© Borgis - New Medicine 3/2004, s. 74-76
Anna Chmielik, Jan Ciszecki
Assessment of health-related quality of life
Paediatric Rehabilitation Clinic, Child Health Memorial Hospital, Warsaw, Poland
Head: Prof. Jan Ciszecki MD, PhD
Summary
The growing population of chronically ill and disabled patients requires a new approach to the assessment of their health status. The patient survival is no longer an endpoint in medical care efficiency; quality of life is also important. Although this view is widely accepted, there is still no consensus regarding the definition of health-related quality of life (HRQL), and how the quality of life should be measured. The authors present a brief description of the main concepts of HRQL and methods of measurement with regard to paediatric care.
Advances in medical sciences have brought a significant improvement in medical care, which has resulted in a decreased infant mortality rate, eradication of many infectious diseases as well as an effective prevention and treatment of potentially fatal diseases. Consequently, this has contributed to lifespan extension, but also to an increasingly growing population of disabled and chronically ill patients (1). For example, an improved neonatal care resulted in an increased survival rate of premature infants; however, at the same time it was accompanied by an increased prevalence of neurological problems or vision and hearing disorders. The efficiency of medical care is no longer assessed merely by survival. The quality of life, not only its span, is equally important (2).
Due to their chronic course or dysfunction of social interactions they provoke, certain ENT diseases, may lead to a decreased quality of life, e.g., chronic otitis media, severe hearing loss, chronic speech disorders, upper respiratory infections, tracheostomy. Therefore, while choosing an appropriate treatment, ENT specialists should consider the above-mentioned problem, as well as carry out its assessment.
Despite a significant interest in the subject among researchers, the definition and assessment measures of quality of life are still under debate. There is no one generally accepted definition of quality of life, although there is a consensus that quality of life is a broad, multidimensional concept. It is usually characterized as an overall assessment of physical and mental wellbeing across different, broad domains, including socioeconomic status, characteristics of community and environment as well as other factors (3, 4).
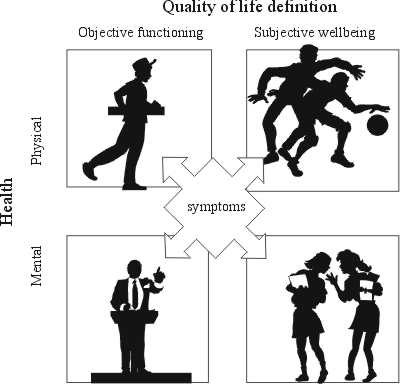
Since the description of quality of life is so broad and imprecise, the term "health-related quality of life” (HRQL) is used in medical sciences. HRQL includes areas of an overall quality of life, which are directly related to an individual´s health, excluding such aspects as income, freedom, air or water quality (3, 4). The concept of quality of life as a component of health is not new. It was highlighted in 1948 by the World Health Organization in the definition of health. Health was described as the presence of physical, mental and social wellbeing, and not only absence of illness (5). Dividing health into physical and mental domains helps understand the influence of health status on HRQL. HRQL can be described as a four-domain structure including both objective and subjective assessment of the patient´s health (6).
Objective physical functioning involves measuring the physical ability to work and perform everyday tasks. Assessment of objective mental functioning is related to the psychological ability to do simple everyday activities, as well as carrying out complex professional and social duties. This part of HRQL is very similar to the assessment of physical and mental disabilities. The subjective assessment provides information about the patient´s feelings. Physical wellbeing reflects general satisfaction from physical health, including information about the sense of discomfort or pain, as mental wellbeing is related to an individual´s psychological comfort, emotional state and social interaction. A traditionally measured health status is only a part of the HRQL assessment, so it is different than the assessment of HRQL (7, 8).
Moreover, there is no simple association between the individual´s health status and wellbeing. Patients with severe disease symptoms do not always describe their quality of life as poor (8), which might result from the mode of assessment. People assess their health-related quality of life by comparing their experience of health with their expectations of it (9). Therefore patients with different expectations will report different quality of life even if their health status is the same. Moreover, patients whose health has changed, may assess their quality of life at the same level. Perception of quality of life varies between people and changes with time (10).
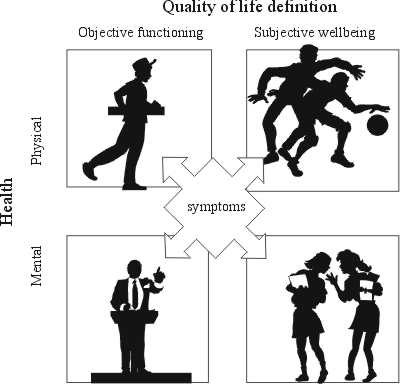
Fig. 1. A classification scheme of quality of life measures. Muldonn 1998.
The purpose of HRQL measurements
HRQL measurements may be used in clinical practice, as well as in establishing health standards and economic analysis.
Assessment of HRQL offers clinicians an opportunity to compare alternative treatments. When there is no difference in mortality rate and both methods of therapy are associated with a possible further diagnostic process and treatment or risk of complications, HRQL measures help to choose the best method (11). The other purpose is to perform an overall assessment of the burden which a severe illness imposes on the patient. The HRQL measurements provide additional useful information not achievable from conventional clinical measures. (For example, an increased ejection fraction of the left ventricle in patients with cardiac disease may not be reflected in changes of their everyday activities (4). In patients with chronic diseases, the assessment of HRQL may help distinguish individuals requiring specialist intervention (11). HRQL measures have also an independent prognostic value in predicting survival rate in oncology (2).
Assessment of HRQL could serve one or more of the three goals: discrimination, evaluation or prediction. Discriminative measures distinguish differences between individuals or groups at a point of time. Evaluative ones assess changes in HRQL during a period of time, and predictive measures are used to predict the future outcome (3, 4, 5, 13).
HRQL instruments
As the concept of HRQL is so broad and multidimensional, there are variable instruments assessing particular domains, and also constructed to be used in different clinical situations. HRQL measures have been developed according to a psychometric approach (14) and represent two basic classes: generic and specific.
The generic measures attempt to assess all important aspects of health across variable HRQL domains, such as the functional and psychological status, social functioning and disease-related symptoms. Since they deal with very broad areas, generic tools may not be sufficiently sensitive to detect changes in specific conditions. Special instruments have been developed for application to particular patient populations.. The measures focus on those aspects of health which are relevant in particular diseases or disorders, and their treatment.
The choice of an appropriate HRQL instrument depends on the research purpose. Generic measures are suitable in large patient populations, so it is possible to carry out a comparison across disease groups or healthy persons and patients. However, the measures are not sufficiently sensitive to detect small changes in individuals. In contrast, specific instruments are used in specific clinical situations which are more sensitive to changes over time. These measures are more appropriate in assessing an impact of specific treatments on HRQL; however, they are not appropriate in patients with more than one disease (3, 4, 5, 11).
Every HRQL measure should satisfy specific criteria i.e. reliability, validity and responsiveness (2, 5). An HRQL tool is reliable when it measures constant results in the same patient who is stable in his HRQL over time (5). Validity refers to the degree to which an instrument measures what it has been developed to measure (4). Responsiveness is an ability of an HRQL measure to detect minimal change in individual´s HRQL over time (13). Apart from that, each HRQL instrument should be minimally burdensome for patients, easy to use and interpret, as well as acceptable for patients and health care professionals (4).
HRQL assessment in paediatrics
The HRQL assessment in children differs widely from the HRQL measurement in adult patients. Firstly, adult HRQL tools are not appropriate in children; it is generally known that children differ from adults in their view of life. For that reason, paediatric HRQL instruments should focus more on such aspects of everyday life as appearance, activities or relationships with peers, rather than being economically productive. They should also be adapted to changes occuring during child development (11, 15). HRQL can be measured by children themselves or by their parents. Although children and parents do not necessarily share similar views on illness and its impact on their quality of life, both types of assessment are valid and complementary (11). Parent-proxy reports may be more useful in longitudinal HRQL researches. They are also useful when children are unable to provide information because of their physical or mental disability (15).
The assessment of treatment and rehabilitation outcome in children with disorders of the central nervous system is particularly difficult. It should include an evaluation of psycho- physical development in terms of the child´s calendar age, the degree of mental development, and the ability to perform every day tasks (16). The assessment can be made by doctors, physiotherapists, teachers, parents or care providers as well as children themselves if it is possible to establish an adequate communication with them. In the USA and Canada, the Gross Motor Function Classification System (GMFCS) is widely used to measure the degree of disability; at present, the system is also recommended in other countries. The standardized assessment of children under 2 years of age, at 2-4 years, 4-6 years and 6-12 years is made by doctors, physiotherapists and other trained medical staff (17). The PEDI measure (Pediatric Evaluation of Disability Inventory) complements the GMFCS evaluation. The method consists of assessing self-care, movement and social interaction over time by the same persons – doctors, physiotherapists, parents (18). It is not easy to introduce such paediatric measures as GMFCS or PEDI as it requires a consensus about methods of assessment or interpretation of outcome. On the other hand, these measures might help clinicians to perform an objective assessment of the treatment chosen (19).
Despite many unsolved problems with the HRQL assessment, it is worth doing it in clinical practice since a better understanding of patients´ quality of life will result in providing them with the best possible holistic care.
Piśmiennictwo
1. Kowalik S., Ratajska A., Szmaus A.: W poszukiwaniu nowego wymiaru jakości życia związanego ze stanem zdrowia. 17-29; w: Wołowicka L. Jakość życia w naukach medycznych. AM Poznań 2001. 2. Eiser C., Morse R.: A review of measures of quality of life for children with chronic illness. Arch. Dis. Child. 2001; 84:205-11. 3. Guyatt G.H., Feeny D.H., Patrick D.L.: Measuring health-related quality of life. Ann. Int. Med. 1993; 118:622-29. 4. Feeny D., Furlong W., Mulhern R.K., et al.: A framework for assessing health-related quality of life among children with cancer. Int. J. Cancer 1999; Suppl 12:2-9. 5. Bjornson K.F., McLaughlin J.F.: The measurement of health-related quality of life (HRQL) in children with cerebral palsy. Eur. J. Neurol. 2001; 8(Suppl 5):183-93. 6. Muldoon M.F., Barger S.D., et al.: What are quality of life measurements measuring? BMJ 1998; 316:542-45. 7. Smith K.W., Avis N.E., Assmann S.F.: Distinguishing between quality of life and health status in quality of life research: a meta-analysis. Qual. Life. Res. 1999; 8:447-59. 8. Feldmann B.M., Grundland B., McCullough L., et al.: Distinction of quality of life, health related quality of life, and health status in children referred for rheumatologic care. J. Rheumatol. 2000; 27:226-33. 9. Calman K.C.: Quality of life in cancer patients- an hypothesis. J. Med. Ethics. 1984; 10:124-7. 10. Carr A.J., Gibson B., Robinson P.G.: Is quality of life determined by expectations or experience? BMJ 2001; 322:1240-43. 11. Eiser C.: Children´s quality of life measure. Arch. Dis. Child. 1997; 77:350-54. 12. Gantz P.A., Lee J.J., Siau J.: Quality of life assessment. An independent prognostic variable for survival in lung cancer. Cancer 1991; 67:3131-35. 13. Jaeschke R., Guyatt G., Cook D., et al.: Określanie i mierzenie jakości życia związanej ze zdrowiem. Med. Prakt. 1999; 4:155-62. 14. Mazur J., Mierzejewska E.: Jakość życia związana ze zdrowiem dzieci i młodzieży – koncepcje, metody badawcze i wybrane zastosowania. Med. Wieku Rozwoj. 2003; 7:35-48. 15. Ronen G.M., Streiner D.L., Rosenbaum P.: Health-related quality of life in children with epilepsy: Development and validation of self-report and parent proxy measures. Epilepsia 2003; 44:598-612. 16. Russanan B.S., Tilton A., Gormeley M.: Cerebral Palsy: A rational approach to a treatment protocol. Muscule & Nerve, suppl 1997; 181-93. 17. Russel D.J., Rosenbaum P.L., Cadman D.T., et al.: The gross motor function measure: a means to evaluate the effects of physical therapy. Dev. Med. Child. Neurol. 1989; 31:341-52. 18. Feldman A.B., Haley S.M., Coryell.: Concurent and construct validity of Pediatric Evaluation of Disability Inventory. Phys. Ther. 1990; 70:602-610. 19. Ketlar M., et al.: Effect of functional therapy program on motor abilities of children with cerebral palsy. Phys. Ther. 2001; 81:1534-1545.