© Borgis - New Medicine 3/2004, s. 71-73
Anna Bielicka, Lidia Zawadzka-Głos, Mieczysław Chmielik
Laryngeal cysts in children
Department of Paediatric Otorhinolaryngology, Medical University of Warsaw, Poland
Head: Prof. Mieczysław Chmielik MD, PhD
Summary
Laryngeal cysts in children include those resulting from an abnormal embryonic development as well as acquired cysts. Congenital laryngeal cysts are relatively uncommon, and are usually found in the early neonatal period; they are most commonly located in the epiglottic portion and they are extremely rare in the glottic and subglottic portions (2, 3, 4). Although the cysts of the larynx are histologically benign, they may contribute to sudden death from asphyxia. The authors present five cases of laryngeal cysts diagnosed and treated at the Department of Paediatric Otorhinolaryngology, Medical University of Warsaw, over the years 1999-2004. It is frequently difficult to diagnose if a cyst is congenital or acquired, especially in children requiring intubation soon after birth.
Introduction
Laryngeal cysts in children may be congenital or acquired. Congenital laryngeal cysts are rare and their incidence is estimated at 1.87 in 100 000 live births (1). They usually produce symptoms in the first days of life, and the epiglottic portion is their most frequent location (epiglottic vallecula, aryepiglottic fold, epiglottis, laryngeal pouch). The cysts are extremely rare in the glottic and subglottic portions (2, 3).
De Santo (1970) divided laryngeal cysts into two types:
1. saccular cysts, related to the laryngeal saccule and resulting from an abnormal dilatation or herniation of the saccule;
2. ductal cysts, resulting from an obstruction in the submucous gland ducts and having a variable location in the larynx (5).
It is worth considering saccular cysts and laryngoceles caused by a dilatated saccule of the larynx. Congenital saccular cysts are believed to be due to a developmental failure in maintaining the patency of the orifice between the saccule and laryngeal ventricle. It is distinct from a laryngocele in that there is no opening into the laryngeal ventricle and it is filled with mucus. Saccular cysts may further be subdivided into anterior and lateral. Laryngoceles are described as dilatated or herniated laryngeal saccules filled with air. They occur mainly in middle- -aged men, exceptionally in neonates, and they are grouped in three distinct categories, i.e. internal, external and mixed laryngoceles (7).
Clinical symptoms of laryngeal cysts vary with their size and location. Large cysts may lead to dyspnoea and stridor. Other symptoms may include dysphonia, stertorous respiration, poor feeding. Saccular cysts produce early postnatal symptoms of airway obstruc-tion, and they are recognised in the first days of life. In laryngoceles, the symptoms are similar to those presented by saccular cysts, but they may become more severe on crying or shouting, which is associated with an increased air pressure in the airway.
The diagnosis of laryngeal cysts is confirmed on direct laryngoscopy. Accessory investigations, performed usually prior to directoscopy, include radiological examination of the neck (lateral projection), chest, oesophagus, USG of the larynx and neck, and NMR or CT of the neck.
Once the diagnosis has been established, laryngeal cysts should be treated surgically. The treatment consists mainly of endoscopic techniques, i.e. conventional microsurgery or CO2 laser. The removal of cysts via an external approach is performed when one or two endoscopic procedures have resulted in recurrences and when the endoscopic treatment is hindered due to deep or extensive cysts.
Case reports
Case 1
A full-term 3,500 gm male infant was delivered spontaneously; his Apgar score was 10 points. From his first days of life, physical examination revealed stertorous respiration indicative of laryngomalacia; however, direct laryngoscopy was not performed to confirm the diagnosis. At the age of 5 months the boy was admitted as a laryngological emergency with symptoms of acute subglottic laryngitis (inspiratory dyspnoea, stridor, barking cough and fever). On admission the patient was given conservative treatment, but on the 5th day his general condition deteriorated: he developed inspiratory dyspnoea and stridor; an emergency endotracheal intubation was performed. The intubation was difficult; it was necessary to use a rigid bronchoscope. Several days later laryngotracheo-bronchoscopy was performed with a 3.5-size instrument. The examination revealed a cyst on the lingual surface of the epiglottis and a concentric soft stricture in the subglottic portion. The cyst extended as far as the piriform fossa. Tracheotomy was performed to repair the stricture in the subglottic portion. Twelve days after the intubation, cyst marsupialization was carried out using an endoscopic technique. NMR examination of the larynx was performed one month later and showed the stricture extending from the level of the true glottis to the level of the tracheotomy tube. The anteroposterior and transverse diameters were 2mm-3 mm and 8mm respectively. At the age of nine months, the patient had the first follow-up directobronchoscopy performed which showed a persistent subglottic stricture, however, without a recurrent cyst. Another repeat endoscopic examination performed six months later revealed a normal laryngeal lumen. The tracheotomy tube was removed; decannulation was successful.
Case 2
A premature, 620 g female infant was delivered by caesarean section at 25 weeks of gestation. She was found to have symptoms of intrauterine infection; the Apgar score was 1. Since she developed symptoms of acute respiratory insufficiency, the infant was intubated immediately after birth. Hyaline membrane syndrome, intraventricular haemorrhage and patent ductus arteriosus were recognised. The arterial duct was ligated on the eighth day of the infant´s life. The patient´s respiration was supported with mechanical ventilation from birth until 51 days of life. On removal of the endotracheal tube laryngel stridor was noted, in view of which, laryngomalacia was suspected. From the 20th month of life the infant developed recurrent lower airway infections (spastic bronchitis, pneumonia, subglottic laryngitis). Since bronchial asthma was suspected, the patient was given antiasthmatic medication. In view of her persistent airway infection accompanied by laryngeal stridor, cough, mixed-type dyspnoea and failure to improve despite the medical treatment, the patient was admitted to our department for endoscopic airway evaluation. On admission the girl was in a moderate general condition, with a laryngeal stridor aggravating on restlessness and exercise. Blood O2 saturation level was 92-98%. Directobronchoscopy showed a large-size subglottic cyst arising from the anterior laryngeal wall, narrowing the laryngeal lumen by almost 90%. The cyst was removed using endoscopic techniques, without intubation. The cyst was found to contain a transparent fluid. Following the surgery the patient´s respiration improved efficiently, and her symptoms subsided. Histopathological examination showed Cystis simplex lined with columnar epithelium.
Case 3
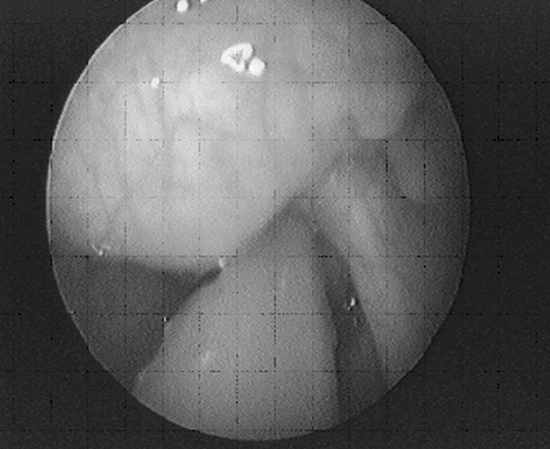
A premature female infant, a second twin, was delivered by caesarean section at 27 weeks of gestation in view of a likely risk of intrauterine infection and escape of the amniotic fluid of the first twin. The infant´s birth weight was 1040 g, the Apgar score 5 points. Congenital pneumonia, hyaline membrane syndrome, intraventricular haemorrhage II/IIIo and patent ductus arteriosus were recognised. From the 1st until 15th day of life the infant required mechanical ventilation support, and subsequently, passive oxygen therapy, until the 30th day of life. At the age of 6 days ligation of the arterial duct wasperformed. After extubation, she was found to suffer from occasional laryngeal stridor, especially after exercise, a mild distress and cough. The case was also suggestive of laryngomalacia (no endoscopic examination was performed). At the age of 7 months, the girl was admitted to our department to undergo an endoscopic evaluation of her respiratory symptoms. On admission her general condition was good. The patient was not dyspnoeic. Directoscopy revealed a small cyst (2-3 mm) arising from the anterolateral laryngeal wall on the left side. The cyst was removed with laryngeal forceps (Photograph 1).

Fig. 1. A cyst present in the subglottic portion (Case 3).
Case 4
The patient was born at term; the delivery was normal. From the third month of life the infant was found to experience snoring, choking and excessive salivation. At the age of 5 months the child underwent the first directoscopy which revealed a cyst at the base of the tongue. The cyst content was aspirated and the infant´s symptoms diminished. When the child was 7 months old, the symptoms aggravated again, and at that time the patient was admitted to our Department. Directo-scopy showed a large cyst in the laryngeal vesti- bule (Photograph 2) which had outgrown the left glossoepiglottic fold, and the cyst duct had penetrated into the piriform fossa. The cyst and its duct (2.5 cm) were removed on an endoscopic procedure. The cyst was found to contain pus.
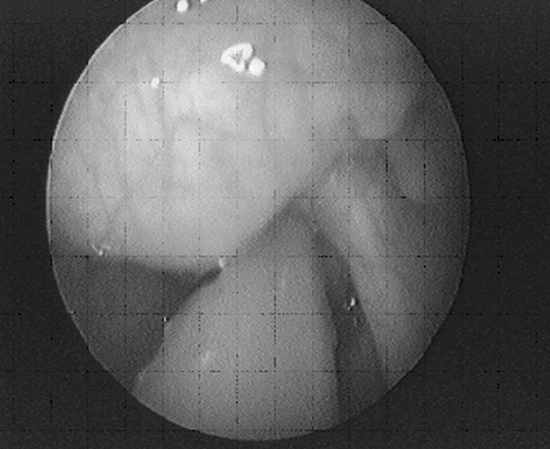
Fig. 2. A large cyst in the vestibule of the larynx outgrowing the left glossoepiglottic fold (Case 4).
Case 5
The patient was admitted to our department at the age of six years. He had been a full-term infant and the delivery had been normal. Stertorous respiration and feeding difficulties had been noticed to occur already in the first days of his life. A directoscopy performed at the age of 7 months had revealed a cyst on the epiglottis. Three operations of cyst removal had been done using endoscopic techniques (at 7 months, 2 and 4 years). Owing to cyst recurrences the child had been qualified for surgery via the external approach to be performed at our department and the surgical operation was carried out when the patient was 6 years old. So far a five-year follow-up has shown that the child has been free of any recurrences.
Discussion
In both cases of subglottic cysts (case 2 and 3), it was difficult to recognize if the cysts were congenital or acquired. We do not know if acute respiratory distress in those patients born at 25 and 27 weeks of gestation had resulted only from their underdeveloped respiratory systems or additionally from the presence of congenital cyst in the subglottic portion. Since most cases of the subglottic cysts reported in literature were recognised in children intubated in the neonatal period, Mitchel´s hypothesis shows that the cysts are due to inflammation produced by the endotracheal tube (2). The healing process consists of granulation and subsequent fibrin tissue formation, which may obstruct the ducts of the subglottic mucous glands, thus, leading to the formation of retention cysts. This observation has been confirmed by Lim who has reported the presence of subglottic cysts in a group of 55 patients (8). All those patients required prolonged intubation in the neonatal period, and the majority of them had been premature infants (94%); inspiratory stridor was also observed in that same group, however, at different times following extubation (8). Lim considers that an increased percentage of children with subglottic cysts noted over the recent years, is associated with an increased number of premature infants requiring prolonged intubation. Premature infants often present with ARS symptoms soon after birth and require immediate endotracheal intubation. Diagnostic endoscopy is usually performed at a later time. The hypothesis of the subglottic cyst formation as a result of injury sustained on intubation seems to be confirmed by a higher incidence rate of the cysts occurring on the left side (78.6%). This may be due to the intubation technique itself since the endotracheal tube is guided into place via the right side of the patient´s oral cavity, and the left side of the subglottic portion is more exposed to injury during the procedure (8).
Conclusions
1. Laryngeal cysts in children are rare conditions, but it should be remembered that these changes are likely to occur if the newborn or infant has dyspnoea, dysphagia or dysphonia.
2. In many cases, it is difficult to determine if the cysts are congenital or acquired, particularly in children requiring intubation soon after birth.
3. The diagnosis of laryngomalacia without endoscopic examination, based only on stridor, may lead to a delayed diagnosis and a life-threatening airway obstruction.
Piśmiennictwo
1. Pak M.W., Woo J.K., van Hasselt C.A.: Congenital laryngeal cysts: current approach to management. J. Laryngol. Otol. 1996 Sep; 110(9):854-6. 2. Triglia J.M., Portaspana T., Cannoni M., Pech A.: Subglottic cyst in a newborn. J. Laryngol. Otol. 1991 Mar; 105(3):222-3. 3. Smith O.D., Callanan V., Harcourt J., Albert D.M.: Intracordal cyst in a neonate. Int. J. Pediatr. Otorhinolaryngol. 2000 May 30; 52(3):277-81. 4. Mitchell D.B., Irwin B.C., Bailey C.M., Evans J.N.: Cysts of the infant larynx. J Laryngol Otol. 1987 Aug; 101(8):833-7. 5. DeSanto L.W., Devine K.D., Weiland L.H.: Cysts of the larynx – classification. Laryngoscope 1970 Jan; 80(1):145-76. 6. Forte V., Fuoco G., James A.: A new classification system for congenital laryngeal cysts. Laryngoscope 2004 Jun; 114(6):1123-7. 7. Cotton R.T., Myer C.M.: Practical Pediatric Otolaryngology. Lippincott-Raven Publishers Philadelphia 1999. 8. Lim J., Hellier W., Harcourt J., Leighton S., Albert D.: Subglottic cysts: the Great Ormond Street experience. Int. J. Pediatr. Otorhinolaryngol. 2003 May; 67(5):461-5.