Małgorzata Badełek-Izdebska, Karolina Raczkowska-Łabuda, *Lidia Zawadzka-Głos
Bacterial laryngotracheobronchitis as one cause of airway obstruction in older children
Bakteryjne zapalenie krtani, tchawicy i oskrzeli jako jedna z przyczyn obturacji dróg oddechowych u starszych dzieci
Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Lidia Zawadzka-Głos, MD, PhD
Streszczenie
Zapalenie krtani, tchawicy i oskrzeli jest częstą, zwykle samoograniczającą się infekcją wirusową. Bakteryjne zapalenie krtani, tchawicy i oskrzeli jest spowodowane wtórnym zakażeniem bakteryjnym wirusowej infekcji krtani prowadzącym do powstania śluzowo-ropnego wysięku, który może spowodować ostrą niedrożność górnych dróg oddechowych, a w konsekwencji doprowadzić do stanu zagrożenia życia. Bakteryjne zapalenie tchawicy powinno być brane pod uwagę w diagnostyce różnicowej każdego dziecka z ostrą niedrożnością górnych dróg oddechowych. Rozpoznanie to powinno być również brane pod uwagę u każdego dziecka z krupem wirusowym, który nie reaguje na konwencjonalne leczenie. Właściwym sposobem ostatecznego rozpoznania bakteryjnego zapalenia tchawicy jest bezpośrednia wizualizacja tchawicy przez bronchoskopię, jednak nie we wszystkich przypadkach może to być konieczne. Postępowanie obejmuje ścisłą obserwację i monitorowanie, wczesne rozpoczęcie podawania antybiotyków o szerokim spektrum działania, leczenie bólu oraz oczyszczanie dróg oddechowych z zalegającej wydzieliny. Decyzja o zabezpieczeniu drożności dróg oddechowych za pomocą intubacji lub tracheotomii powinna być podejmowana indywidualnie w zależności od nasilenia objawów i stanu pacjenta. W przypadku wczesnego rozpoznania i właściwego leczenia można spodziewać się całkowitego wyzdrowienia. Przedstawiamy dwie pacjentki z rozpoznanym zapaleniem krtani, tchawicy i oskrzeli, u których właściwie postawione rozpoznanie pozwoliło na skuteczne wyleczenie.
Summary
Laryngitis, tracheitis and bronchitis is a common, usually self-limiting viral infection. Bacterial laryngitis, tracheitis and bronchitis is caused by secondary bacterial infection of a viral laryngeal infection leading to a mucopurulent exudate that can cause acute upper airway obstruction and eventually lead to a life-threatening condition. Bacterial tracheitis should be considered in the differential diagnosis of any child with acute upper airway obstruction. This diagnosis should also be considered in any child with viral croup that does not respond to conventional treatment. The correct way to definitively diagnose bacterial tracheitis is by direct visualisation of the trachea by bronchoscopy, but this may not be necessary in all cases. Management includes close observation and monitoring, early initiation of broad-spectrum antibiotics, pain management, and clearing the airways of lingering secretions. The decision to secure an airway by intubation or tracheotomy should be made on an individual basis depending on the severity of symptoms and the patient’s condition. If diagnosed early and treated properly, complete recovery can be expected. We present two patients diagnosed with laryngotracheobronchitis, in whom a correct diagnosis allowed successful recovery.
Introduction
Acute laryngotracheobronchitis (LTB) is a particular form of respiratory tract infection that involves all parts of the larynx, trachea and bronchi. It is most common in young children aged between 3 months and 3 years (up to 6 years according to some authors). It also rarely occurs in older children, adolescents and adults. Originally, it is usually an infection of viral aetiology caused by viruses identified in subglottic laryngitis, which undergoes bacterial superinfection. Inflammatory changes and swelling occupy both the larynx and the walls of the trachea and bronchi. The gradually increasing oedema is further aggravated by an increasing amount of thick, easily drying and difficult to expectorate secretion. The tracheal and bronchial mucosa is covered by a layer of fibrous material that covers the inflammation-damaged surface. The cough is tiresome, becoming dry and unproductive over time, and the secretions in the airways cause inspiratory and expiratory dyspnoea, gradually leading to respiratory failure. The infection is usually accompanied by fever, and the patient’s condition is aggravated by the effort required to clear the airways. The implementation of treatment does not bring the expected improvement – despite intensive irrigation and hydration of the airways and the administration of glucocorticosteroids, no improvement in the patient’s condition is observed. Administration of adrenaline by nebulisation is also ineffective in this case. The appropriate management of suspected bacterial laryngitis should be hospitalisation and monitoring of the patient’s airway to confirm the diagnosis.
Case report 1
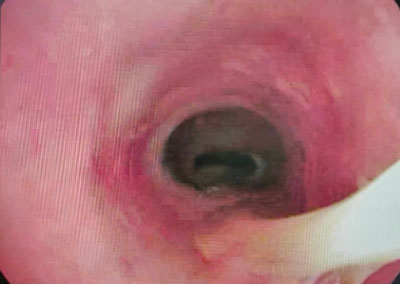
A 10-year-old girl was admitted to the Emergency Department of the Children’s Clinical Hospital of the Medical University of Warsaw because of severe inspiratory and expiratory dyspnoea that did not resolve after anti-inflammatory and bronchodilator drugs, fever to 38.7°C and cough. In addition, the patient complained of significant weakness, lack of appetite, a feeling of constriction during breathing and a hushed voice. On admission, the girl was in average general condition, visible inspiratory and expiratory dyspnoea, stridor, hushed voice. Saturation 94%, HR 140/minute. Auscultation revealed an intermittent murmur over the lung fields. She received inhalations of a corticosteroid (Nebbud) and fenoterol with ipratropium bromide (Ventolin). She was consulted by the ENT specialist on duty, who performed a nasofibroscopy of the larynx and found the following: pale pink epiglottis without oedema, epiglottal folds reddened, swollen, vestibular folds without inflammatory changes, vocal folds pale, smooth, in the subglottal region a concentrically dried secretion on the tracheal walls was visible (fig. 1).

Fig. 1. Concentrically dried discharge in the subglottal region
The girl was admitted to hospital and qualified for urgent interventional bronchoscopy, which was performed under general anaesthesia. The examination revealed severe inflammation in the airways – the mucosa of the larynx, trachea and main bronchi was swollen, congested, with numerous inflammatory papules, and an evident retention of abundant mucopurulent secretion, especially in the subglottis and trachea (fig. 2). The secretion was collected for bacteriological examination, the bronchi were flushed with saline and aspirated. After the procedure, she was circulatory and respiratory efficient and did not require airway patency protection. In the chest x-ray performed, no abnormalities. Inflammatory parameters in the blood not elevated. Treatment included a broad-spectrum antibiotic in the form of a third-generation cephalosporin (Ceftriaxone), saline inhalations, analgesics and antipyretics, and humidification of the child’s environment. The girl’s vital signs were monitored continuously – saturation fluctuated between 94-98%, HR was normal. In the following days, a mucolytic preparation in inhalations was included in the treatment and respiratory rehabilitation was carried out. The bronchoalveolar lavage examined showed the presence of Streptococcus pneumoniae, which was sensitive to the treatment used. The result confirmed the patient’s diagnosis of bacterial laryngitis, tracheitis and bronchitis. During treatment, a gradual improvement of the general condition and resolution of complaints and symptoms was observed. Therefore, a repeat bronchoscopy was abandoned. The patient was discharged home on day 9 for continued treatment on an outpatient basis.

Fig. 2. Mucopurulent secretion in the trachea
Case report 2
A 10-year-old girl of Ukrainian origin admitted for dyspnoea accompanied by fever up to 38.6°C, cough and sore throat. One month earlier she had suffered from acute subglottic laryngitis treated in a hospital in Kiev with parenteral corticosteroid with good results. The day before the current admission, she developed a dry, agonising cough and attacks of dyspnoea. During the consultation, nasofibroscopy was performed, finding: a pale, non-edematous epiglottis with dilated vascular pattern, reddened and oedematous laryngeal aureus with features of laryngopharyngeal reflux and pale, smooth vocal folds. In the subglottic region, purulent-mucous content is seen moving during coughing (fig. 3). After several attempts to expectorate, the secretion lodges on the anterior wall of the trachea to a small extent, without significantly narrowing the airway lumen.
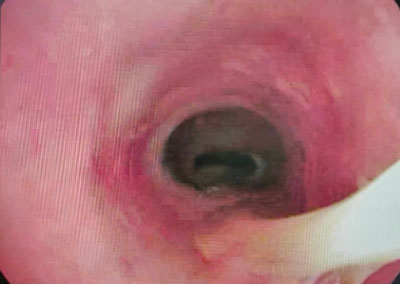
Fig. 3. Mucopurulent secretions in the subglottic and tracheal regions
Based on the symptoms and physical examination, a diagnosis of laryngotracheobronchitis was made. There was no indication for emergency interventional bronchoscopy. In the lung x-ray performed – no deviations, inflammatory parameters were moderately elevated. After admission to the ward, treatment included third-generation cephalosporin (Ceftriaxone), inhalation with 1.5% saline, analgesics and antipyretics, and humidification of the child’s environment. Respiratory physiotherapy was also provided. The patient’s vital signs were monitored continuously – saturation fluctuated between 97-100%. During the course of treatment, an improvement in the general condition and resolution of symptoms was observed. The girl was discharged home on the 8th day of treatment after the complaints had resolved.
Discussion
One of the earliest descriptions of acute (non-membranous) LTB, is considered to be an article by Dr Harry Baum, published in JAMA in 1928 (1). The disease he described almost 70 years ago included cases that are similar to modern descriptions of bacterial tracheitis. In his description of the severe course of the disease in 24 patients (10 of whom died), „glue-like” secretions were found in the tracheobronchial airways. In 10 cases, streptococci were isolated. The authors, who were familiar with diphtheria and non-diphtheria LTB, found similarities in clinical symptoms between the two conditions. However, the nature of the exudate found in the trachea differed, with diphtheria causing a more fibrous exudate compared with the more purulent nature of the discharge in LTB. Prior to the advent of antibiotics, mortality rates for laryngeal diphtheria ranged from 50 to 70%, far exceeding the 25% mortality associated with laryngeal diphtheria. Bacterial tracheitis, then referred to as non-bacterial laryngotracheitis and bronchitis with effusion, was commonly diagnosed and described in the literature in the 1940s and 1950s. After this time, bacterial LTB ceased to be addressed until the 1970s, which may have been related to the widespread use of antibiotics in inflammatory childhood diseases. In 1979, Jones, Santos and Overall published an article in JAMA describing eight infants and children presenting with acute obstructive airway infection with features common to epiglottitis and subglottic laryngitis (croup) (2). Patients did not respond to typical treatment for these entities, including a lack of response to adrenaline nebulisations. Due to the culturing of bacterial pathogens from the thick mucopurulent secretions collected during suctioning, the new-age disease entity became known as „bacterial tracheitis”. It is now referred to in the literature as „membranous laryngotracheobronchitis”, „bacterial laryngotracheobronchitis” or „pseudomembranous croup” (3).
Although the exact pathogenesis of bacterial tracheitis is unknown, hypotheses include (A) primary bacterial infection, (B) primary viral infection with bacterial superinfection, (C) bacterial and viral co-infection and (D) severe viral infection with bacterial colonisation. Of these, the concept of bacterial tracheitis as a complication of viral croup has the most supporters. This hypothesis is supported by the results of patients in whom both viral and bacterial agents were isolated from tracheal cultures. Some viral infections may interfere with systemic cellular immune function or local phagocytic function. In addition, viruses and bacteria may interact to facilitate mutual spread and multiplication. Among the viruses most commonly identified during isolation, parainfluenzae viruses types 1 and 3 predominate. Other viruses responsible for primary infection include respiratory syncytial virus (RSV), rhinoviruses, enteroviruses, influenza viruses and adenoviruses (4). Among bacterial pathogens, methicillin-susceptible Staphylococcus aureus is the most commonly detected in culture samples of respiratory tract secretions. Haemophilus influenzae, Streptococcus pneumoniae, Moraxella catarrhalis, Streptococcus pyogenes are also frequently identified (5, 6). Less frequently isolated are: Klebsiella, Pseudomonas aeruginosa, Mycoplasma pneumoniae (7). Local and systemic factors may contribute to the development of secondary bacterial laryngotracheobronchitis. Ruptures of the respiratory epithelium and loss of cilia function impair local host defence. In addition to viral infection, other conditions are associated with bacterial tracheitis. Bacterial LTB has been reported as a complication of airway procedures, including intubation and tonsillectomy/adenoidectomy (8). Local tissue damage caused by the endotracheal tube may allow bacteria to adhere to the trachea in the same way as a viral infection (9).
The clinical picture consists of a variety of symptoms of upper respiratory tract disease with fever, cough and varying degrees of respiratory distress. Symptoms of LTB may be a combination of those of viral laryngitis, tracheitis and bronchitis with epiglottitis. Bacterial LTB differs from acute epiglottitis and viral LTB due to the longer duration of symptoms and the presence of the typical ineffective cough, which is much more severe. Excessive salivation may occur occasionally. The mucosa of the larynx, trachea and bronchi is swollen and congested. The inflammatory process damages the superficial epithelial layers, leading to the formation of membranous fibrous plaques. These plaques, combined with a thick, mucopurulent secretion extending from the subglottic region to the bronchi, dry out, sometimes forming casts of the airway lumen. These membranes are called „pseudomembranes” because, unlike diphtheria, they easily separate from the substrate without causing bleeding (pseudocroup, pseudomembranous croup).
In laboratory tests, leukocyte counts range from normal to moderately elevated, usually with a predominance of neutrophils. CRP values may also be normal or elevated. Blood cultures taken at the peak of fever are often negative, but should be taken if sepsis is suspected or the patient is immunocompromised.
Lateral neck X-rays may show narrowing of the airway in the subglottic region („candle dripping” sign) with irregular wall outline intratracheally. The epiglottis should appear normal (10).
Endoscopic examination of the airway is conclusive in the differential diagnosis. In patients whose general condition allows it, we can initially perform laryngeal nasofibroscopy, assessing the supraglottic region and the glottis. In other patients and if deviations are found on fibreoptics, assessment of the larynx and tracheobronchial tree under general anaesthesia is indicated (11). Laryngotracheobronchoscopy is not only of diagnostic importance – allowing the diagnosis to be established or confirmed – but above all of therapeutic significance. Removal of lingering secretions and fibrin deposits from the airway lumen reduces obstruction and allows the collected material to be transferred for microbiological examination. Airway endoscopy also allows monitoring of the course of the disease. Sometimes, a single procedure is not sufficient to improve the patient’s condition, due to re-occurrence of airway obstruction through re-emerging secretions and fibres. In such cases, consideration should be given to intubating the patient or even performing a temporary tracheostomy and repeated mechanical removal of airway obstructions (7).
A patient with suspected laryngotracheobronchitis requires inpatient treatment and close observation and monitoring of basic vital signs. Monitoring of saturation and administration of humidified oxygen when saturation falls can prevent the onset of respiratory failure. Unlike patients with croup, patients with bacterial tracheitis do not respond to nebulised adrenaline administration.
Parenteral broad-spectrum empirical antibiotic therapy is initiated from the start of treatment and adjusted if a specific pathogen is cultured according to the antibiogram result. Current guidelines recommend a 10- to 14-day course of antibiotics (12). Amoxicillin with clavulanic acid, clindamycin with third-generation cephalosporin, ceftriaxone plus vancomycin or nafcillin, and ampicillin with sulbactam are used as first-line drugs (13). Proper hydration of the patient, both orally and intravenously, and humidification of the air in the patient’s environment, including by saline inhalation, is of great importance. Mucolytic drugs to help liquefy secretions can be administered orally or by inhalation. Respiratory physiotherapy should be included from the outset to assist the patient in the proper evacuation of residual secretions. Glucocorticoids have not been shown to alter the clinical course or outcome (14, 15). Antiviral treatment may be beneficial if it is established that the preceding viral aetiology is influenza and symptoms are present for less than 48 hours. Routine empirical antiviral treatment is not recommended (10).
Hypoxaemia, respiratory muscle fatigue and tachypnoe may signal a threatening airway failure. Endotracheal intubation may be necessary to ensure airway patency in patients with severe symptom severity, severe general condition or when frequent removal of airway secretions is required. Tracheotomy is reserved for the few patients with laryngitis and tracheitis in whom symptoms of mechanical airway obstruction persist for an exceptionally long time. If diagnosed and treated early, complete recovery can be expected.
Conclusions
Bacterial laryngotracheobronchitis should be considered in the differential diagnosis in children with viral croup-like disease that does not respond to conventional treatment.
A patient with suspected laryngotracheobronchitis requires inpatient treatment and close observation and monitoring of baseline vital signs.
In the case of suspected bacterial LTB, nasofibroscopy and/or bronchoscopy should be performed to confirm the diagnosis and to remove any residual airway secretions.
Broad-spectrum intravenous antibiotic therapy should be given for 10-14 days and adjusted depending on the antibiogram result.
Severe laryngitis and tracheitis may require urgent intubation or even tracheotomy to prevent airway obstruction and to allow repeated removal of secretions.
Piśmiennictwo
1. Baum HL: Acute laryngotracheobronchitis. JAMA 1928; 91(15): 1097-1102.
2. Jones R, Santos JI, Overall JC: Bacterial tracheitis. JAMA 1979; 242: 721-726.
3. Wen SH, Lin L, Yu G et al.: Pseudomembranous laryngotracheobronchitis due to coinfection with human bocavirus 1 and Mycoplasma pneumoniae: a case report. Transl Pediatr 2021; 10(3): 673-678.
4. Johnson DW: Croup. BMJ Clin Evid 2014; 2014: 0321.
5. Kuo CY, Parikh SR: Bacterial tracheitis. Pediatr Rev 2014; 35: 497-499.
6. Blot M, Bonniaud-Blot P, Favrolt N et al.: Update on childhood and adult infectious tracheitis. Med Mal Infect 2017; 47(7): 443-452.
7. Uba A: Infraglottic and bronchial infections. Prim Care 1996; 23(4): 759-791.
8. Eid NS, Jones VF: Bacterial tracheitis as a complication of tonsillectomy and adenoidectomy. J Pediatr 1994; 25: 401-402.
9. Farber HJ, Berg RA: Bacterial tracheitis as a complication of endotracheal intubation. Pediatr Pulmonol 1991; 11: 87-89.
10. Al-Mutairi B, Kirk V: Bacterial tracheitis in children: Approach to diagnosis and treatment. Paediatr Child Health 2004; 9(1): 25-30.
11. Eckel HE, Widemann B, Damm M, Roth B: Airway endoscopy in the diagnosis and treatment of bacterial tracheitis in children. Int J Pediatr Otorhinolaryngol 1993; 27(2): 147-157.
12. Kasian GF, Bingham WT, Steinberg J et al.: Bacterial tracheitis in children. CMAJ 1989; 140(1): 46-50.
13. Blot M, Bonniaud-Blot P, Favrolt N et al.: Update on childhood and adult infectious tracheitis. Med Mal Infect 2017; 47(7): 443-452.
14. Tebruegge M, Pantazidou A, Thorburn K et al.: Bacterial tracheitis: a multi-centre perspective. Scand J Infect Dis 2009; 41(8): 548-557.
15. Liston SL, Gehrz RC, Siegel LG, Tilelli J: Bacterial tracheitis. Am J Dis Child 1983; 137(8): 764-767.