Michal Zyla1, Karol Bielski1, 2, Marek Dabrowski3, Wojciech Wieczorek4, 5, Halla Kaminska6, Lukasz Czyzewski7, Wladyslaw Gawel8, Jerzy Robert Ladny9, Klaudiusz Nadolny9, *Lukasz Szarpak4, 9
Skills and attitudes toward intraosseous access in cardiopulmonary resuscitation among nursing personnel
Umiejętności i postawy personelu pielęgniarskiego wobec wkłuć doszpikowych podczas resuscytacji krążeniowo-oddechowej
1Polish Society of Disaster Medicine, Warsaw, Poland
2MEDITRANS The Voivodship Emergency Medical Service and Ambulance Transport, Warsaw, Poland
3Department of Medical Rescue, Poznan University of Medical Sciences, Poland
4Department of Emergency Medicine, Medical University of Warsaw, Poland
5Department of Anaesthesiology, Intensive Care and Emergency Medicine in Zabrze, Medical University of Silesia in Katowice, Poland
6Department of Children’s Diabetology, Medical University of Silesia in Katowice, Poland
7Department of Nephrologic Nursing, Medical University of Warsaw, Poland
8Student’s Scientific Association of Children’s Diabetology, Medical University of Silesia in Katowice, Poland
9Department of Emergency Medicine and Disaster, Medical University of Bialystok, Poland
Streszczenie
Wstęp. Uzyskanie dostępu donaczyniowego w przypadku stanu zagrożenia życia u pacjenta jest jedną z kluczowych umiejętności, jaką winien wykazywać się personel medyczny. Podczas resuscytacji krążeniowo-oddechowej, gdy łożysko naczyniowe jest zapadnięte, uzyskanie dostępu dożylnego może być utrudnione i może wpływać na opóźnienie w podaży leków i płynów.
Cel pracy. Celem pracy było porównanie zdolności uzyskiwani dostępu dożylnego i doszpikowego z wykorzystaniem igły Jamshidi i wkłucia doszpikowego NIO podczas symulowanej resuscytacji krążeniowo-oddechowej.
Materiał i metody. Badanie zostało zaprojektowane jako randomizowane krzyżowe i przeprowadzone w warunkach symulacji medycznej. W badaniu wzięły udział 64 pielęgniarki uczestniczące w kursie Advanced Cardiopulmonary Life Support. Podczas badania analizowano czas uzyskania dostępu donaczyniowego oraz łatwość wykonania procedury.
Wyniki. Czas trwania procedury uzyskania dostępu donaczyniowego był zróżnicowany i wynosił odpowiedni 34 s (IQR: 30-43) dla wkłucia dożylnego, 12 s (IQR: 11-15) dla wkłucia doszpikowego z wykorzystaniem NIO oraz 29 s (IQR: 23-38) dla wkłucia doszpikowego z wykorzystaniem igły Jamshidi. Analiza statystyczna wykazała istotne statystyczne różnice w czasie trwania procedury pomiędzy NIO i wkłuciem dożylnym (p < 0,001) oraz pomiędzy NIO i igłą Jamshidi (p < 0,001). Łatwość wykonania procedury była zróżnicowana i wynosiła odpowiednio: 1,5 punktu (IQR: 1-2,5) dla NIO, 4 punkty (IQR: 2,5-4,5) dla igły Jamshidi oraz 4 punkty (IQR: 3-5,5) dla wkłucia dożylnego.
Wnioski. W przeprowadzonym badaniu, pielęgniarki już po krótkim szkoleniu były w stanie uzyskiwać dostęp doszpikowy w czasie krótszym aniżeli miało to miejsce w przypadku dostępu dożylnego. NIO było najbardziej efektywnym spośród badanych urządzeń.
Summary
Introduction. Obtaining intravascular access in life-threatening conditions is one of the key procedures that the medical personnel should be able to perform. During cardiopulmonary resuscitation, when the blood vessels are collapsed, obtaining standard IV access may be difficult and may be associated with a delay in giving drugs and fluids to the patient.
Aim. The aim of the study was to compare the ability to perform intravascular access using a standard intravenous cannula and NIO and Jamshidi intraosseous devices during simulated cardiopulmonary resuscitation conducted by nurses.
Material and methods. The study was designed as a randomized, crossover study and was performed in the conditions of medical simulation. 64 nurses who took part in the Advanced Cardiopulmonary Life Support courses were enrolled in the study. The study analyzed both the time of obtaining intravascular access as well as the easiness of performing this procedure.
Results. The procedure time using distinct intravascular access methods varied and were respectively 34 s (IQR: 30-43) for intravascular access, 12 s (IQR: 11-15) for intraosseous access using NIO device, and 29 s (IQR: 23-38) for intraosseous access using Jamshidi needle. The statistical analysis revealed a statistically significant difference in the procedure time between NIO and IV cannula (p < .001) and between NIO device and Jamshidi needle (p < .001). The easiness of performing the procedure varied and scored: 1.5 points (IQR: 1-2.5) for NIO, 4 points (IQR: 2.5-4.5) for Jamshidi, and 4 points (IQR: 3-5.5) for intravenous cannula.
Conclusions. In the conducted study the nurses after short training were able to provide the intraosseous access with shorter time then intravascular. NIO device turned out to be the most effective among all the devices used in the study.

INTRODUCTION
The ability to obtain intravascular access in life-threatening conditions is one of the key procedures that the medical personnel should be able to perform. Sudden cardiac arrest, anaphylactic shock or hypovolemic shock are only some of the situations of sudden cardiac arrest, which require immediate intravascular access and pharmacotherapy. In the case of cardiopulmonary resuscitation and non-fibrillative rhythms in cardiac arrest – advanced resuscitation procedures also include giving the adrenaline as soon as possible. However, in cases where the vessels are collapsed, peripheral vein cannulation may be difficult or often even impossible to perform.
Intraosseous access is currently the first recommended vascular access in pediatric emergencies such as cardiac arrest or hypovolemic shock, although it is only ranked as the first alternative to intravascular access for adult cardiac arrest (1-4). The medullar cavities of the proximal tibia or the head of humerus are the most commonly used locations for intraosseous access. Pharmacokinetic and pharmacodynamics studies showed that the intraosseous route is equivalent to intravenous access for administration of radionuclide tracers and emergency drugs such as vasoactive drugs (5, 6).
AIM
The aim of this study was to compare the overall time needed for establishing the intraosseous access with the NIO device and Jamshidi needle compared to the overall time for obtaining the peripheral intravenous access, performed by nurses during simulated cardiopulmonary resuscitation.
MATERIAL AND METHODS
This prospective, randomized, crossover observational study was conducted between November 2017 and January 2018. The Institutional Review Board of the Polish Society of Disaster Medicine (Approval number: 32.2017.IRB) approved the study protocol.
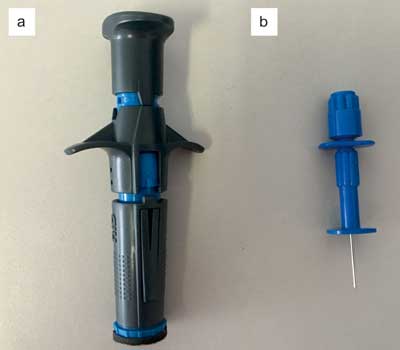
The study used a comparison of intravenous access, during which it was recommended to cannulate the median cubital vein according to the rules of aspiration and antisepsis. In the case of intraosseous access, two devices were used: semi-automatic NIO Adult device and a Jamshidi needle, the access was obtained through the proximal part of the tibia (fig. 1a, b). The procedure of obtaining intraosseous access was also performed with the principles of asepsis and antiseptics.
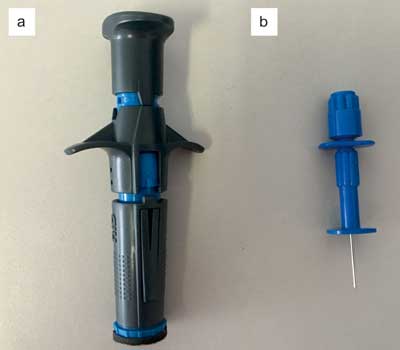
Fig. 1a, b. Intraosseous devices used in the study: (a) NIO Adult Device, (b) Jamshidi needle
Prior to the study, all participants took part in the course regarding the obtaining the intraosseous access. During the training, the instructor discussed and demonstrated the correct way of obtaining access with the aforementioned devices. The study participants did not take part in the practical part.
Immediately after completing the theoretical part, the study participants were divided in three groups, the first one started with obtaining the intravenous access with a standard intravenous cannula, the second group performed intraosseous access with NIO Adult, the third group used the Jamshidi needle. After 20-minute breaks, participants of the study performed intravascular access with another method. A detailed randomization procedure is presented on figure 2.
Fig. 2. Randomization flow chart of the study
The procedure of obtaining the vascular access was performed in the simulated cardiopulmonary resuscitation environment. In order to simulate a patient with cardiac arrest, the Advanced Skill Trainer training manikin was used (Laerdal, Stavanger, Norway). To make the scenario appear more real, cardiopulmonary resuscitation was carried out in accordance with the advanced resuscitation procedures. Additionally, the LUCAS 3 mechanical chest compression system was used to optimize chest compressions.
Powyżej zamieściliśmy fragment artykułu, do którego możesz uzyskać pełny dostęp.
Mam kod dostępu
- Aby uzyskać płatny dostęp do pełnej treści powyższego artykułu albo wszystkich artykułów (w zależności od wybranej opcji), należy wprowadzić kod.
- Wprowadzając kod, akceptują Państwo treść Regulaminu oraz potwierdzają zapoznanie się z nim.
- Aby kupić kod proszę skorzystać z jednej z poniższych opcji.
Opcja #1
29 zł
Wybieram
- dostęp do tego artykułu
- dostęp na 7 dni
uzyskany kod musi być wprowadzony na stronie artykułu, do którego został wykupiony
Opcja #2
69 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 30 dni
- najpopularniejsza opcja
Opcja #3
129 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 90 dni
- oszczędzasz 78 zł
Piśmiennictwo
1. de Caen AR, Berg MD, Chameides L et al.: Part 12: Pediatric Advanced Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015; 132 (18 suppl. 2): S526-542.
2. Link MS, Berkow LC, Kudenchuk PJ et al.: Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015; 132 (18 suppl. 2): S444-464.
3. Soar J, Nolan JP, Böttiger BW et al.; Adult advanced life support section Collaborators: European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation 2015; 95: 100-147.
4. Maconochie IK, Bingham R, Eich C et al.; Paediatric life support section Collaborators: European Resuscitation Council Guidelines for Resuscitation 2015: Section 6. Paediatric life support. Resuscitation 2015; 95: 223-248.
5. Johnson D, Garcia-Blanco J, Burgert J et al.: Effects of humeral intraosseous versus intravenous epinephrine on pharmacokinetics and return of spontaneous circulation in a porcine cardiac arrest model: A randomized control trial. Ann Med Surg (Lond) 2015; 4(3): 306-310.
6. Wimmer MH, Heffner K, Smithers M et al.: The comparison of humeral intraosseous and intravenous administration of vasopressin on return of spontaneous circulation and pharmacokinetics in a hypovolemic cardiac arrest swine model. Am J Disaster Med 2016; 11(4): 237-242.
7. Jones L, Phillips K, Pollack C Jr et al.: A new system for sternal intraosseous infusion in adults. Prehosp Emerg Care 2000; 4(2): 173-177.
8. Szarpak L, Truszewski Z, Smereka J et al.: A Randomized Cadaver Study Comparing First-Attempt Success Between Tibial and Humeral Intraosseous Insertions Using NIO Device by Paramedics: A Preliminary Investigation. Medicine (Baltimore) 2016; 95(20): e3724.
9. Bielski K, Szarpak L, Smereka J et al.: Comparison of four different intraosseous access devices during simulated pediatric resuscitation. A randomized crossover manikin trial. Eur J Pediatr 2017; 176(7): 865-871.
10. Paxton JH, Knuth TE, Klausner HA: Proximal humerus intraosseous infusion: a preferred emergency venous access. J Trauma 2009; 67(3): 606-611.
11. Leidel BA, Kirchhoff C, Bogner V et al.: Comparison of intraosseous versus central venous vascular access in adults under resuscitation in the emergency department with inaccessible peripheral veins. Resuscitation 2012; 83(1): 40-45.
12. Santos AP, Conkin R, Dowd K: Needle Break: Complication and Management of Intraosseous Vascular Access. Am Surg 2017; 83(1): 18-20.
13. Johnson M, Inaba K, Byerly S et al.: Intraosseous Infusion as a Bridge to Definitive Access. Am Surg 2016; 82(10): 876-880.
14. Lewis P, Wright C: Saving the critically injured trauma patient: a retrospective analysis of 1000 uses of intraosseous access. Emerg Med J 2015; 32(6): 463-467.
15. Greenstein YY, Koenig SJ, Mayo PH, Narasimhan M: A Serious Adult Intraosseous Catheter Complication and Review of the Literature. Crit Care Med 2016; 44(9): e904-909.
16. Thadikonda KM, Egro FM, Ma I, Spiess AM: Deltoid Compartment Syndrome: A Rare Complication after Humeral Intraosseous Access. Plast Reconstr Surg Glob Open 2017; 5(1): e1208.
17. Sheils M, Ross M, Eatough N, Caputo ND: Intraosseous access in trauma by air medical retrieval teams. Air Med J 2014; 33(4): 161-164.
18. Reuter-Rice K, Patrick D, Kantor E et al.: Characteristics of Children Who Undergo Intraosseous Needle Placement. Adv Emerg Nurs J 2015; 37(4): 301-307.
19. Lallemand MS, Moe DM, McClellan JM et al.: No intravenous access, no problem: Intraosseous administration of tranexamic acid is as effective as intravenous in a porcine hemorrhage model. J Trauma Acute Care Surg 2018; 84(2): 379-385.
20. Winkler M, Talley C, Woodward C et al.: The use of intraosseous needles for injection of contrast media for computed tomographic angiography of the thoracic aorta. J Cardiovasc Comput Tomogr 2017; 11(3): 203-207.
21. Baadh AS, Singh A, Choi A et al.: Intraosseous Vascular Access in Radiology: Review of Clinical Status. AJR Am J Roentgenol 2016; 207(2): 241-247.
22. Budach NM, Niehues SM: CT angiography of the chest and abdomen in an emergency patient via humeral intraosseous access. Emerg Radiol 2017; 24(1): 105-108.
23. Idris M, Sakkir N, Naik KG, Jayaram NK: Intraosseous injection as an adjunct to conventional local anesthetic techniques: A clinical study. J Conserv Dent 2014; 17(5): 432-435.
24. Polat O, Oğuz AB, Cömert A et al.: Intraosseous access learning curve: is it really practical? Am J Emerg Med 2014; 32(12): 1543-1544.