© Borgis - New Medicine 1/2003, s. 2-4
Zofia Rajtar-Leontiew1, Andrzej Koczyński2
Can purulent bacterial osteomyelitis (osteitis with arthritis) develop during foetal life?
1 Department of Newborn Pathology
Head: Zofia Rajtar-Leontiew MD, PhD
2 Department of Radiology and Ultrasonography, Clinical Hospital, the Medical University of Warsaw
Head: Andrzej Koczyński MD
Summary
The authors pose the question whether purulent bacterial osteomyelitis may originate during foetal life and develop later in the neonate. They present two cases with the disease and discuss the problems and practical implications.
Purulent bacterial osteitis with arthritis in newborns is an acute blood borne disease (1). It has a long-established and identified clinical course, including ultrasound and radiological pictures, showing a distinct change in blood supply and bone structure in this period of life (2). Early diagnosis of osteitis and of its aetiology is very important to allow the introduction of proper treatment and limitation of negative con-sequences, which will quite often include a severe handicap. Osteitis in a newborn may be suggested by symptoms such as: restlessness, abnormal positioning of the extremity, crying associated with movement (both active and passive), pain reactions, oedema and increased warmth in the involved area and sometimes redness. Ultrasound investigation of the bone and joint performed at this stage shows oedema of the soft tissues and joint effusion – usually gradually increasing. Bone and cartilage do not show destructive lesions during the early days when infection is being localised, present data suggesting that such lesions develop after at least 7 or even 10 days from disease commencement (3, 4,5). Thus, diagnosis of osteitis with its associated destruction and/or pathological joint dislocation during the first 3 days of newborn life, seen in the two cases which we have observed, must arouse suspicion that the mentioned pathological changes originated during the foetal period. For this reason they could have been detected at an early phase and identified by x-ray scan. Bacterial infection can cross from mother to child through the placenta into the foetal capillaries or can spread via an ascending route from the cervix. Bacterial intrauterine infections described to date include septicaemia, pneumonia, meningitis, conjunctivitis, osteitis and cartilage infection as a component of congenital syphilis. We have not found anyone describing purulent intrauterine osteitis and arthritis, which would show distinctive changes on x-ray examination by the second or third day of life.
These two cases of intrauterine osteitis and arthritis which we describe appear to be the first reports of such a condition.
Case 1. B.S. Hospital case number 1553/56/02.
Child born at term to mother pregnant for the second time, birth weight 3430g, Apgar 10. Oedema and redness of the right knee joint was found on the second day of life, associated with pain on movement, together with parallel purulent conjunctivitis. The results of laboratory tests suggested the presence of an inflammatory reaction. CRP was 103 mg%, ASPAT 113U/L, ALAT 70 U/L, WBC 15 700, sedimentation rate 5/h. WBC pattern bands 2, neutrophils 22, segments 50, eosinophils 1, monocytes 3, lymphocytes 22. Ultrasound investigation suggested an inflammatory process of bone and cartilage [osteitis and arthritis], and an x-ray scan performed on the second day of life already showed an area of diffuse bone structure within the distal epiphysis of the femur – i.e. a pattern characteristic of the later stages of this disease. The aetiology of the inflammation was confirmed by bacterial culture – Streptococcus agalactiae was detected in both the newborn´s blood and in the mother´s vagina. The course of the disease was complicated by coagulation system disturbances. The treatment was selected as a result of the bacterial tests. The further course of the disease and resulting radiological changes were in accordance with expectations based on the location of the infection. During the third week (18th day of life) a distinctive periostal reaction [callus formation] was found in both the right proximal and distal femoral epiphyses. After another 3 weeks of treatment there was significant regression of inflammatory lesions, seen with both ultrasound and radiological examinations. Hospitali-sation and treatment continued till the 6th week of life. After discharge the infant was transferred to outpatient care.
Case 2. K.S. Hospital case number 1726/84/01/F and 53529/01/Ch.
Child born to mother from 5th pregnancy delivered by caesarean section (previous 3 births also by cae-sarean section). Birth weight 4100g, length 56 cm, Apgar 10. Referred to our clinic at the beginning of the 3rd day of life, diagnosed dislocation of left elbow joint. On admission, oedema and cyanosis of the joint area were found with associated restriction of movement and related pain. Surgeon performed repositioning based on physical examination and an x-ray obtained on the 3rd day of life, and applied a soft immobilising dressing. After 2days (on 5th day of life) a follow-up x-ray revealed the failure of the repositioning manoeuvre, involving splinting of the fragment of the left distal humeral epiphysis and asymmetry of the cartilaginous area of the elbow joint. Laboratory test results pointed to an ongoing inflammatory process, CRP value was 309mg%, WBC 16 800, alkaline phosphatase 259 U/L, ASPAT 45, ALAT 51 U/L, OB4/h.
Having diagnosed osteitis of the distal epiphysis of the humerus and arthritis of the left elbow, complicated by a pathological dislocation found as early as the 3rd day of life, antibiotics were introduced. Cultures of blood and of fluid from the joint were negative. The further course of the disease showed a characteristic lesion i.e. callus formation by the 24th day of life and gradual renewal of the left distal humeral epiphysis with significant thickening along the whole axis was typical of osteitis and arthritis. Treatment and hospitalisation lasted for 9 weeks. Disturbances of the shape of the humerus did not influence anatomical positioning within the left elbow joint.
Parallel to the changes described above regarding the humerus and left elbow joint, paralysis of the left brachial plexus, congenital deformation of the cranial bones, and on the 4
th day of life a short episode of convulsions were observed. Urine culture showed a significant bacterial count of
E. coli species – 10
6. Serum antibodies against TORCH were absent. On discharge from hospital in the 10
th week of life the child was transferred into multidisciplinary care, involving physiotherapist, surgeon and neurologist.
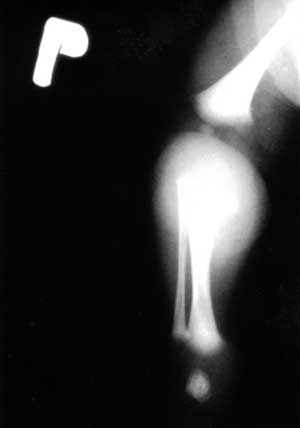
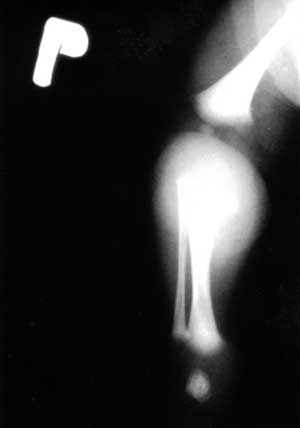
Fig. 1. Swelling of the soft tissues in the tibial upper part.

Fig. 2. Discreet lateralisation of the right femur with elongation of the Shenton-Menard line.

Fig. 3. Osseous notchings within the distal metaphysis of the right femur.

Fig. 4. Osseous reconstruction in metaphyseal parts of long bones within the right knee, with laminar periosteal reaction of the right tibial diaphysis.
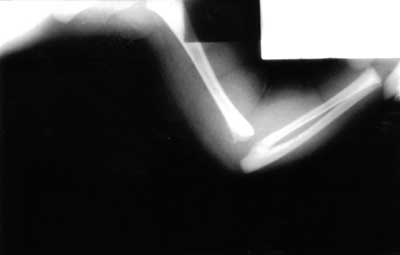
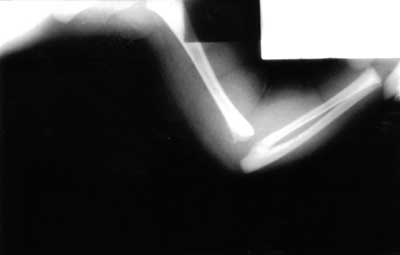
Fig. 5. Swelling of the soft tissues around the left elbow joint with intra-articular dislocation of forarm bones.

Fig. 6. A huge periosteal reaction with callus in the distal metaphyseal part of the left humerus, with marked thickening of adjacent soft tissues.

Fig. 7. The left humerus two weeks later – picture compared to fig. 2. The periosteal reaction is more condensed and osseous pattern of the metaphysis is reconstructed.

Fig. 8. A comparable picture to fig. 3 after three weeks: marked signs of osseous rebuilding and remodelling of the bone.
Conclusions
1.Radiological lesions visible on the 2nd or 3rd day of life, characteristic of late stage of osteitis, can suggest that the process already started a few or even several days earlier, i.e. in the foetus in utero.
2.The presented data are our own original observations and may have practical significance.
3.These observations require confirmation through further investigations involving a larger group of newborns with osteitis and arthritis diagnosed during the first days of life.
Piśmiennictwo
1. Dobrzańska A. et al.: Krwiopochodne zapalenie kości i stawów u noworodków na podstawie własnego materiału. Pediatria Polska 2000, 12:447-453. 2. Konarska Z. et al.: Septic coxitis during the neonatal period: the diagnosis and therapy of early-stage osteitis and arthritis. New Medicine 2001, 4, 1:10-11. 3. Banhoeffer J. et al.: Diagnosis of acute haematogenous osteomyelitis and septic arthritis: 20 years experience at the University Children´s Hospital, Basel. Swiss Med. WKLY, 2001, 131:575-581. www.smw.ch. 4. Merino Arribas J. et al.: Acute osteomyelitis. Clinical, radiological and bacteriological features and outcome. An. Esp. Pediatr. 2001, 55 (1):20-4. 5. Aroojis A.J., Ashok N. Johari: Epiphyseal Separations after Neonatal Osteomyelitis and septic arthritis. J. Pediatr. Orthop. 2000, 20:544-549.
Pozostałe artykuły z numeru 1/2003: