*Maja Lipiec1, Zuzanna Lipiec-Rzepecka2, Sara Shamsa-Nieckula1, Dorota Olczak-Kowalczyk1
Determinants of dental trauma in 5-year-old children – a questionnaire study in the Polish population
Determinanty urazowych uszkodzeń zębów u dzieci 5-letnich – badania ankietowe populacji polskiej
1Department of Paediatric Dentistry, Medical University of Warsaw
Head of Department: Professor Dorota Olczak-Kowalczyk, MD, PhD
2Multidisciplinary Provincial Hospital in Gorzów Wielkopolski
Hospital Director: Jerzy Ostrouch
Streszczenie
Wstęp. Urazy zębów są rozpowszechnionym zjawiskiem w Polsce i na świecie. Postępowanie związane z urazami zębów mlecznych stanowi wyzwanie diagnostyczne oraz lecznicze. Urazom zębów mogą towarzyszyć liczne powikłania. Dotychczas nie były prowadzone epidemiologiczne badania stomatologiczne, które oceniłyby częstość oraz czynniki determinujące występowanie urazów zębów mlecznych w populacji polskiej.
Cel pracy. Określenie częstości, rodzaju i przyczyn urazów zębów mlecznych oraz sposobu postępowania leczniczego, a także wyodrębnienie czynników korelujących z wyżej wymienionymi parametrami u dzieci w pierwszych 5 latach życia w Polsce.
Materiał i metody. Badania ankietowe przeprowadzono w 15 województwach w ramach programu pt. „Monitorowanie stanu zdrowia jamy ustnej populacji polskiej w latach 2016-2020”. Do badania włączono rodziców dzieci w wieku 5 lat. Kwestionariusz badań zawierał pytania dotyczące czynników socjoekonomicznych, sprawdzające wiedzę rodziców i ich zachowania zdrowotne w odniesieniu do zdrowia jamy ustnej dzieci oraz urazów zębów. Wyniki poddano analizie statystycznej przy poziomie istotności p < 0,05.
Wyniki. Do analizy włączono 1044 prawidłowo wypełnione kwestionariusze. Urazu zęba mlecznego doznało około 10% dzieci, najczęściej w 3. roku życia. Na skutek urazu przeważnie dochodziło do złamania korony oraz zwichnięć zębów. Większość rodziców dzieci, które doznały urazu zęba, zgłosiła brak potrzeby leczenia. Najczęściej stosowaną metodą leczniczą była jednak ekstrakcja.
Wnioski. Skutkiem urazu zęba może być występowanie powikłań, a w konsekwencji pogorszenie jakości życia dziecka. Tylko wczesne zaopatrzenie i leczenie urazów może temu zapobiec.
Summary
Introduction. Tooth injuries are a widespread phenomenon in Poland and worldwide. The management of primary tooth injuries is a diagnostic and therapeutic challenge. Tooth injuries can be accompanied by many complications. No epidemiological studies have been conducted that would assess the frequency and factors determining the prevalence of primary tooth injuries in the Polish population.
Aim. Determining the incidence, type and causes of primary dentition injuries and treatment methods, as well as identification of factors correlating with the above-mentioned parameters in 5-year-olds in Poland.
Material and methods. Questionnaire surveys were conducted in 15 voivodeships as part of the programme entitled “Oral health monitoring of the Polish population in years 2016-2020”. Parents of 5-year-old children were included in the study. The questionnaire included questions on socioeconomic factors, parental knowledge and health behaviours in relation to children’s oral health and dental trauma. The results were analysed statistically.
Results. A total of 1,044 correctly completed questionnaires were included in the analysis. About 10% of children had a history of primary tooth trauma, usually in the third year of life. The most common injuries were crown fractures and tooth luxations. Most of the parents of children who have sustained a tooth injury reported no need for treatment. Extraction was the most common treatment method.
Conclusions. Tooth injury may lead to complications and, consequently, reduced life quality in the child. Only early care and treatment of dental trauma can prevent them.

Introduction
Tooth injuries are a widespread phenomenon both in Poland and worldwide. The prevalence of deciduous tooth injuries is estimated at about 22.7% in the world and about 14.2% in the European region (1). The management of primary tooth injuries is a diagnostic and therapeutic challenge. Therefore, a greater frequency of dental visits is often needed, which frequently results in absence from school or kindergarten (2). Tooth injuries may be accompanied by multiple complications, most often associated with failure to provide proper assistance at the scene of accident or delayed dental appointment. Research has shown that more than half (67.7%) of respondents (teachers and medical professionals) do not consider it necessary to visit a dentist after traumatic loss of a primary tooth (3). Injuries of primary teeth can lead to complications within the affected teeth, such as loss of a tooth or its vitality. They can also be complicated by damage to permanent teeth, e.g. underdevelopment of the enamel of permanent teeth (4% of cases) or compromised enamel quality (32% of cases) (4). The sequelae of injuries are not only a health problem. They may also be associated with increased treatment expenses and deterioration of child’s quality of life, including worse relationships with peers. So far, no epidemiological dental studies have been conducted in Poland that would assess the incidence of primary tooth injuries in the Polish population and the factors determining their occurrence.
Aim
The aim of the study was to determine the incidence, types and causes of deciduous tooth injuries and the treatment procedure, as well as to identify factors correlating with the above-mentioned parameters in 5-year-olds in Poland.
Material and methods
Questionnaire surveys were conducted in 15 provinces as part of the programme entitled “Oral health monitoring of the Polish population in years 2016-2020”, financed by the Ministry of Health (contract No. 11/1/2019/1210/836, paragraph 3, section 23). Parents of 5-year-old children were included in the study. Stratified sampling was used to select the population sample. Poviats, communes, followed by towns and villages as well as kindergartens in individual towns/villages were randomly selected in each of the voivodships. Parents of children over or under the age of 5 years, those who did not consent to participate in the study, and the authors of incorrectly completed questionnaires, were excluded from the study. The sample size was estimated using the data from the Central Statistical Office (the population of children aged 5 years: 353,516) and data on the incidence of tooth decay as the leading health problem in Poland.
The parental questionnaire included questions about socioeconomic factors, as well as verified parental knowledge and health behaviours in relation to children’s oral health (hygiene, dietary, dental care, oral health-related quality of life) and a history of dental injuries in terms of the number of affected teeth, location of the tooth in the mouth, age at the time of injury, the mechanism of the injury, the scene of injury, and the treatment method used.
The study was approved by the Bioethics Committee of the Medical University of Warsaw (KB 185/2018). The data were analysed statistically. Comparisons of the study groups for quantitative variables were performed using parametric tests, i.e. the t-test for comparing two groups (e.g. gender) or the analysis of variance for more than two groups (e.g. provinces). Categorized variables were analysed using the chi-square test. For the tests performed, the results were presented as p-values, i.e. the observed significance levels (p < 0.05). Spearman correlation analysis was used to assess the relationships between the selected factors. SPSS and Statistica programme were used for analyses.
Results
The analysis included 1,044 correctly completed questionnaires, received from the parents of girls (51%) and boys (49%). The socioeconomic characteristics of respondents are presented in table 1.
Tab. 1. Socio-economic characteristics of the respondents
| | Total number of respondents n (%) |
| Total | 1044 (100%) |
| Gender | male | 512 (49%) |
| female | 532 (51%) |
| Place of residence | urban | 580 (55.6%) |
| rural | 464 (44.4%) |
| Maternal education level | elementary | 1 (0.1%) |
| vocational | 22 (2.1%) |
| secondary | 259 (24.8%) |
| postsecondary college or course | 125 (12%) |
| higher | 637 (61%) |
| Paternal education level | elementary | 7 (0.7%) |
| vocational | 41 (4%) |
| secondary | 374 (35.8%) |
| postsecondary college or course | 98 (9.4%) |
| higher | 524 (50.1%) |
| Self-assessed financial status of the family | unsatisfactory (poor) | 42 (4.02%) |
| average (good) | 68 (39%) |
| very good | 27 (59%) |
| Single parenthood | 84 (8%) |
| Use of dental care (dental appointment) | 670 (64.2%) |
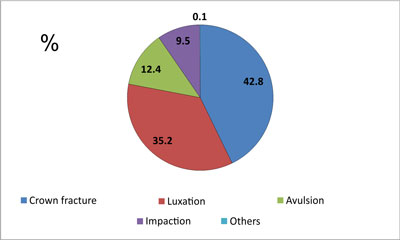
A total of 105 children (10.1%) had a history of primary tooth injury, most often in their third year of life (fig. 1). Usually, 1 tooth was injured (6.23% of injuries), the least frequently > 2 teeth (0.86% of injuries), in the anterior part of the maxilla (8.43% of injuries). Fracture of the tooth crown was the most common trauma (fig. 2). Tooth injury was accompanied by soft tissue damage in 48 children (45.7% of the reported cases of tooth trauma). These were usually lip or gum injuries. Falls (55.2%) and collisions/hitting an object (41.9%) were the main causes of injuries. Home (54.3%), backyard/playground (26.7%), kindergarten (10.5%), and street (8.6%) were the most common injury scenes.

Fig. 1. The incidence of primary tooth trauma in four age groups
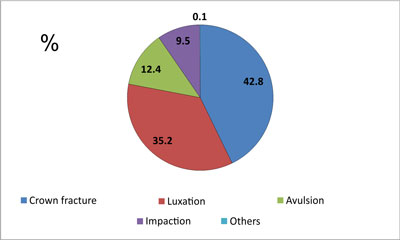
Fig. 2. Types of primary tooth trauma reported by parents
Powyżej zamieściliśmy fragment artykułu, do którego możesz uzyskać pełny dostęp.
Mam kod dostępu
- Aby uzyskać płatny dostęp do pełnej treści powyższego artykułu albo wszystkich artykułów (w zależności od wybranej opcji), należy wprowadzić kod.
- Wprowadzając kod, akceptują Państwo treść Regulaminu oraz potwierdzają zapoznanie się z nim.
- Aby kupić kod proszę skorzystać z jednej z poniższych opcji.
Opcja #1
24 zł
Wybieram
- dostęp do tego artykułu
- dostęp na 7 dni
uzyskany kod musi być wprowadzony na stronie artykułu, do którego został wykupiony
Opcja #2
59 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 30 dni
- najpopularniejsza opcja
Opcja #3
119 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 90 dni
- oszczędzasz 28 zł
Piśmiennictwo
1. Petti S, Glendor U, Andersson L: World traumatic dental injury prevalence and incidence, a meta-analysis. One billion living people have had traumatic dental injuries. Dent Traumatol 2018; 34: 71-86.
2. Ligali TO, Folayan MO, Sheiham A: Assessment of time taken to treat dental trauma in Nigerian children. Eur Arch Paediatr Dent 2011; 12: 37-40.
3. Szufnara A, Lipczyn?ska-Lewandowska M, Majewska-Bes?ka S, Szczepańska J: Ocena wiedzy nauczycieli oraz personelu medycznego na temat udzielania pierwszej pomocy w przypadkach urazów ze?bów. Nowa Stomatol 2018; 23(4): 135-141.
4. Holan G: Long-term effect of different treatment modalities for traumatized primary incisors presenting dark coronal discoloration with no other sign of injury. Dent Traumatol 2006; 22: 14-17.
5. Olczak-Kowalczyk D, Lipiec M: Uszkodzenia urazowe ze?bów mlecznych na podstawie badan? ankietowych rodziców/opiekunów prawnych dzieci w wieku 5 lat. [W:] Monitorowanie stanu zdrowia jamy ustnej populacji polskiej w latach 2016-2020. Uwarunkowania stanu zdrowia jamy ustnej i uszkodzenia urazowe zębów u dzieci i młodzieży w Polsce w 2020 roku. Sekcja Druków Uczelnianych Warszawskiego Uniwersytetu Medycznego, Warszawa 2021: 239-248.
6. Borum MK, Andreasen JO: Therapeutic and economic implications of traumatic dental injuries in Denmark: an estimate based on 7549 patients treated at a major trauma centre. Int J Paediatr Dent 2001; 11: 249-258.
7. Porritt JM, Rodd HD, Ruth BS: Quality of life impacts following childhood dento-alveolar trauma. Dent Traumatol 2011; 27: 2-9.
8. Locker D: Self-reported dental and oral injuries in a population of adults aged 18-50 years. Dent Traumatol 2007; 23: 291-296.
9. Petersson EE, Andersson L, Sorensen S: Traumatic oral vs non-oral injuries. Swed Dent J 1997; 21: 55-68.
10. Lam R: Epidemiology and outcomes of traumatic dental injuries: a review of the literature. Aust Dent J 2016; 61(1 Suppl): 4-20.
11. Granville-Garcia AF, de Menezes VA, de Lira PI: Dental trauma and associated factors in Brazilian preschoolers. Dent Traumatol 2006; 22: 318-322.
12. Oliveira LB, Marcenes W, Ardenghi TM et al.: Traumatic dental injuries and associated factors among Brazilian preschool children. Dent Traumatol 2007; 23: 76-81.
13. Otuyemi OD, Segun-Ojo IO, Adegboye AA: Traumatic anterior dental injuries in Nigerian preschool children. East Afr Med J 1996; 73: 604-606.
14. Choi SC, Park JH, Pae A, Kim JR: Retrospective study on traumatic dental injuries in preschool children at Kyung Hee Dental Hospital, Seoul, South Korea. Dent Traumatol 2010; 26: 70-75.
15. Szewczak K: Formy spędzania czasu wolnego przez dzieci klas trzecich szkoły podstawowej – raport z badań. Edukacja Elementarna w Teorii i Praktyce 2015; 1(35): 47-71.
16. Hasan AA, Qudeimat MA, Andersson L: Prevalence of traumatic dental injuries in preschool children in Kuwait- a screening study. Dental Traumatol 2010; 26: 346-350.
17. Gabris K, Tarjan I, Rozsa N: Dental trauma in children presenting for treatment at the Department of Dentistry for Children and Orthodontics, Budapest, 1985-99. Dent Traumatol 2001; 17: 103-108.
18. Osuji OO: Traumatised primary teeth in Nigerian children attending University Hospital: the consequences of delays in seeking treatment. Int Dent J 1996; 46: 165-170.
19. Glendor U, Halling A, Andersson L, Eilert-Petersson E: Incidence of traumatic tooth injuries in children and adolescents in the county of Västmanland, Sweden. Swed Dent J 1996; 20: 15-28.
20. Kahabuka FK, Plasschaert A, Van’t Hof M: Prevalence of teeth with untreated dental trauma among nursery and primary school pupils in Dar es Salaam, Tanzania. Dent Traumatol 2001; 17: 109-113.
21. Borum MK, Andreasen JO: Sequelae of trauma to primary maxillary incisors. Part I. Complications in the primary dentition. Endod Dent Traumatol 1998; 14: 31-44.
22. Kahabuka FK, Willemsen W, Van’t Hof M et al.: Initial treatment of traumatic dental injuries by dental practitioners. Endod Dent Traumatol 1998; 14: 206-209.
23. Merkle A: Complete intrusion of a maxillary right primary central incisor. Pediatr Dent 2000; 22: 151-152.
24. Ram D, Holan G: Partial pulpotomy in a traumatized primary incisor with pulp exposure: case report. Pediatr Dent 1994; 16: 44-48.
25. Cunha RF, Pugliesi DM, Mello Vieira AE: Oral trauma in Brazilian patients aged 0-3 years. Dent Traumatol 2001; 17: 210-212.
26. Llarena del Rosario ME, Acosta AV, Garcia-Godoy F: Traumatic injuries to primary teeth in Mexico City children. Endod Dent Traumatol 1992; 8: 213-214.
27. Fried I, Erickson P: Anterior tooth trauma in the primary dentition. Incidence, classification, treatment methods, and sequelae: a review of the literature. ASDC J Dent Child 1995; 62: 256-261.
28. Nelson LP, Shusterman S: Emergency management of oral trauma in children. Curr Opin Pediatr 1997; 9: 242-245.
29. Yam AA, Diop F, Faye M et al.: Complications of injuries to the deciduous teeth. Clinical and radiographic evaluation: perspectives on management and prevention (apropos 4 cases). Odontostomatol Trop 2000; 23: 5-9.
30. Glendor U: On dental trauma in children and adolescents. Incidence, risk, treatment, time and costs. Swed Dent J Suppl 2000; 140: 1-52.
31. Mestrinho HD, Bezerra AC, Carvalho JC: Traumatic dental injuries in Brazilian pre-school children. Braz Dent J 1998; 9: 101-104.
32. Garcia-Godoy F, Garcia-Godoy F, Garcia-Godoy FM: Primary teeth traumatic injuries at a private pediatric dental center. Endod Dent Traumatol 1987; 3: 126-129.
33. Bastone EB, Freer TJ, McNamara JR: Epidemiology of dental trauma: a review of the literature. Aust Dent J 2000; 45: 2-9.
34. Rai SB, Munshi AK: Traumatic injuries to the anterior teeth among South Kanara school children – a prevalence study. J Indian Soc Pedod Prev Dent 1998; 16: 44-51.
35. Fried I, Erickson P, Schwartz S, Keenan K: Subluxation injuries of maxillary primary anterior teeth: epidemiology and prognosis of 207 traumatized teeth. Pediatr Dent 1996; 18: 145-151.
36. Wilson S, Smith GA, Preisch J, Casamassimo PS: Epidemiology of dental trauma treated in an urban pediatric emergency department. Pediatr Emerg Care 1997; 13: 12-15.
37. Onetto JE, Flores MT, Garbarino ML: Dental trauma in children and adolescents in Valparaiso. Chile Endod Dent Traumatol 1994; 10: 223-227.
38. Fleming P, Gregg TA, Saunders ID: Analysis of an emergency dental service provided at a children’s hospital. Int J Paediatr Dent 1991; 1: 25-30.
39. Perez R, Berkowitz R, McIlveen L, Forrester D: Dental trauma in children: a survey. Endod Dent Traumatol 1991; 7: 212-213.
40. Soporowski NJ, Allred EN, Needleman HL: Luxation injuries of primary anterior teeth – prognosis and related correlates. Pediatr Dent 1994; 16: 96-101.
41. Nicolau B, Marcenes W, Sheiham A: The relationship between traumatic dental injuries and adolescent’s development along the life course. Community Dent Oral Epidemiol 2003; 31: 306-313.
42. Hamilton FA, Hill FJ, Holloway PJ: An investigation of dento-alveolar trauma and its treatment in an adolescent population – part 1: the prevalence and incidence of injuries and the extent and adequacy of treatment received. Br Dent J 1997; 182: 91-95.
43. Williams S, Matejka JM: Trauma to primary teeth of South African pre-school children. Endod Dent Traumatol 1999; 15: 73-76.
44. Zadik D: A survey of traumatized primary anterior teeth in Jerusalem preschool children. Community Dent Oral Epidemiol 1976; 4: 149-151.
45. Reddy KVKK, Kumar KN, Venkatasubramanian R et al.: Incidence of traumatic injuries in children aged 3-18 years in Tirupathi. Int J Pedod Rehabil 2017; 2(2): 73-76.