*Monika Jabłońska-Jesionowska, Lidia Zawadzka-Głos
Children’s head and neck infections caused by Streptococcus intermedius in the Pediatric Otolaryngology Department of Warsaw Medical University
Infekcje górnych dróg oddechowych u dzieci o etiologii Streptococcus intermedius w Klinice Otolaryngologii Dziecięcej Warszawskiego Uniwersytetu Medycznego
Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Lidia Zawadzka-Głos, MD, PhD
Streszczenie
Wstęp. Paciorkowce są powszechnie znanymi patogenami prawidłowej flory bakteryjnej jamy ustnej, gardła, przewodu pokarmowego i układu moczowo-płciowego. Najczęściej spotykane, łatwe do rozpoznania i leczenia są infekcje spowodowane paciorkowcami beta-hemolizującymi, które wywołują zapalenia gardła, anginy paciorkowcowe, zapalenia uszu i zatok przynosowych. Jednak nie wszystkie infekcje paciorkowcowe są łatwe do wyleczenia. Są takie paciorkowce, które tworzą ropnie w głębokich tkankach organizmu powodując zagrażające życiu powikłania.
Cel pracy. Celem pracy jest zwrócenie uwagi na patogen z grupy Streptococcus viridans, czyli Streptococcus intermedius, który będąc saprofitem górnych dróg oddechowych może powodować zagrażające życiu powikłania w przebiegu zakażenia.
Materiał i metody. Przeprowadzono retrospektywną analizę danych dzieci leczonych w Klinice Otolaryngologii Dziecięcej WUM z powodu zakażenia Streptococcus intermedius. U tych dzieci analizowano wiek, płeć, chorobę podstawową, powikłania oraz leczenie zachowawcze i operacyjne.
Wyniki. W Klinice Otolaryngologii Dziecięcej WUM z powodu infekcji wywołanej przez Streptococcus intermedius leczono 6 dzieci w wieku od 14 miesięcy do 15 lat. Było to 5 chłopców i 1 dziewczynka. U wszystkich dzieci w przebiegu infekcji stwierdzono ropnie w tkankach głębokich głowy i szyi jako powikłania: ostrego zapalenia zatok u 4 dzieci, zapalenia gardła u 1 i po urazie kości nosa u 1 dziecka. U żadnego dziecka nie stwierdzono przewlekłych zaburzeń odporności. Leczeniem z wyboru była antybiotykoterapia i chirurgiczny drenaż ropni. Wszystkie dzieci zostały skutecznie wyleczone.
Wnioski. Izolacja Streptococcus intermedius z posiewów pobranych z miejsca zakażenia w obrębie górnych dróg oddechowych wiąże się z ryzykiem powikłań pod postacią głębokich ropni głowy, szyi oraz ośrodkowego układu nerwowego. Każdy pacjent z zakażeniem o etiologii Streptococcus intermedius wymaga obrazowania CT lub MRI twarzoczaszki i mózgu ze względu na możliwość wystąpienia głębokich ropni. Leczeniem z wyboru jest antybiotykoterapia ceftriaksonem, klindamycyną oraz drenaż chirurgiczny ropnia. Wrażliwość Streptococcus intermedius na popularne antybiotyki jest powodem skutecznego leczenia pomimo poważnych, zagrażających życiu powikłań.
Summary
Introduction. Streptococci are commonly known pathogens of the normal bacterial flora of the mouth, pharynx, gastrointestinal tract and genitourinary system. The most common infections are beta-hemolyzing streptococci causing pharyngitis, streptococcal angina, otitis and paranasal sinusitis. But not all streptococcal infections are easy to treat. They are those that forming abscesses in the deep tissues of the body and caused life-treating complications.
Aim. The aim of the study is to draw attention to the pathogen of the Streptococcus viridans group, i.e. Streptococcus intermedius, which, being a saprophyte of the upper respiratory tract, may cause life-threatening complications during an infection.
Material and methods. The age, sex of children, underlying disease, complications, conservative and surgical treatment of children treated in the Pediatric Otolaryngology Department of the Medical University of Warsaw due Streptococcus intermedius infections were analyzed.
Results. 6 children in age from 14 months to 15 years were treated in the ENT Department of Warsaw Medical University due to Streptococcus intermedius infections. There were 5 boys and 1 girl. All children were diagnosed with abscesses in deep tissue as a complication of acute sinusitis in 4 children, pharyngitis in 1 and post trauma nasal bone in 1 child. All children were immunocompetent. The treatment of choice was antibiotic therapy and drainage of abscesses. All children were successfully treated.
Conclusions. The isolation of Streptococcus intermedius in cultures taken from infection’s site in the upper respiratory tract is associated with the risk of complications in the form of deep head and neck and central nervous system abscesses. Each patient with an infection of Streptococcus intermedius etiology requires CT or MRI imaging of the craniofacial and brain due to the possibility of deep abscesses. The treatment of choice is antibiotic therapy with ceftriaxone, clindamycin and together with surgical drainage of the abscess. The sensitivity of Streptococcus intermedius to popular antibiotics is the reason for effective treatment despite serious complications.
Introduction
Streptococci are commonly known pathogens. They are normal bacterial flora of the mouth, throat, gastrointestinal tract and genitourinary system in children and adults (1-3). They are often activated when immunity decreases. The most common infections are beta-hemolytic streptococci which cause pharyngitis, streptococcal angina, otitis and paranasal sinusitis. Each ENT specialist in his practice successfully treated a patient with a streptococcal infection, quickly and without complications. Patient’s medical histories and clinical observations show that not all streptococcal infections are easy to treat. They are those that cause severe, life-treating complications in the deep tissues of the head, including the central nervous system, neck, thorax and abdominal cavity, that are difficult to treat.
Streptococci are Gram-positive bacteria. They are aerobic and facultative anaerobic bacteria. Those bacteria have hemolytic properties. Depending on the type of hemolysis, they are divided into 2 groups: alpha-hemolyzing, where there is a reduction of iron in hemoglobin, which causes a green color on the blood agar plate, which is why they are also called Streptococcus viridans, and beta-hemolyzing, where erythrocytes are completely decomposed.
Beta-hemolyzing streptococci are divided into about 20 groups, from A to O, depending on the presence of polysaccharide molecules in the cell wall of the pathogen (Lancefield antigen). Among the beta-hemolyzing agents the most known are: Streptococcus pyogenes (group A) responsible for the development of streptococcal angina, pharyngitis, erysipelas, scarlet fever and Streptococcus agalactiae (group B) responsible for the perinatal infection of newborns leading to the development of dangerous sepsis (4).
Alpha-hemolyzing streptococci are also known as Streptococcus viridans, Streptococcus anginosus group or formerly Streptococcus milleri after name the microbiologist W D Miller. It was first described by Guthof in 1956 after isolating them from a dental abscess. They include: Streptococcus intermedius, Streptococcus anginosus and Streptococcus constellatus (5). These organisms are a constant component of the normal human bacterial flora of the mouth, throat, gastrointestinal tract and genitourinary system. Their characteristic feature is the ability to form abscesses and the development of systemic infections. They produce hyaluronidases, which facilitate the penetration of pathogens into the deep tissues, which is responsible for their high pathogenic invasiveness.
Particular Streptococci anginosus pathogens also differ from each other, among them Streptococcus intermedius stands out. It produces enzymes hyaluronidase and neuraminidase, which can increase spread of the infection especially through a bony wall and also secretes specific human cytolysin responsible for abscess formation. Streptococcus constellatus produces only hyaluronidase and Streptococcus anginosus does not produce any (6-8).
Infections due to group of the Streptococcus anginosus are often polymicrobial and may be accompanied by e.g. Eikenella corrodens or Fusobacterium nucleatum (9, 10).
Treatment is antibiotic therapy with a beta-lactam antibiotic. The drug of choice is ceftriaxone. In case of allergy to beta-lactam antibiotics vancomycin is the choice. All Streptococcus anginosus are macrolide resistant. Due to the contamitant anaerobic infection, metronidazole or clindamycin should be added. Treatment should be carried out depending on the resolution of clinical and/or radiological symptoms, usually 4-6 weeks is sufficient. In the presence of abscess, surgical drainage is essential (9-11). In isolation of a pathogens from the Streptococcus anginosus group, especially Streptococcus intermedius, special consideration should be given to the possibility of distant abscesses in the deep tissues of the head, neck, central nervous system, as well as lung and liver abscesses or complicated intra-abdominal infections (12-17).
Aim
The aim of the study is to draw attention to the pathogen of the Streptococcus viridans group, i.e. Streptococcus intermedius, which, being a saprophyte of the upper respiratory tract, may cause life-threatening complications during an infection.
Material and methods
The medical history of children treated in the Pediatric Otolaryngology Department of the Medical University of Warsaw due Streptococcus intermedius infections was analyzed. The age, sex of children, underlying disease, complications, conservative and surgical treatment, and long-term effects were analyzed retrospectively.
Results
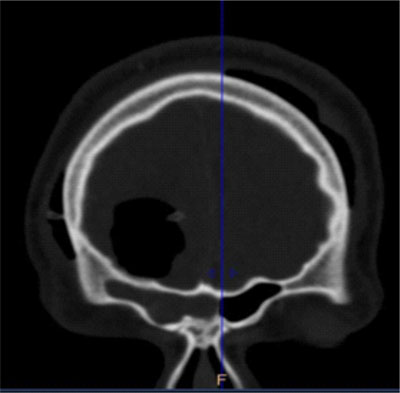
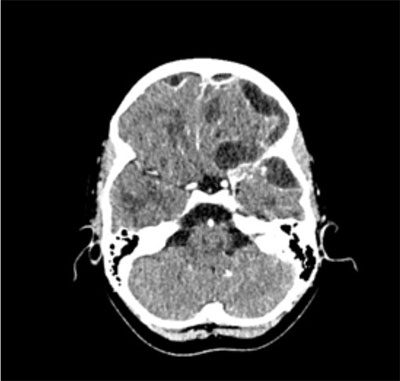
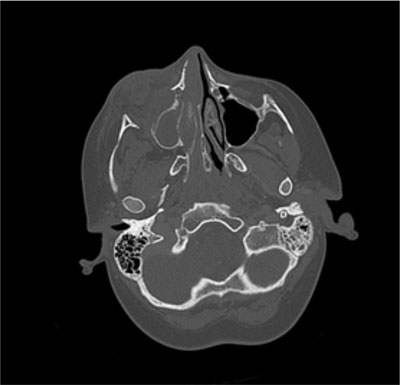
In the last 4 years, 6 children were treated in the Pediatric Otolaryngology Department due to Streptococcus intermedius infections. The children ranged in age from 14 months to 15 years of age; the median age was 10 years. There were 5 boys and 1 girl in the group. Acute paranasal sinusitis was diagnosed in 4 children, post traumatic abscess of the lateral nasal wall in 1 and peritonsillar abscess in 1 child. Acute paranasal sinusitis in one child was odontogenic. All children were immunocompetent, with no immunodeficiency; one 14-year-old boy has been treated for bronchial asthma since the age of 3. One child developed acute sinusitis during infection with influenza B and two children during SARS-CoV-2 infection. In all children severe complications was observed: abscess of the frontal sinus in 3 children together with Pott’s puffy tumor in 2 (fig. 1), multiple abscesses of the brain in 2 children (fig. 2), thrombosis of the intracranial sinuses in 2 children, intraorbital abscess in one child (fig. 3), peritonsillar abscess in one and osteomyelitis also in one (fig. 4). The table 1 presents the basic analyzed patient’s data.
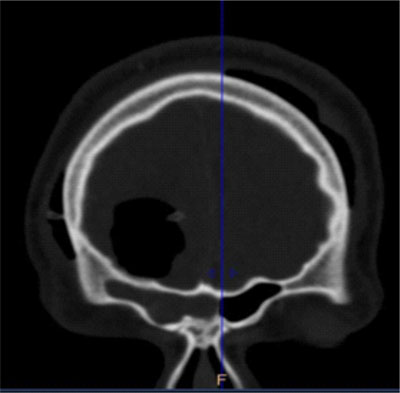
Fig. 1. Extra and intracranial complications of the right frontal sinusitis
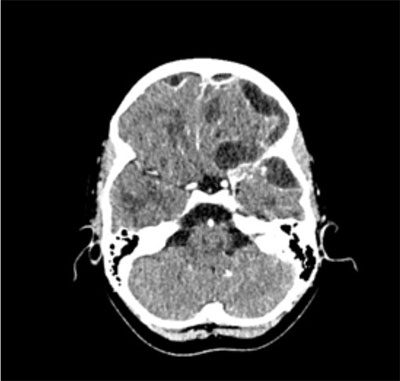
Fig. 2. Multiple abscesses of the brain
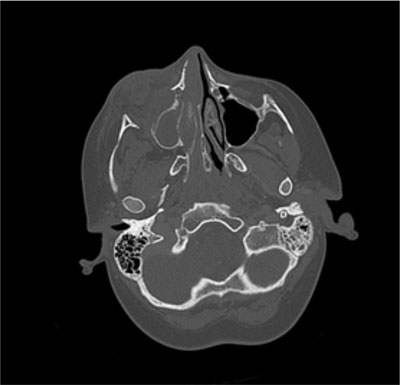
Fig. 3. Intraorbital abscess

Fig. 4. Osteomyelitis of the maxillae
Tab. 1. Data of patients with Streptococcus intermedius infection
| Age | Sex | Diagnosis | Complications | Blood tests | Conservative treatment | Surgery | Culture of abscess cavities | Treatment time |
HP
15 years | M | Acute sinusitis
SARS-CoV-2 | Abscess of the left frontal sinus with Pott’s puffy tumor
Multiple abscesses of the brain
Thrombosis of the transverse sigmoid sinus
Lower limb thrombosis | WBC 20 (N 4-10)
CRP 1.4 (N 0-1)
D-dimers 28000 (N 0-550)
PCT 0.4 | Ceftriaxon
Klindamycin
Vankomycin
Metronidazol
Heparin | Left frontal sinus Beck’s puncture
Multi-hole trepanation, drainage of numerous CNS abscesses | SI | 8 weeks with antibiotic
6 weeks antithrombotic treatment |
OL
10 years | F | Acute sinusitis
Influenza B | Abscess of the right frontal sinus
Multiple abscesses above and subdural brain
Bacterial meningitis
Thrombosis of the upper sagittal sinus | WBC N
CRP 25 (N 0-1)
D-dimers 4000 (0-550) | Ceftriaxon
Klindamycin
Vankomycin
Metronidazol
Heparin
Meronem
Penicillin | Bilateral right frontal sinus Beck’s puncture
Puncture of both maxillary sinuses
FESS
Left fronto-spheno-temporal craniotomy, drainage of numerous abscesses | SI | 8 weeks with antibiotic
4 weeks antithrombotic treatment |
OL
15 years | M | Acute sinusitis
SARS-CoV-2 | Abscess of the left frontal sinus with Pott’s puffy tumor | WBC N
CRP 2 (N 0-1) | Ceftriaxon
Klindamycin | Left maxillary sinus puncture;
Left frontal sinus Beck’s, puncture | SI | 4 weeks |
JP
14 years | M | Dental caries
Acute sinusitis | Abscess of the right maxillary sinus
Right orbital abscess | WBC 15
CRP 20 (N 0-1) | Ceftriaxon
Klindamycina | Extraction of 17 teeth
Puncture of the maxillary sinus
Drainage of an orbital abscess | SI | 3 weeks |
TK
4 years | M | Post traumatic abscess of the nasal lateral wall | Osteomyelitis of maxillae and nasal bones | WBC N
CRP N | Ceftriaxon
Klindamycin
Metronidazol | Nasal lateral wall abscess drainage x 3 | Eikenella corrodens SI | 3 weeks
3 weeks |
MS
14 months | M | Pharyngitis | Peritonsillar abscess | WBC N
CRP 1.2
(N 0-1) | Klindamycin, Amoxycilin + Clavulonic acid | Drainage of the peritonsillar abscess | SI | 3 weeks |
In the treatment of all children apart from antibiotic therapy, surgery was required. Apart from opening the primary site of infection, which were maxillary and frontal sinuses, peritonsillar abscess, or an abscess of the lateral wall of the nose, 2 children required trepanation of the skull to drainage multiple brain abscesses, and 1 required orbital abscess drainage. A 14-year-old boy required extraction of 17 teeth, which were his primary source of infection.
In all children Streptococcus intermedius was cultured from the above-mentioned abscesses in maxillary sinus, frontal sinus, peritonsillar abscess, lateral nasal wall abscess and brain abscesses. Some children was taken blood for bacterial culture because of a very high temperature and it was negative.
Antibiotic susceptibility was determined in each case; all bacterial colonies were sensitive to: clindamycin, penicillin, cephalosporin, vancomycin. In a child with an abscess of the lateral nasal wall anaerobic bacteria were also grown and it was Eikenella corrodens sensitive to: penicillin, fluoroquinolone, meropenem, cefotaxime. In all children conservative treatment was carried out according to the antibiogram and lasted from 4 to 8 weeks in the cases of brain abscesses. In each case ceftriaxone and clindamycin were used, with the exception of the child with peritonsillar abscess as a complication of pharyngitis where the patient received amoxicillin with clavulanic acid and clindamycin. Patients with brain abscesses in long-term therapy also received vancomycin and metronidazole, and heparin due to thrombosis in the brain sinuses. A patient with primary traumatic nasal lateral abscess complicated by osteitis of the maxillary frontal process, in whom Eikenella corrodens was isolated in addition to Streptococcus intermedius, was also treated with ceftriaxone, clindamycin and metronidazole.
All patients were cured. A 10-year-old girl and 15-year-old boy with multiple brain abscesses, sinus thrombosis and meningitis does not present permanent neurologic deficits. A 14-year-old boy with an odontogenic abscess of the maxillary sinus and an orbital abscess was deprived of 17 permanent carious teeth, the lack of which will require dentures.
Discussion
The Streptococcus anginosus group (SAG, S. anginosus, S. intermedius and S. constellatus) are part of the normal bacterial flora of the oral cavity, gastrointestinal tract and genitourinary system (1-3). The presence of pathogens from this group, especially Streptococcus intermedius, is often associated with the severe course of the disease due to the ability to form abscesses in deep tissues. Head and neck abscesses are the most common complications of sinusitis, ear infections, odontogenic infections and post-traumatic lesions (6-8, 12-17). In the material of our clinic, infection with Streptococcus intermedius etiology was complications of acute sinusitis in 4 cases (68%), in 1 of dental carries (16%), and in 1 child (16%) it was the result of a facial trauma of the maxilla and nose bone area. We did not have a patient with otitis due to Streptococcus anginosus. In our patients, we isolated Streptococcus intermedius from an orbital abscess that was a complication of odontogenic maxillary sinusitis, from intracranial abscesses that were a complications of frontal sinusitis with Pott’s puffy tumor, and from an abscess of the lateral nasal wall resulting post-traumatic osteomyelitis of the maxilla and nasal bones.
Data from the literature show that in the course of Streptococcus intermedius infections, severe complications in the form of deep and intracranial abscesses may arise in completely healthy children, which may additionally cause the diagnosis more difficult (13). In our material, we observed intraorbital and intracranial complications in previously healthy children without chronic immune disorders. In 3 cases, they occurred in children in the course of viral infection with influenza type B and SARS-CoV-2 infection. Viral infections can cause a decrease in the body’s resistance to immune disorders.
No bacteria were found in blood collected for culture in all children with abscesses in deep tissues. Streptococcus intermedius was grown from the purulent material evacuated from the abscess (12). The cause of intracranial abscesses is the direct transmission of infection from the adjacent craniofacial tissues through the bone wall, probably due to the action of enzymes secreted by the pathogen. Streptococci beta-hemolyzing group causing streptococcal angina, scarlet fever and other widespread infections are well known, with no doubts about treatment. Streptococci beta-hemolyzing group B, responsible for perinatal infections in newborns, also has adequate standards of treatment. The data from the literature, and also our observation shows that Streptococcus intermedius is sensitive to popular, widely used antibiotics such as penicillin, ceftriaxone, clindamycin and metronidazole (6, 9, 10). Infections due to Streptococcus intermedius even with serious complications such as brain abscess treated with above-mentioned antibiotic therapy and surgery lead to eradication of the pathogen. All our children were healed and those with drained brain abscesses show no neurological deficits. Alpha-hemolytic streptococci cause infections with life-threatening complications, therefore the identification of bacteria from this group in biological material should raise our particular vigilance regarding the course of infection. It seems that the alfa-hemolyzing Streptococci, so-called Streptococci anginosus or viridans are isolated perhaps too rarely from biological material. Also, the literature indicates that bacteria from this group are often considered only as contaminants in cultures. We as pediatricians, ENT surgeons should pay particular attention to the presence of Streptococcus anginosus in biological materials. Clinical microbiologists should use existing laboratory tests to isolate Streptococcus intermedius from group of Streptococcus anginosus due to the severe deep tissue complications it can cause (14).
1. The isolation of Streptococcus intermedius in cultures taken from infection’s site in the upper respiratory tract is associated with the risk of complications in the form of deep head and neck abscesses and central nervous system abscesses.
2. The isolation of bacteria from the Streptococcus anginosus group should lead to the determination of Streptococcus intermedius in this group due to the risk of life-threatening complications.
3. Each patient with an infection of Streptococcus intermedius etiology requires CT or MRI imaging of the craniofacial and brain due to the possibility of deep abscesses.
4. The treatment of choice is antibiotic therapy with ceftriaxone, clindamycin and together with surgical drainage of the abscess.
5. The sensitivity of Streptococcus intermedius to popular antibiotics is the reason for effective treatment despite serious complications.
1. Whiley RA, Beighton D, Winstanley TG et al.: Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus (the Streptococcus milleri group): association with different body sites and clinical infections. J Clin Microbiol 1992; 30(1): 243-244.
2. Issa E, Salloum T, Tokajian S: From normal flora to brain abscesses: A review of Streptococcus intermedius. Front Microbiol 2020; 7(11): 826.
3. Almatrafi MA, Almuflihi A, Jarwann R et al.: Viridans group streptococcus meningitis in an immunocompetent child: A case report. Am J Case Rep 2021; 14(22).
4. Mishra AK, Fournier P.: The The role of Streptococcus intermedius in brain abscess. European J of Clinical to Microbiology and Inf Dis; 2013 Apr; 32 (4): 477-483.
5. Guthof O: Pathogenic strains of Streptococcus viridans; streptococci found in dental abscesses and infiltrates in the region of the oral cavity. Zentralbl Bakteriol Orig 1956; 166: 553-564.
6. Yeşilbaş O, Tahao?lu I, Yozgat CY et al.: Subdural empyema, brain abscess, and superior sagittal sinus venous thrombosis secondary to Streptococcus anginosus. Turk Arch Pediatr 2021; 56(1): 88-91.
7. Faden HS: Infections associated with Streptococcus intermedius in children. Pediatr Infect Dis J 2016; 35: 1047.
8. McNeil JC, Dunn JJ, Kaplan SL et al.: Complications of Otitis Media and Sinusitis Caused by Streptococcus anginosus group organisms in children. Pediatr Infect Dis J 2020; 39(2): 108-113.
9. Furuichi M, Horikoshi Y: Sites of infection associated with Streptococcus anginosus group among children. J Infect Chemother 2018; 24(2): 99-102.
10. Kou YF, Killeen D, Whittemore B et al.: Intracranial complications of acute sinusitis in children: The role of endoscopic sinus surgery. Int J Pediatr Otorhinolaryngol 2018; 110: 147-151.
11. Deutschmann MW, Livingstone D, Cho JJ, et al.: The significance of Streptococcus anginosus group in intracranial complications of pediatric rhinosinusitis. JAMA Otolaryngol Head Neck Surg 2013 Feb; 139 (2):157-60.
12. Kragha KO: Multiple brain abscesses due to Streptococcus anginosus: Prediction of mortality by an imaging severity. Case Rep Radiol 2016; 2016: 7040352.
13. Petti CA, Simmon KE, Bender J et al.: Culture-negative intracerebral abscesses in children and adolescents from Streptococcus anginosus group infection: a case series. Clinical Infectious Diseases 2008; 46(10): 1578-1580.
14. McNeil J, Chase D, James JD et al.: Complications of otitis media and sinusitis caused by Streptococcus anginosus group organisms in children. Pediatr Infect Dis J 2020; 39(2): 108-113.
15. Chaudhry IA, Shamsi FA, Elzaridi E et al.: Outcome of treated orbital cellulitis in a tertiary eye care center in the middle East. Ophthalmology 2007; 114(2): 345-354.
16. Imholz B, Becker M, Lombardi T et al.: Septic thrombosis of the cavernous sinus secondary to a Streptococcus milleri oral infection. Dentomaxillofac Radiol 2012; 41: 525.
17. Watkins LM, Pasternack MS, Banks M et al.: Bilateral cavernous sinus thromboses and intraorbital abscesses secondary to Streptococcus milleri. Ophthalmology 2003; 110: 569-574.