© Borgis - New Medicine 3/2004, s. 83-86
Ireneusz Bielecki, Łukasz Zygan, Ewa Kluczewska*1, Ryszard Tomaszewski, Elwira Nowak-Adamska1
Sino- and otogenic intracranial complications: 2 cases reports
1Department of Otolaryngology, Silesian Health Centre for Child and Mother,
Medical University of Silesia, Katowice, Poland
Head: Ireneusz Bielecki MD
*Department of Diagnostic Imagining, Silesian Health Centre for Child and Mother,
Medical University of Silesia, Katowice, Poland
Head: Ewa Kluczewska MD, PhD
Summary
In opposite to adults, in children intracranial complications occur mainly in acute sinusitis and acute suppurative otitis media.
Infection resulting from an inflammatory process or injury, may spread inwards the skull across a damaged bone, across a natural dehiscence in bone tissue, and also along blood-vessels in an intact bone.
The authors present two cases of sinogenic and otogenic intracranial complications.
An early diagnosis of intracranial complications by means of CT scan, and the surgical removal of the infection foci from the sinus or ear may significantly contribute to a good prognosis.
Epidemiological data are also analysed and literature reports are reviewed.
Introduction
The incidence of oto- and sinogenic intracranial complications has significantly decreased due to the progress in the antibiotic therapy. At present, these life-threatening complications occur mainly in poor populations. In the pre-antibiotic era, the mortality rate resulting from intracranial complications was very high, amounting to 80%-100% (1, 10). Nowadays, the mortality rate in different countries of the world is represented by 5% -15% (5, 12, 13). The decrease in the mortality rate has also resulted from the development of diagnostic imaging as well as highly improved technical skills demonstrated by surgeons operating on the skull base and sinuses. In opposite to adults, in children intracranial complications most often occur in acute sinusitis and acute suppurative otitis media (cholesteatoma, granular tissue) (6, 14); they are considerably less frequent in acute inflammation. The intracranial complications include nonpurulent and purulent cerebrospinal meningitis, epidural abscess, subdural abscess, abscess of the brain and the cerebellum as well as suppurative venous sinuses. About 60% of otogenic intracranial complications are the inflammation of external layer of the dura, and the subdural empyema. Over 7% of cerebrospinal meningitis is otogenic (11, 15). Abscesses of the brain and the cerebellum occur in 0.13% -0.2 % per 100 000 population. Kangsanarak reported intracranial complications in 0.36% of patients treated for chronic otitis media (8). Leskinen estimated the incidence of those complications at approximately 1.1 cases in 100 000 people annually (9). In our geographical region, cerebrospinal meningitis is a prevalent condition. However, a concomitant otitis is not indicative of resulting meningitis. In the material reported by Będziński and Koszewski, purulent foci found in the brain and the cerebellum may be of aural origin (27% of cases) and sinus origin (6.5%) (2). At present, the prevalence of subdural empyema and brain abscess account for about 50-82% of the total sinogenic intracranial complications (3, 4, 6, 7, 12). Otogenic abscesses occur in the temporal lobe or the cerebellum and represent 30-40% of the total abscesses in the cerebral tissue; however, the percentage of frontal lobe abscesses originating from the sinuses is only 10-13% (16). The different frequency of occurrence of these complications is due to higher immunity of the mucous membrane and osseous wall of the sinus as compared with that of the middle ear structures (14). Infection may spread inwards the skull, across a damaged bone, due to an inflammatory process or injury, across the natural dehiscence in bone tissue, and also along blood vessels in an intact bone. Infection may also spread via haematogenic metastases, particularly in immunodeficient patients, when the endogenic focus of infection has been activated. The most common pathogenic bacteria are represented by: Streptococcus pneumoniae, Streptococcus pyogenes, Neisseria meningitidis, Haemophilus influenzae, Staphylococcus aureus and Pseudomonas aeruginosa. The most common bacteria found in purulent foci in infants include Proteus, Klebsiella, Enterococcus and Escherichia coli.
Abscesses occurring in the course of paranasal sinusitis, particularly in the frontal sinuses, are most frequently located in the frontal lobe, and often display an oligosymptomatic course. Pericerebellar otogenic abscesses are most often found in the posterior cranial cavity, and in typical cases, they are manifested by intracranial hypertension, neurological symptoms, and fever. In epidural empyema, manifestations are usually rare, particularly in their frontal lobe location, and they include headache, subfebrile states, and meningeal symptoms. Nausea and vomiting as well as papilloedema may also occur in intracranial hypertension.
Both diagnosis and monitoring of the treatment course are accomplished by means of computer tomography (CT) with a contrast medium.
In intracranial complications resulting from ear or sinus infection, the treatment involves surgical removal of the infection focus and drainage of the abscess. It is also necessary to do bacteriological examination of the material obtained from the abscess. The prognosis in patients with epidural empyema is good, provided that surgical treatment is performed early.
Case reports
Two patients with intracranial complications of paranasal sinusitis and suppurative otitis media were treated at the Department of Otolaryngology, Silesian Health Centre for Children and Mother, Katowice.
Case 1
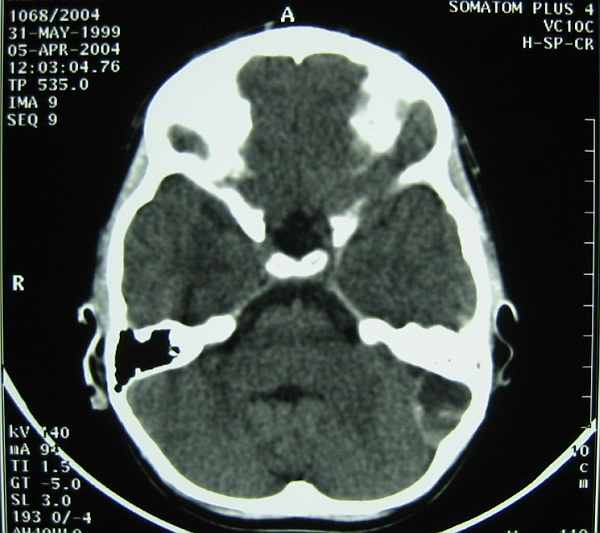
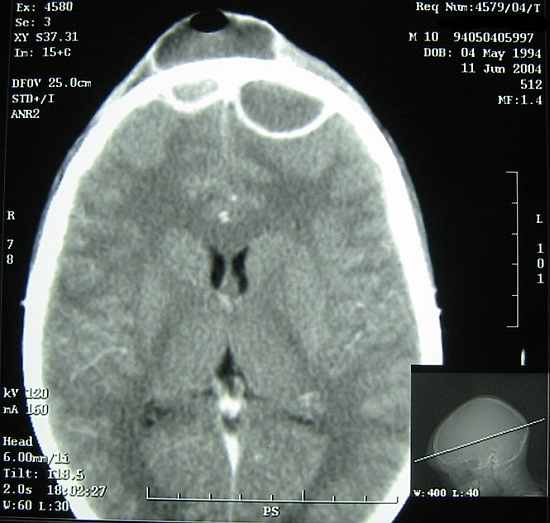
A 5-year-old girl was admitted in severe condition, but she was alert and cooperative. She had severe headache, nausea, diarrhoea and fever of 39 C. The child had been treated for over 6 months for bilateral chronic otitis media with effusion. One week prior to admission the patient had been treated with Clarithromycin for acute pharyngitis. On admission she had symptoms of bilateral otitis media with involvement of the left tympanic membrane, and acute pharyngitis. Nuchal rigidity was present; there were no neurological findings. Lumbar puncture showed evidence of serous cerebrospinal meningitis. CT scan revealed the presence of epidural empyema situated superficially in the left side of the pericerebellum. On neurosurgical consultation it was recommended that neurosurgical treatment should be instituted only in case of an increased intracranial hypertension and /or abnormal neurological symptoms, also with a lack of improvement after otolaryngological surgery. The patient underwent an immediate surgery. The tympanic membrane was incised bilaterally (tympanocentesis), and pus was removed from both tympanic cavities. The antral cavity was opened in the left ear (antrostomy) from which a large quantity of thick pus was evacuated. A drain was left in place in the cavity of empyema. The ear did not reveal typical signs of chronic otitis media with cholesteatoma, granular tissue, or polyps. The suppurative content was examined bacteriologically; the culture showed no growth after 4 days. Antibiotic therapy included Biotraxon, Amikin, Metronidazole. The antral cavity was rinsed with an antibiotic solution twice daily. On the 4th treatment day the patient´s general condition deteriorated; she complained of headache, and nuchal rigidity was also present. CT scan did not show any progression of empyema. On lumbar puncture the cerebrospinal fluid was normal. Therapy with Vancomycin was instituted. Starting from the 5th day, the patient´s condition gradually improved; she received an intravenous antibiotic therapy for 3 weeks, followed by oral antibiotics in the 4th week. Repeat CT scans performed on the 21st day of the treatment, and at 6 weeks after completion of the therapy showed a total remission of empyema.
Case 2
A 10-year-old boy was admitted in severe condition, with a hyperpyrexia (40C), extensive frontal infiltration, and bilateral oedema of the soft periorbital tissues of the ocular region which had started two days previously and had been increasingly progressive. For over 30 days the boy had been treated with antibiotics (Cefuroxime, Azithromycin) for acute sinusitis confirmed radiologically at an outpatients´ clinic. ENT examination on admission revealed a large inflammatory tumour of about 5 cm in diameter, and a huge swelling and inflammation of the soft tissues of the face. CT scan showed bilateral frontal sinusitis, epidural empyemas adjacent to both frontal lobes. Neurological examination was normal, without positive meningeal symptoms, or features of focal CNS damage. On neurosurgical consultation, otolaryngo-logical surgery was recommended, and in the case of progressively severe intracranial hypertension, neurosurgical treatment should be performed immediately. The patient underwent an urgent surgical operation. The frontal sinuses were opened and both subperiosteal and epidural abscesses were removed showing an abundant quantity of pus discharge effluent under pressure, osteoclasia and necrosis of the frontal bone with a large subperiosteal abscess. Sinusoscopy of the left maxillary sinus showed no evidence of inflammatory lesions. Intravenous antibiotic therapy with Clindamycin and Metronidazole was administered for four weeks. The abscess pit and both frontal sinuses were irrigated with an antibiotic solution twice daily. Repeat CT scans showed a complete remission of empyemas.
Conclusions
Early diagnosis of intracranial complications by means of CT scan, and surgical treatment consisting of the removal of infection foci from the sinus or ear offer a good prognosis. Antibiotic therapy should be administered for over 4 weeks, and the treatment results should be controlled with CT. Intracranial complications in acute and chronic paranasal sinusitis and suppurative otitis still seem to pose a problem, in spite of generally used broad-spectrum antibiotics. This concerns especially children in whom an inflammatory process may run a violent course and intracranial complications may develop rapidly.
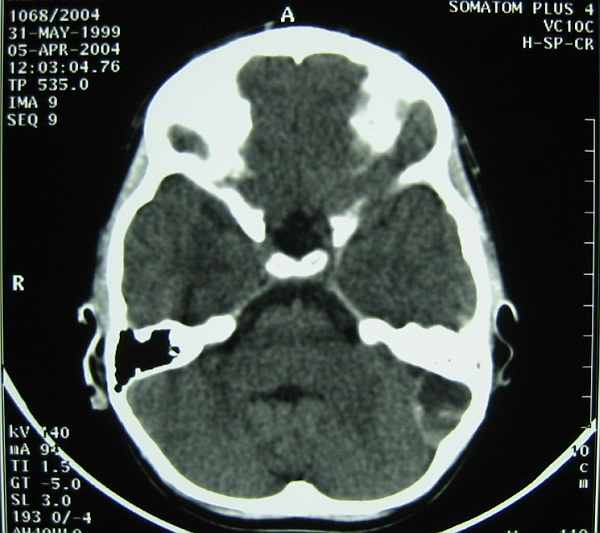
Fig. 1. Case K. J. CT scan of the head. Epidural empyema in the pericerebellum space in the left part.

Fig. 2. Case K. J. CT scan of the head after three-week treatment.

Fig. 3. Case P. A. Inflammatory infiltration and subperiostal abscess on frontal region of the head.
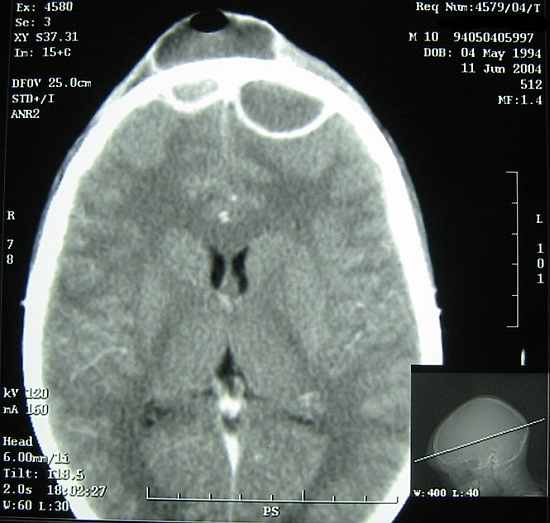
Fig. 4. Case P. A. CT scan of the head. Bilateral frontal sinusitis and bilateral epidural empyemas in anterior fossa.

Fig. 5. Case P. A. CT scan of the head after three-week treatment.
Piśmiennictwo
1. Albu S., Tomescu E., et al.: Intracranial complications of sinusitis. Acta Otorhinolaryngol. Belgian. 2001; 55: 265-272. 2. Będziński J., Koszewski W.: Cause and frequency of occurrence abscesses of the brain and the cerebellum in adult. Dive. Neurochir. Pol. 1988; 32:228-231. 3. Bradley P.J., Manning K.P., Shaw M.D.M.: Brain abscess secondary this paranasal sinusitis. J. Laryngol. Otol. 1984; 98:719-22. 4. Clayman G.L., Adams G.L., et al.: Intracranial complications of paranasal sinusitis: and combined institutional rewiev. Laryngoscope 1991; 101:11, 1245. 5. Gallagher R.M., Gross C.W., Phillips C.D.: Suppurative intracranial complications of sinusitis. Laryngoscope 1998; 108:163-165. 6. Giannoni C.M., Syeward M.G., Alford E.L.: Intracranial complications of sinusitis. Laryngoscope 1997; 107:863-67. 7. Hoyt D.J., Fischer S.R.: Otolaryngological management of patients with subdural empyema. Laryngoscope 1991; 101:20-24. 8. Kangsanarak J., Navacharoen N., et al.: Intracranial complications of suppurative otitis medias: 13 years experience. Am. J. Otol. 1995; 16:104-109. 9. Leskinen K., Jero J.: Complications of acute otitis medias in children in southern Finland. Int. J. Pediatr. Otorhinolaryngol. 2004; 68:317-324. 10. Mamatova T.sh, Rasulova A.K.: Otogenic cerebellar abscesses in the light of 10-year observation materials at the ENT clinic at the Tashkent institute of continuing education of physicians. Vestn. Otorinolaringol. 2000; 4: 47-50. 11. Prusiński A.: Otogenic intracranial complications. In: Janczewski G., Latkowski B.: Otoneurologia. Bel. Corp. Warsaw 1998; 339-350. 12. Singh B., Van Dellen J., Ramjettan T.J.: Sinogenic intracranial complications. J. Laryngol. Otol. 1995; 109:945. 13. Szmeja Z., Kruk-Zagajewska A., Grądzki J., Kulczyński B.: The abscesses of front cranial pit in material in the material of the Otolaryngology Departament, K. Marcinkowski University of Medical Sciences in Poznan in the years1964-1984. Otolaryngol. Pol. 1986; 3:192. 14. Szmeja Z, Kruk-Zagajewska A., Szyfter W., et al.: Intracranial complications of sinusitis in the material of the Otolaryngology Departament, K. Marcinkowski University of Medical Sciences in Poznan in the years 1964-1999. Otolaryngol. Pol. 2001; 55:293-298. 15. Wrodycki W., Kuydowicz J., Krakowiak M., et al.: The epidemiological and clinical analysis of purulent cerebrospinal meningitis in adults. Pol. Tyg. Medicine. 1994; 49:462-464. 16. Zakrzewski A.: Clinical Otolaryngology. PZWL Warszawa 1981; 72.