© Borgis - New Medicine 3/2004, s. 77-79
Beata Borawska, Grażyna Bartnik, Danuta Raj-Koziak, Anna Fabijańska, Henryk Skarżyński, Maciej Mrówka
Children with tinnitus and hyperacusis in the material of the tinnitus clinic, Warsaw
Tinnitus Clinic, Institute of Physiology and Pathology of Hearing, Warsaw, Poland
Head: Grażyna Bartnik MD, PhD
Summary
The paper presents a review of 82 children (aged 5-8 years) with tinnitus and/or other hearing disorders diagnosed and treated at the Tinnitus Clinic, the Institute Physiology and Pathology of Hearing. Symptoms, the alleged aetiology and the period of time of the subjective improvement achieved by the children have been assessed. The results have been compared to those obtained in adult patients at our clinic.
Introduction
Data reported by different authors show that the prevalence of tinnitus in children is not frequent and ranges from 1.5% to 1.9% (1). At the Tinnitus Clinic, the Institute of Physiology and Pathology of Hearing, children represent 1.5% of the total number of tinnitus patients. Despite a low prevalence, tinnitus in children is a crucial diagnostic and therapeutic problem (2). So far most reports have associated tinnitus in children with impaired hearing, especially in patients with chronic otitis media (3, 4). Everyday practice at the Tinnitus Clinic shows that children complain of troublesome tinnitus less frequently than adults, sometimes without paying any attention to the disorder. However, the problem is noticed by their parents who wish to know if the condition is dangerous and if and how it may affect the child´s health (2).
Hyperacusis seems to be a more complex problem than tinnitus, and it has an adverse effect on interpersonal communication. Children suffering from both tinnitus and hyperacousis experience the inconvenience to a greater extent than those suffering only from tinnitus (2). Phonophobia poses another problem and should be distinguished from hyperacusis on careful history taking (6).
Upper respiratory infections and complications involving the ears are the most common factors increasing the risk of tinnitus and hyperacusis (3, 5)
Objective
The aim of this study was to carry out a retrospective assessment of children with tinnitus or/and hyperacusis in terms of aetiology, audiological diagnostics and results of adequate treatment.
Material and method
The study group included 82 children at the age ranging from 5 years to 18 years (43 girls (52.4%) and 39 boys (47.6%)); There were 65 (79.3%) children with tinnitus, 11 (13.4%) children with hyperacusis and 6 (7.3%) children with phonophobia; 6 children with hyperacusis also suffered from tinnitus.
Table 1 presents the hearing status and frequency of specific symptoms (tinnitus, hyperacusis, phonophobia) in the study group. Tinnitus occurred more frequently than hyperacusis. There were 25 (30.5%) children with persistent tinnitus who had normal hearing; 6 (7.3%) children had conductive hearing loss; 13 (15.8%) children had perceptive hearing loss; 12 (14.6%) children with normal hearing had periodic tinnitus, 4 (4.8%) children had conductive hearing loss; 5 (6.1%) children were found to have perceptive hearing loss; 3 children (3.6%) with normal hearing suffered from tinnitus and hyperacusis, 3 (3.6%) had perceptive hearing loss. Children with isolated hyperacusis had normal hearing; 5 (6.1%) patients with phonophobia had normal hearing, and there was one child with perceptive hearing loss.
According to the treatment protocol in tinnitus/hyperacusis, children received the same type of therapy as adult patients (7). On consultation the children were accompanied by their parents/one parent. The parents´ assistance was crucial in filling in questionnaires for the tinnitus/hyperacusis children and in taking careful paediatric histories.
Video- and microotoscopy were performed and nasopharyngeal fiberoscopy was done in 4 patients.
Audiological diagnostics started with the middle ear evaluation by means of impedance audiometry. Subsequently, a pure tone audiometry was performed, and uncomfortable level (UCL) for frequency 1.2 and 4 kHz was assessed. In patients with middle ear abnormalities causal treatment (medical or surgical) was instituted. In children with a normal function of the middle ear, DPOAE, ABR- latency, MML and WTN were done. Speech audiometry was carried out in some cases. Ultimately, the children were qualified for tinnitus therapy according to the TRT protocol (Tinnitus Retraining Therapy)
Results
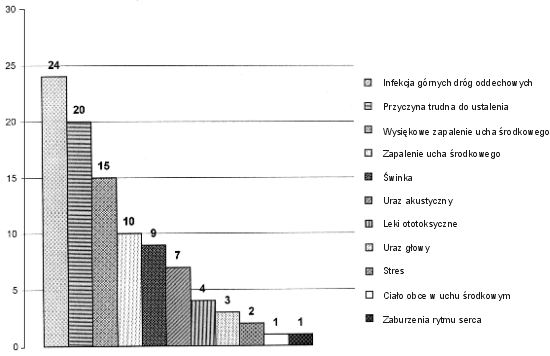
Figure 1 shows the frequency of risk factors of tinnitus and hyperacousis in the study group. The most frequent factors included upper respiratory infections (25%) and chronic otitis media (15.5%). However, it was not possible to indicate the cause of the condition in some cases (20.8%). Other factors were significantly less frequent.
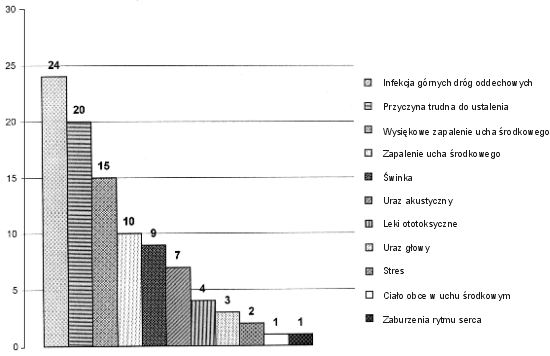
Fig. 1. Aetiology of tinnitus and/or hyperacousis.
Table 1. Aetiology of tinnitus and/or hyperacousis.
| Upper respiratory infection | 24 |
| Unknown cause | 20 |
| Chronic otitis media | 15 |
| Otitis media | 10 |
| Mumps | 9 |
| Acoustic trauma | 7 |
| Ototoxic agents | 4 |
| Head injury | 3 |
| Stress | 2 |
| Foreign body in the middle ear | 1 |
| Dysrhythmia | 1 |
Children suffering from acute upper respiratory infection or from chronic otitis media were treated regarding the cause. Pharmacological treatment was administered in 13 children (15.8%). Eight children underwent surgical treatment (9.6%), adenotomy was performed in two children, four children had tympanotomy and two children, myringoplasty. Children who underwent adenotomy or adenotomy and tympanotomy did not complain of tinnitus. The impedance audiometry was normal. Myringoplasty in one child resulted in a complete remission of tinnitus, the other patient had persistent tinnitus and the child was qualified for TRT. Despite surgical treatment, three children had persistent tinnitus and required a further therapy.
The assessment of children with upper respiratory infection and chronic otitis media showed that a causal treatment guarantees a complete remission of symptoms in a large percentage of cases. Due to medical treatment of acute upper respiratory infections (4 children) and chronic otitis media (7 children), a complete remission was obtained in 11 children (87.5%); in each case, tonal audiometry showed normal hearing. Two children with persistent tinnitus despite the treatment of acute upper respiratory infection, were qualified for TRT.
Eight children underwent surgery, adenotomy was performed in two children, four children had adenotomy and tympanotomy performed, the remaining two children had myringoplasty. After the surgical operation, the children did not have any tinnitus. The result of impedance audiometry was satisfactory. Following myringoplasty, one child showed a total remission of tinnitus, the other child with persistent tinnitus was qualified for TRT. Despite surgical treatment, three children had persistent tinnitus requiring therapy.
Finally, 64 persons were qualified for tinnitus and hyperacusis therapy by using the TRT method.
Three out of 6 children with phonophobia were referred to a psychological consultation, and a suitable sound training was recommended to the remaining three patients. Follow-up assessment showed a rapid remission of hyperacusis. In the group of eight children who underwent hyperacusis TRT therapy, 6 patients (75%) showed significant improvement after 2-3 months, the two others, after 6 months. Most children had subjective improvement after a 2-3 months´ treatment evidenced by remission of symptoms. The thorough diagnostic audiological examination helped recognize the potential source of tinnitus, reduced the parents´ anxiety about the child´s discomfort.
Discussion
The aim of the present study was to perform a retrospective assessment of children with tinnitus and/or hyperacusis with respect to the disease aetiology, audiological diagnostics and therapeutic effects. A detailed history obtained from the patients was the basic tool used in the investigation; it was the first and crucial diagnostic element which helped to work out a further diagnosis; the history of risk factors obtained on the interview from both parents and children allowed the clinicians to perform a reliable assessment of the child´s condition.
Reports have shown that tinnitus in children occurs in a small percentage of cases (only 1.5% were paediatric patients), which was also confirmed by the material obtained at the Tinnitus Clinic, the Institute of Physiology and Pathology of Hearing. Tinnitus was found in 65 children, and hyperacusis only in 11 children. Apart from those symptoms, phonophobia was another problem in children; it was distinguished from hyperacusis on taking the patient´s history. Children with phonophobia exhibited a fear of sound in specific, stressful situations; other loud sounds did not trigger any negative emotions. Children with hyperacusis experienced ear discomfort when exposed to risk factors of tinnitus and hyperacusis.
The most frequent implicit aetiological factors of tinnitus included upper respiratory and ear infections (1, 2, 3, 6), which has also been confirmed by our study. (Figure 1). In the study group of children, ear and upper respiratory infections were recognized in 60% of cases; hence, of importance are an appropriate diagnosis and causal treatment resulting in complete regression; an early treatment prevents development of complications. The treatment in children with tinnitus and conductive hearing loss was effective in 87.5% of cases. Epidemic parotitis (mumps), and particularly, its complications resulting in unilateral hearing loss, are another relatively frequent risk factor of tinnitus in children (8). In our material nine such cases were identified. In profound unilateral conductive hearing loss, a hearing aid (CROS type) was fitted and improved directional hearing which is usually a more severe problem for the child than tinnitus itself (9). Nevertheless, these children were qualified for the TRT therapy. Exposure to noise, in particular an acute acoustic trauma, was reported by 7 patients; four of them had hyperacusis, which impaired interpersonal communication (2, 3, 11).
Sixty four patients underwent a habituation therapy. It is worth mentioning that the outcome was a subjective improvement in children after 2-3 months of the treatment. Thus, the period of time is twice shorter in comparison to that in adults, in whom a significant improvement may be found after at least 6 months of therapy, as confirmed by previous reports (11). The rapid regression in children may be due to a higher plasticity of their central nervous system, and, a bigger capacity than in adults, to create new neuronal connections during systematic sound treatment (2, 3, 12).
Conclusions
1. The frequency of tinnitus and/or hyperacusis in children, according to the material obtained at the Tinnitus Clinic, the Institute of Physiology and Pathology of Hearing, is significantly smaller in comparison to that found in adults.
2. Tinnitus was more frequent than hyperacusis or phonophobia both in adults and children.
3. Upper respiratory infections and otitis media are the most frequent aetiological factors in tinnitus and/or hyperacusis in children.
4. Causal treatment of tinnitus in children with upper respiratory and ear infections provides a complete remission of tinnitus in a large percentage of patients.
5. Habituation of tinnitus and/or hyperacusis proceeds more rapidly in children than in adults.
Piśmiennictwo
1. Bartnik G., Fabijańska A., Rogowski M.: Szumy uszne i nadwrażliwość słuchowa u dzieci – obserwacje własne. Nowa Pediatria, 1998; 11:33. 2. Bartnik G., Fabijańska A., Raj-Koziak D., Rogowski M.: Algorytm postępowania u dzieci z szumem usznym w Klinice Szumów Usznych IFPS. Nowa Pediatria 1999; 17,6:23-26. 3. Graham J.M.: Tinnitus in children with hearing loss. Ciba Foundation Symposium 1981. 4. Mills R.P., Cherry J.R.: Subjective Tinnitus in children with otological disorders. International Journal of Pedistric Otorhinolaryngology 1984; 7:1-27. 5. Mills R.P. et al.: Tinnitus in childhood. Clinical Otolaryngology 1986; 11, 431-434. 6. Jastreboff P.J., Hazel J.P.: A Neurophysological approch to tinnitus: Clinical Implications. British Journal of Audiology 1993; 27:7-17. 7. Bartnik G., Borawska B.: Program terapii szumów usznych metodą TRT. http://www.ifps.org.pl/Plyty/bartnik.html#10 2002. 8. Dziubek Z.: Choroby zakaźne i pasożytnicze. Warszawa: PZWL 1999. 9. Skarżyński H. (red.).: Monografia – Szumy uszne i nadwrażliwość słuchowa. Warszawa: IFPS 1998; roz. 5, 6, 7, 10, 12. 10. Bartnik G., Raj-Koziak D., Fabijańska A.: Szumy uszne i nadwrażliwość słuchowa u dzieci. Audiofonologia 200; XVIII a, 159-165. 11. Bartnik G.: Analiza wyników habituacji u pacjentów z szumem usznym i nadwrażliwością słuchową. Rozprawa na stopień naukowy doktora. Akademia Medyczna w Warszawie 2001. 12. Nodar R.: Tinnitus aurium in school age children. Auditory Research 1984; 12:133-135.