouth. In most cases, these patients reported a choking episode. In 1 patient aged 14, a fragment of a ceramic cup was found, which had been aspirated during an attempted self-mutilation. The foreign body was visualized on the X-ray. The patient presented with hemoptysis and dyspnea. The figures no 2 and 3 shows the graphical analysis of the types of foreign bodies in each age groups. The youngest patient, who underwent bronchoscopy and foreign body removal, was 6 months old and the oldest was 16 years old; in turn, the youngest patient who did not have a foreign body was also 6 months old, but the oldest was 7 years old. In 153 children with a choking episode, in whom no foreign body during bronchoscopy, but: mucopurulent discharge 54 (35%), mucosa congestion with ecchymosis 38 (25%), granulation tissue in 2 (1.5%) children; and in 59 (38.5%) cases no pathology was found. When analyzing results of a pediatric examination after an episode of choking, there were no children without auscultatory changes. In the group 142 of children who had a foreign body removed wheezing was found in 82 (59%) children, respiratory noise asymmetry in 67 (47%), whirring in 27 (19%) and tachypnea in 14 (10%). The same changes occurred in 153 children, who had no foreign body found in the airways with the following frequency: in 44 (29%) wheezing, in 53 (35%) respiratory asymetry, whirring in 43 (28%), and tachypnea in 25 (16%) children. After taking an X-ray of the chest in children with a foreign body in the respiratory tract, it was found: shading foreign body in 9 children (6%), atelectasis in 23 (16%), mediastinal displacement in 10 (7%) and features of an air-trapping in 36 (26%) children, in 64 (45%) of cases the X-ray was unchanged. Similarly, chest X-ray in children with no foreign body detected showed features of an air-trapping in 85% (130 children) and no changes in the remaining 15% of cases (23 children).
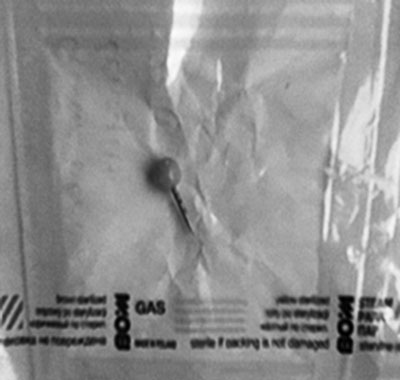
Fig. 1. Thumbtacks removed from bronchi
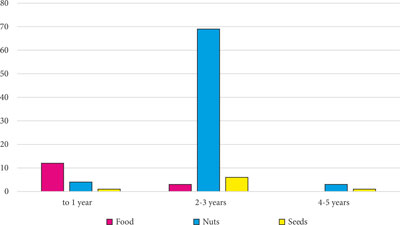
Fig. 2. Analysis of the type of foreign body (FB) according to the age
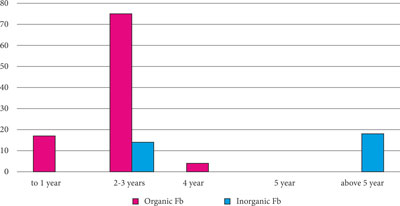
Fig. 3. Type of organic foreign bodies according to the group of age
Discussion
Another analysis of patients suspected of having a foreign body in the airways classified for bronchoscopy under general anesthesia shows that both: the history indicating the episode of aspiration and additional tests do not give the correct answer, which is a sign of the presence of foreign bodies in the respiratory tract and the indication for urgent bronchoscopy. All 295 children experienced an episode of choking. A foreign body in the respiratory tract was found in 142 children (48%). A cough with expectoration of secretions that occurred, for example, during a meal time, was interpreted as an episode of choking. In some of the children there was a thick mucopurulent discharge which was the features of the infection. Out of 142 removed foreign bodies only 9 (6%) were visible on the X-ray, which is the absolute sign of a foreign body. Thus the result of radiological diagnosis can’t be the only indication for bronchoscopy lower airways. Changes on chest X-ray in the nature of mediastinal displacement, atelectasis, emphysema or air-trapping occurred even more often in children with infection, where the pathology of the airway resulted from obstruction with secretions or edema. It is undeniable that organic foreign bodies, including peanuts and seeds, are dominant in the group of children under 3 years of age (1-7). While the choking is accidental, the administration of this type of food for children is the aware action of the caregivers. The healthy content of nutrients and minerals in grains and nuts are obvious, but this kind of food in the mouth of a young child with incomplete dentition might be very dangerous, as our analysis shows. The diameter of peanuts or other seeds is comparable to the diameter of a child’s lower respiratory tract, which ranges from 5 mm in a newborn to 6.5 mm at around 3 years of age and can completely obstruct the airways. The compact and hard consistency of grains and nuts is also dangerous, and the fact that they do not dissolve quickly under the influence of food enzymes. It needs to be remembered, that nut’s allergy, which may not yet be diagnosed in young child, may cause swelling of the respiratory mucosa, which aggravates the symptoms of dyspnea. After analyzing the cases of 295 children who underwent bronchoscopy after an single episode of choking, it seems that the procedure could be avoided by appropriate management in about 31% of cases. These are children, who were given seeds, nuts (77 children) or small pieces of toys (14 children) up to 3 years of age. It is difficult to deprive children of toys, although you can be careful when choosing their size. It is noteworthy that among our patients no any episode of choking occurred in educational facilities such as nursery or kindergarten. The above analysis also shows that nuts and seeds should not be given to children under 3 years of age. Small, hard pieces of food in children with incomplete teeth and a lack of coordinated chewing movements are a dangerous part of eating. The hard nut can be replaced with e.g. peanut butter. Such an educational tip should be among the many others a young parent receives. It seems that the number of performed bronchoscopies could be reduced by prevention. The information about choking hazard needs to be delivered to the caregivers. The special attention is needed to not give small hard organic food to their children, especially nuts and grains. Parents’ attention should also be paid to toys, which for toddlers must be free of small, moving parts. We conduct numerous clinical analysis and have a large quantity of information on foreign body aspiration in children; what is the most common choking behavior in children and at what age (3, 8-11). This information should be communicated to parents and primary care physicians. This would be aimed at increasing caregivers’ attention to appropriate conduct and create of safe environment for children. As the studies of other authors show the viewer on this subject in young people is insufficient and the introduction of appropriate education increases their awareness (12-21). We should also be alert to food companies that they put information on their products about the choking risk of a young child (3, 7, 8). Relevant guidelines must also include instructions on toys sold to children. Also companies producing food and toys for children should be obliged to place information on the risk of chocking on their products (7). In the group of older children, as in adults, there will always be random aspirations of a foreign body. The fact of reporting such an episode allows to avoid unnecessary conservative treatment and delaying bronchoscopy, and to avoid long-term complications resulting from the long-term presence of a foreign body with the development of inflammatory changes, during which the procedure is associated with an increased risk of respiratory failure.
Conclusions
In the case of foreign bodies of the respiratory tract, no characteristic symptoms were found in the clinical examination and diagnostic tests that confirm or exclude a foreign body, what allowed to avoid a difficult and often dangerous procedure such as bronchoscopy. Even a single choking episode is not always associated with foreign body aspiration. In order to avoid unnecessary bronchoscopy in an urgent procedure, appropriate behaviors minimize choking hazard should take place (2). Peanut is the most common foreign body in the group of children from 2-3 years of age, which accounts for 81% of all foreign bodies at this age and as much as 96% of organic foreign bodies in this age group (2, 4, 5). Caregivers educational campaign from early childhood should contain information on the need to avoid whole nuts and seeds in the diet of children under 3 years of age. Following the example of educational and care facilities, it is necessary to select safe toys without small, moving fragments, appropriate to the child’s age and to control the course of play (3).
Piśmiennictwo
1. Mahmud A, Mohammed Y, Akeem A, Aluko A: Knowledge of foreign-body aspiration in children among caregivers in Kano Nigeria. African Journal of Trauma 2017; 6(2): 42-46.
2. Iversen RH, Klug TE: Need for more clear parental recommendations regarding foreign body aspiration in children. Dan Med J Sep 2012; 59(9): A 4498.
3. Foltran F, Ballali S, Rodriguez H et al.: Inhaled foreign bodies in children: a global perspective on their epidemiological, clinical, and preventive aspects. Pediatr Pulmonol 2013; 48 (4): 344-351.
4. Pan H, Lu Y, Shi L et al.: Similarities and differences in aspirated tracheobronchial foreign bodies in patients under the age of 3 years. Int J Ped Otorhinolaryngol 2012; 76(6): 911-914.
5. Cohen S, Goldberg S, Springer C et al.: Foreign body aspiration in children. Harefuah 2015; 154(3): 175-177, 211.
6. Chand R, Shaikh M, Khan Y et al.: Frequency of Various Foreign Bodies Retrieved from the Airway During Bronchoscopy in Children: A Pediatric Tertiary Care Center Experience. Cureus 2020; 12(7): e9348.
7. Sidell DR, Kim IA, Coker TR et al.: Food choking hazards in children. Int J Pediatr Otorhinolaryngol 2013; 77(12): 1940-1946.
8. Hochdorn A, Oliveira A, Lorenzoni G et al.: Monitoring Public Perception of Health Risks in Brazil and Italy: Cross-Cultural Research on the Risk Perception of Choking in Children. Children (Basel) 2021; 8(7): 541.
9. Lorenzoni G, Azzolina D, Baldas S et al.: Increasing awareness of food-choking and nutrition in children through education of caregivers: the CHOP community intervention trial study protocol. Observational Study BMC Public Health 2019; 19(1): 1156.
10. Lorenzoni G, Lanera C, Azzolina D et al.: Assessing school-based intervention strategies to foster the prevention of choking injuries in children: The results of the CHOP (CHOking Prevention) trial Health Soc Care Community 2021.
11. Cutrone C, Pedruzzi B, Tava G et al.: The complimentary role of diagnostic and therapeutic endoscopy in foreign body aspiration in children. Int J Ped Otorhinolaryngol 2011; 75(12): 1481-1485.
12. Higuchi O, Adachi Y, Adachi YS et al.: Mothers’ knowledge about foreign body aspiration in young children. International Journal of Ped Otorhinolaryngology 2013; 77(1): 41-44.
13. Sahin A, Meteroglu F, Eren S, Celik Y: Inhalation of foreign bodies in children: experience of 22 years. J Trauma Acute Care Surg 2013; 74(2): 658-663.
14. Nichols BG, Visotcky A, Aberger M et al.: Pediatric exposure to choking hazards is associated with parental knowledge of choking hazards. Int J Pediatr Otorhinolaryngol 2012; 76: 169-173.
15. Slapak I, Passali FM, Gulati A, Group SSW: Non food foreign body injuries. Int J Ped Otorhinolaryngol 2012; 76: 26-32.
16. Sih T, Bunnag C, Ballali S et al.: Nuts and seed: a natural yet dangerous foreign body. Int J Ped Otorhinolaryngol 2012; 76 Suppl. 1: 49-52.
17. Gregori D, Salerni L, Scarinzi C et al.: Foreign bodies in the upper airways causing complications and requiring hospitalization in children aged 0-14 years: results from the ESFBI study. ESFBI Study Group. Eur Arch Otorhinolaryngol 2008; 265(8): 971-978.
18. Montana A, Salerno M, Feola A et al.: Risk management and recommendations for the prevention of fatal foreign body aspiration: four cases aged 1.5 to 3 years and mini-review of the literature. Int J Environ Res Public Health 2020; 17(13): 4700.
19. Thamboo A, Nguyen T, Ludemann JP: Choking prevention: shortcomings of traditional public education campaigns, prompting the development of web-based interactive teaching tools for preteens, teenagers, and adults. J Otolaryngol Head Neck Surg 2009; 38(6): 646-651.
20. Bentivegna KC, Borrup KT, Clough ME, Schoem SR: Basic choking education to improve parental knowledge. Int J Ped Otorhinolaryngol 2018; 113: 234-239.
21. Karatzanis AD, Vardouniotis A, Moschandreas J et al.: The risk of foreign body aspiration in children can be reduced with proper education of the general population. Int J Ped Otorhinolaryngol 2007; 71(2): 311-315.