Maria Rutowicz1, Maria Wolniewicz2, Paula Piórkowska1, *Lidia Zawadzka-Głos2
Unusual location of the ectopic salivary glands – a case report
Ślinianka ektopowa o nietypowej lokalizacji – opis przypadku
1Student, member of Students’s Association Otorhino, working by the Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
2Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Associate Professor Lidia Zawadzka-Głos, MD, PhD
Streszczenie
Termin „heterotopia ślinianek” obejmuje 3 jednostki chorobowe: dodatkowe gruczoły ślinowe, wady wrodzone związane z anomalią łuków skrzelowych oraz „właściwą” heterotopię (HSGT). HSGT jest definiowane jako obecność tkanki gruczołów ślinowych w lokalizacji poza większymi, mniejszymi czy dodatkowymi śliniankami, przy jednoczesnym wykluczeniu klinicznie i histopatologicznie cech charakterystycznych dla wad łuków skrzelowych. Prawdziwa heterotopia występuje rzadko, zazwyczaj zlokalizowana jest w dolnym rejonie szyi. Istotne jest, by pamiętać, że tkanka ta jest zdolna do reakcji w odpowiedzi na typową stymulację do produkcji śliny, a także może ulegać zmianom chorobowym typowym dla gruczołów ślinowych.
W naszej pracy chciałybyśmy przedstawić przypadek 7-letniego chłopca przyjętego do szpitala z powodu okrągłej, czerwonej, uszypułowanej zmiany zlokalizowanej na tylnym łuku podniebiennym po stronie prawej, która ostatecznie została zdiagnozowana jako ślinianka ektopowa.
Summary
Under the term „salivary heterotopia” we can distinguish 3 entities, which are accessory salivary glands, branchial cleft anomalies containing salivary gland tissue and finally heterotopic salivary gland tissue (HSGT). True HSGT is defined as presence of a normal salivary tissue outside of the major, minor, or accessory salivary glands, together with exclusion of clinical and histopathological features characteristic for branchial cleft anomalies. It is a rare condition, usually localized in the lower neck region. It is important to remember that it reacts with physiological saline-production stimulation and can be affected by all salivary glands’ disorders.
In our article we would like to present a case of a 7-year-old boy presented with pedunculated, red, globular lesion in the right posterior tonsillar arch, which was diagnosed as an ectopic salivary gland.
Introduction
Salivary heterotopia may occur in 3 forms: as accessory salivary glands, in association with branchial cleft anomaly or as a heterotopic salivary gland tissue (HSGT) (1). Accessory salivary glands are localized close to the major glands and have a duct that connects to the main salivary duct, most frequently they are associated with Parotid gland and Stenson duct, with the prevalence up to 25% of the population (1). Branchial cleft anomalies, due to their embryological origin, contain tissue that may differentiate into salivary gland tissue (1). In contrast, true heterotopic salivary gland tissue (HSGT) is defined as presence of a normal salivary tissue outside of the major, minor, or accessory salivary glands, together with exclusion of clinical and histopathological features characteristic for branchial cleft anomalies (1-3). They present as masses, cysts or draining sinuses (4) and may be classified by its location into intranodal, most commonly in periparotid lymph nodes (2, 3) or extranodal, typically occurring in the lower neck region, along the anterior border of the sternocleidomastoid muscle (5). However, numerous other locations have been reported including mandible, parathyroid glands (6), larynx (so far 5 cases in English literature) (7, 8), middle ear (9), gastrointestinal tract (10, 11) cheeks (12). True HSGT is a rare condition. Out of 119 patients with lateral neck anomalies treated in the University Department of Otolaryngology in Madrid, Spain in the period of 12 years in 10 patients salivary gland tissue was identified, but only 5 accomplished criteria for HSGT (13).
Most lesions are diagnosed within the first months of life or in the early childhood. Typical clinical manifestation is a draining sinus, painless swelling or enlarged nodule, located unilaterally on the right side of the lower parts of the neck, often accompanied by intermittent draining of a clear, saliva-like fluid, connected with meal consumption (5, 13). Occasionally, ectopic salivary glands can appear bilaterally, and those patients often have family history of cervical anomalies (14). Interestingly, Hsu et al. reported a case of familial ectopic salivary gland which persisted through five generations – the pedigree of the propositus indicated an autosomal dominant pattern of inheritance (15).
The pathogenesis of these remains uncertain. There are several concepts, but the one that appears the most widely accepted is that some elements of the branchial arches become displaced during the embryologic development and an ectopic ectomesenchyme induces the development of a heterotopic salivary gland- type tissue (1). Other theories include abnormal differentiation of local tissue, dislocation of a portion of one of the normal salivary glands, inclusion of salivary tissue in lymph nodes, and abnormal migration of normal salivary tissue (1).
Below we would like to present an example of an unusual location of ectopic salivary glands within the oral cavity that was observed in our clinic.
Case report
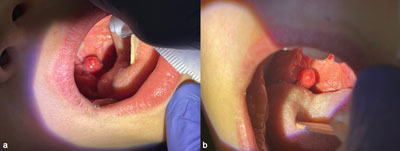
A 7-year-old boy presented to the Department of Pediatric Otorhinolaryngology of Medical University of Warsaw with the exacerbation of symptoms that appeared 2 weeks prior. These symptoms included hoarseness, subtle dysphonia, hypersalivation, dysphagia and globus sensation. He denied pain or dyspnea. In the ORL examination a red globular pedunculated lesion with the diameter of 1 cm was found in the right posterior tonsillar arch (fig. 1a, 1b). The patient’s mother declared that a lesion in the same location had already been detected within the past several years. Since then, the pathology was under observation during laryngological follow-up visits after external ear canal reconstruction. Atresia of the external ear canal was his concomitant inborn defect treated in a different otorhinolaryngological unit. According to mother’s knowledge (no previous medical history was accessible) the diameters of the lesion were stable and until the time of admission to the hospital was symptomless. She also denied fever, night sweating or sudden loss of weight. His laboratory blood tests were normal. During diagnostic process he was qualified for CT with contrast. Due to the technician’s/radiologist’s fault the result of imaging was inconclusive – performed imaging was not fully embracing our lesion. Due to the long, asymptomatic history and low oncologic probability we decided not to repeat the CT (having in mind the radiation exposure) and our patient was qualified for the diagnostic biopsy. The procedure of surgical excision was made, with no complications. The lesion was cut off along the end of the pedunculated structure, without any broader margins. The patient’s post-operative course was unremarkable. The result of the histopathological examination showed an ectopic salivary gland that was totally excised. That is why no further steps were undertaken. All symptoms that lead to specialist consultation and admission to the hospital released after the procedure and full recovery.
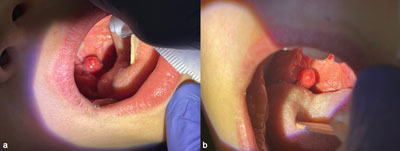
Fig. 1a, b. Clinical presentations of our patient on admission (own clinical material, Department of Pediatric Otorhinolaryngology, Medical University of Warsaw)
Discussion
In the area of the palatine tonsils and arches we may encounter various pathological masses. The differential diagnosis should include anomalies like hypertrophic tonsil, peritonsillar abscess, Hodgkin or non-Hodgkin lymphoma or tonsillar tumors (16). The signs that can indicate a potentially serious pathology in this region are unilaterality of the changes that causes the asymmetry of the tonsils, or even a visible tumor of the neck, lack of the improvement after anti-inflammatory treatment, ulceration of the tonsil mucosa, adenopathy (16). A patient may also complain of dysphagia or pain in the throat. We should also pay attention to other general clinical symptoms of the neoplasia like fever, profuse nighttime perspiration or weight loss (16). But, as our case shows, the presence of some of these signs and symptoms may turn out as a rare, but benign condition.
Heterotopic salivary glands tissue may undergo the same processes as anatomical salivary glands. Cancers arising from HSGT are infrequent and most of them (up to 80%) are benign (4). Daniel and McGuirt identified and analyzed 15 heterotopic salivary glands tumors. 9 of them were benign neoplasm with Whartin’s tumor being the most prevalent (8 cases). The 6 malignant cancers involved 3 mucoepidermoid of which 2 were classified as high grade at time of excision, 2 acinic cell cancer and 1 adenocarcinoma. All these patients received surgical treatment. In the follow-up, one patient deceased from the disease, 13 were alive or deceased of an unrelated cause and 1 was lost to follow-up. The authors emphasized that ectopic salivary gland tissue in the cervical region is probably underdiagnosed and more common than recognized (4). Several other cases of neoplasm occurring in HSGT were reported over past years including acinic cell carcinoma (17), sialoblastoma (12), pleomorphic adenoma (18). The differentiation between primary tumors in the heterotopic salivary tissue and metastatic growth arising from the proper salivary glands may pose a major diagnostic difficulty. The authors seem to agree that a careful search for sites of the primary origin should be carried out in patients presenting with salivary malignancy in the neck.
Another clinicians’ concern and possible reason for the patients to seek medical consultation is infection of the heterotopic salivary glands. Haemel et al. reviewed 11 cases of HSGT from 1983 until 2005 of which 9 revealed periductal chronic inflammation (5). Otherwise, the most common reason for the ectopic salivary gland excision is the patient’s aesthetic concern. The diagnostic path, as in all cervical masses, should include physical examination and imaging: ultrasonography and CT scan or MRI (4). A Fine Needle Aspiration (FNA) should be also done, if possible, to get tissue samples for the histopathological examination that is necessary for the clear definitive diagnosis and proper treatment (4, 7, 18).
In general, the management of ectopic salivary glands, independently of its location, as a treatment of choice is regarded resection, in cervical location usually in a form of a simple excision (neck mass) or parotidectomy (periparotid masses) (1, 4). There was no incidence of the recurrence of the lesion due to Daniel and McGuirt, even when the tumor of the ectopic salivary gland was malignant (4). Patients with lesions that are left without resection should remain under observation on an outpatient basis (8). Any changes of the lesion itself or perceptions of the symptoms should be reported in the follow-up visits (8).
Conclusions
Heterotopic salivary gland tissue (HSGT) is a rare condition. They need to be distinguished from accessory salivary glands and branchial cleft anomalies. HSGT in the neck region can resemble inborn anomalies, while more unusual locations may increase oncological threat and require thorough patient’s history enquiry as well as physical examination, usually combined with imaging. Our case is a rare and benign example of tonsillar asymmetry, which is always a „red flag” when noticed for the first time. We should also remember that HSGT may be affected by all salivary glands’ disorders.
Piśmiennictwo
1. Cannon DE, Szabo S, Flanary VA: Heterotopic salivary tissue. Am J Otolaryngol 2012; 33(4): 493-496.
2. Shinohara M, Harada T, Nakamura S et al.: Heterotopic salivary gland tissue in lymph nodes of the cervical region. Int J Oral Maxillofac Surg 1992; 21(3): 166-171.
3. Neuman T, Maly A, Alterman M et al.: Salivary Gland Heterotopia, a Clinical and Pathological TNM Staging Challenge – Carcinoma ex Pleomorphic Adenoma Arising in a Parotid Lymph node. Cancer Treat Res Commun 2021; 28: 100435.
4. Daniel E, McGuirt WF Sr: Neck masses secondary to heterotopic salivary gland tissue: a 25-year experience. Am J Otolaryngol 2005; 26(2): 96-100.
5. Haemel A, Gnepp DR, Carlsten J, Robinson-Bostom L: Heterotopic salivary gland tissue in the neck. J Am Acad Dermatol 2008; 58(2): 251-256.
6. Edwards PC, Bhuiya T, Kahn LB, Fantasia JE: Salivary heterotopia of the parathyroid gland: a report of two cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 99(5): 590-593.
7. Valentino W, Paknezhad H, Sataloff RT: Heterotopic Salivary Gland Tissue in the Larynx. Ear Nose Throat J 2020; 99(8): NP84-NP85.
8. Shori T, Kouichi Y, Ryuzaburo H, Katsuhisa I: A case of ectopic salivary gland of the larynx, Auris Nasus Larynx 2018; 45(3): 633-636.
9. Morimoto N, Ogawa K, Kanzaki J: Salivary gland choristoma in the middle ear: a case report. Am J Otolaryngol 1999; 20(4): 232-235.
10. Schulberg SP, Serouya S, Cho M, Gadangi PK: Ectopic salivary gland found on rectal biopsy-a rare pathological diagnosis. Int J Colorectal Dis 2020; 35(5): 967-969.
11. Lee JH, Kim S, Kim SJ: (Heterotopic Salivary Gland Tissue at the Hepatic Flexure of the Large Intestine: A Case Report). Korean J Gastroenterol 2018; 72(4): 213-216.
12. Marucci DD, Lawson K, Harper J et al.: Sialoblastoma arising in ectopic salivary gland tissue. J Plast Reconstr Aesthet Surg 2009; 62(8): 241-246.
13. Lassaletta-Atienza L, López-Ríos F, Martín G et al.: Salivary gland heterotopia in the lower neck: a report of five cases. Int J Pediatr Otorhinolaryngol 1998; 43(2): 153-161.
14. Ogawa K, Kondoh K, Kanaya K et al.: Bilateral cervical fistulas from heterotopic salivary gland tissues. ORL J Otorhinolaryngol Relat Spec 2014; 76(6): 336-341.
15. Hsu RF, Hsu YC, Huang SC: Hereditary ectopic salivary gland: survey of three generations. Acta Otolaryngol 2006; 126(3): 330-333.
16. Jankowska K, S?miechura-Gan?czarczyk M, Konopka W: [Unilateral palatal tonsillar tumor – case report]. Otorynolaryngologia 2018; 17(1): 36-40.
17. Das R, Nath G, Bohara S et al.: Two Unusual Cases of Acinic Cell Carcinoma: Role of Cytology with Histological Corelation. J Clin Diagn Res 2016; 10(8): ED21-22.
18. Kamath B, Kamath P, Bhukebag P: Pleomorphic Adenoma in Subcutaneous Plane of the Neck: A Rare Entity. J Clin Diagn Res 2015; 9(9): PD24-25.