This boy was born after uncomplicated pregnancy and delivery. There was no evidence of respiratory distress but because of a small thorax skeletal survey was performed and the diagnosis of ATD established on the basis of chest and pelvic X-rays (Fig 1.A&B).
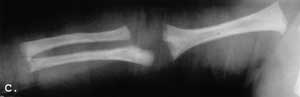
Fig. 1. A-C. A&B Newborn. A. Small thorax slightly narrowed in the upper part. Short, anteriorly widened ribs; B. Flat, triradiate acetabula. Short, bowed femora with widened ends. Advanced ossification of the capital femoral epiphyses; C. 3 year-old. Grossly normal chest.
At the age of 3 months he was admitted to the Mater Hospital in Brisbane with clinical features suggesting hepatomegaly. There was no evidence of chest problems. The routine blood and urine examinations and liver function tests were normal.
Ultrasound of the abdomen was normal. Hepatomegaly was spurious secondary to small thorax. Radiograph of the chest taken at the age of 3 years grossly normal (Fig 1.C).
An older sister is also affected with similar, moderate, asymptomatic from of the disease.
This girl was born after normal pregnancy and delivery. Birth weight was 3560g. Her thorax was small and narrow. Severe respiratory distress was present immediately after birth. She was admitted to intensive care unit died at the age of 5 days.
Radiographic examination on the second day of life documented narrow, rectangular chest charakteristic pelvis and upper limb changes (Fig 2. A-C).
Bone biopsy disclosed changes consistent with ATD.


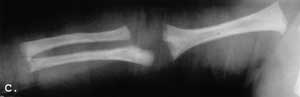
Fig. 2. A-C. Newborn. A. Narrow, rectangular chest, short anteriorly widened ribs; B. Flat, triradiate acetabula; C. Slightly dysplastic long bones. Cupped distal ends of the forearm bones. Irregular distal humeral mataphysis.
Discussion
Both our patients presented with a small thorax. Patient 1 had an asymptomatic clinical course, whereas Patient 2 with smaller and narrower thorax succumbed to respiratory insufficiency after the first few days of life. The size and shape of the thorax is probably an important prognostic sing.
The differential diagnosis of ATD is with chondro-ectodermal dysplasia, Barnes syndrome, short rib polydactyly syndromes, neonatal Shwachman syn-drome and localised chest dysplasias.
Major clinical signs of chondroectodermal
dysplasia are hexodaxtyly, ectodermal dysplasia and cardiac defects. Deformity of the tibia and hamate-capitate bone fusion are major radiographic signs (7). Some authors presume that ATD, chondroectodermal dysplasia and renal-hepatic-pancreatic dysplasia from part of a disease spectrum rather than being distinct con-ditions(2).
Barnes syndrome – thoraco-laryngo-pelvic dysplasia – is characterised by small thorax, small pelvis and laryngeal stenosis. The appearances of the pelvis are different form ATD and the hands are normal (8).
Thoraco-pelvic dysplasia shows close resemblance in the appearance of chest and pelvis to Barnes syndrome but there is no laryngeal stenosis (8).
Short rib polydactydy syndromes are characterized by more severe chest narrowing and severly dysplastic long bones. Still birth or early fatal outcome is the usual clinical course (1,2).
Shwachman syndrome may present at birth with respiratory distress and thorax. Although radiographic apperances of the chest may be confusing, normal pelvis X-rays exclude ATD and Barnes syndrome. Long bones in Shwachman syndrome may show some metaphyseal cupping, which may cause confusion with neonatal rickets (9).
Localised chest dysplasias do not show any other bony abnormalities (10).
Small thorax is a common feature of many bone dysplasias. Other clinical and radiographic characteristics allow easy confirmation or elimination of ATD.
Ultrasound examination about 18-20 weeks of pregnancy can establish prenatal diagnosis of ATD (11).
Piśmiennictwo
1. Bernstein R. et al.: Short rib-polydactyly syndrome: a single or heterogeneous entity? A re-evaluation prompted by four new cases. J. Med. Genet. 1985; 22:46-53. 2. Brueton L.A. et al.: Ellis-van Creveld syndrome, Jeune syndrome, and renal-hepatic-pancreatic dysplasia: separate entities or disease spectrum? 3. Franceschini A. et al.: Short rib-dysplasia group (with/without polydactyly): report of a patient suggesting the existence of continuous spectrum. Am. J. Med. Genet. 1995; 59:359-364. 4. Jequier J.C.: La dystrophie thoracique asphyxiante. Arch. Fr. Ped. 1970; 27:177-193. 5. Jeune M. et al.: Dystrophie thoracique asphyxiante de caractere familial. Arch. Fr. Ped. 1955; 12:886-891. 6. Kozlowski K., Masel J.: Asphyxiating thoracic dystrophy withhout respiratory disease. Report of two casses of the latent from. Ped. Radiol. 1976; 5:30-33. 7. Kozlowski K. et al.: Difficulties in differentiation between chondroectodermal dysplasia (Ellis-van Creveld syndrome) and asphyxiating thoracis dystrophy. Aust. Radiol. 1972; 16:401-410. 8. Marik I. et al.: Thoracic-plevic dysostosis. Clin. Dysmorph. 2000; 9:1-3. 9. Michels V.V., Donovan K.: Shwachman syndrome: unusual presentation as asphyxiating thoracis dystrophy. Brith Defects 1982; 18, 3B:129-134. 10. Rabushka S., Kadison H.I.: Isolated thoracic dysostosis. Radiology 1972; 106:161-165. 11. Schinzel A. et al.: Prenatal sonographic diagnosis of Jeune syndrome. Radiology 1975; 154:777-778.