© Borgis - New Medicine 3/2011, s. 79-83
*Tomasz Miłek1, Piotr Ciostek1, Witold Wożniak1, Andrzej Lewczuk1, Robert Petryka2, Jakub Słowik2, Mirosław Jarosz2
Preliminary results of the use of self-expanding nitinol stents in inoperable gastrointestinal cancers
1First Chair and Department of General and Vascular Surgery of the Warsaw Medical University Department
Head: Prof. Piotr Ciostek, MD, PhD
2Gastrology Department of the Food and Nutrition Institute in Warsaw Department
Head: Prof. Mirosław Jarosz, MD, PhD
Summary
Aim. The aim of the study was to present preliminary results of the palliative treatment of strictures and obstruction of the gastrointestinal tract in stage IV cancers with the use of self-expanding stents.
Material and methods. Within a one-year period, from October 2008 to September 2009, stent implantation in the gastrointestinal tract was performed in 32 patients. Eligibility for palliative treatment was determined on the basis of a clinical examination and diagnostic tests to assess cancer stage. Local advancement of cancer with infiltration of other tissues, such as metastases to the liver, distant lymph nodes or other organs, determined the choice of palliative treatment. The procedures were performed using a c-arm X-ray system and endoscope.
Results. A total of 33 stents were implanted in 32 patients. Problems with stent placement occurred in one patient. During implantation into a stricture secondary to sigmoid colon cancer, the stent slipped down and incompletely filled the tumor lumen. In this case, a short supplementary stent was added, which yielded a satisfactory result of the procedure. In another case, the stent migrated and adhered to the gastric wall, which further impaired passage through the patient′s gastrointestinal tract.
Conclusions. 1) Stent implantation in the gastrointestinal tract lumen in the setting of inoperable carcinomas under endoscopic and X-ray control is effective and safe. 2) In the case of gastrointestinal tract obstruction in patients with left colon cancers and in poor general condition, this procedure should be considered prior to pursuing surgical operations.
Introduction
Along with an increase in incidence of gastrointestinal cancers, there is a growing need for optimisation of surgical management, at best with the use of minimally invasive treatment methods. Unfortunately, advanced and/or obstruction-complicated forms predominate among newly diagnosed gastrointestinal cancer cases. These patients are of particular concern due to the poor results of treatment in this group obtained so far. The recently introduced self-expanding stents implanted into the gastrointestinal tract lumen seem to offer new possibilities in palliative management. Their applications so far were limited to strictures in inoperable eosophageal, gastric and duodenal malignancies. There also have been recent attempts to use them in colonorectal cancer. Stent implantation is a minimally invasive technique. Owing to its use, operation can be avoided, which means the elimination of the risk of systemic and local complications, relatively common after typical operative treatment, or operation can be delayed by several weeks, using the time gained for preliminary anticancer treatment and improvement of the body functioning of the candidate for the procedure. Patients′ life comfort improves, which includes maintaining the possibility of feeding via the physiological oral route or stoma creation avoidance.
The following clinical situations are generally accepted indications for stent implantation:
1. The patient is non-eligible for classical surgical treatment in view of local and general advancement of cancer – stent placement resolves the problem of imminent obstruction and gives the chance for immediate initiation of systemic treatment.
2. The tumour is initially inoperable, as a result of which the patient is found eligible for neoadjuvant chemotherapy – stent use gives time to perform chemotherapy and a chance for a later curative operation.
3. The patient is found non-eligible for classical surgical treatment due to advanced coexisting disorders – the stent solves the problem of imminent obstruction and gives the chance for curing the patient and improving his/her performance, owing to which the patient′s general clinical condition may improve and operation eligibility may favourably change.
In view of the increasing experience of medical teams implanting stents, the indications for their use are more and more confidently extended. The direction which is highly likely to be extensively accepted by clinicians is the use of gastrointestinal stents in conditions of acute malignant obstruction. After endoscopic clearing of the obstruction, to fixate the distension and prevent re-obstruction of the intestinal lumen, a stent is placed at the cleared site. Another interesting indication for the use of stents, this time the so-called coated stents, is sealing of gastrointestinal fistulae, especially when reoperation seems to be technically difficult or unfeasible due to the patient′s poor general clinical condition resulting from undernourishment and electrolyte and protein loss through the fistula. In these cases, stent placement causes immediate sealing of the fistula and enables rapid elimination of the deficiencies via the physiological route (fig. 1, 2). Finally, a particular problem associated with stent use is relapsing cancerous strictures at the place of anastomosis after previous operations, caused by a local relapse. In these cases, when local relapse is associated with generalisation of the cancer process, it is indicated to use the endoscopic technique of widening the stricture and its fixation with the use of a stent. Minimally invasive restoration of gastrointestinal passage and a short hospitalisation enables immediate initiation of systemic treatment.

Fig. 1. Stent placement in sigmoid colon.

Fig. 2. Stent placement in lower esophagus.
aim of the Study
The aim of the study is to present the preliminary results of the palliative treatment of strictures and obstruction of the gastrointestinal tract in stage IV cancers, with the use of self-expanding stents.
Material and methodS
Within one year (an academic year was chosen for the illustration) of October 2007 to September 2008, stent implantation into the gastrointestinal tract was performed in 19 patients. Table 1 presents the anatomical location of cancer lesions, and the number and type of the procedures performed.
Table 1.
| Cancer location | Patient No | Procedure |
Oesophagus
Cardia
Pylorus
Pylorus with duodenal infiltration
Descending colon
Sigmoid colon
Rectosigmoid bend
Oesophagogastric fistula
(anastomoses after gastric resection)
Total | 5
4
1
1
2
2
2
1
1
19 | Widening, stent
Widening, stent
Widening, stent
Stent
Clearing, stent,
Widening, stent
Clearing, widening, stent
Coated stent
|
The operated patients included 12 men and 7 women aged 69-82 years (72 years on average). The decision on eligibility to palliative treatment was made on the basis of a clinical examination and diagnostic tests enabling the assessment of cancer advancement stage. Endoscopy with taking biopsy samples for histopathological examination and abdomen and chest CT scans were performed. The choice of palliative treatment was determined by high local advancement of cancer with infiltration of other organs and signs of process generalisation such as metastases to the liver, distant lymph nodes or other organs. Moreover, the presence and severity of coexisting disorders were thoroughly determined. Each patient was assessed on the Karnofsky performance scale. The condition for eligibility, except for emergency conditions, was performance status below 70. An obvious indication for local palliative treatment was severe insufficiency of the cardiovascular and respiratory systems, usually associated with post-infarction damage to the myocardium, COPD, diabetes mellitus, renal insufficiency.
The procedures were performed with the use of a c-arm X-ray machine and endoscope. After endoscope introduction to the area of cancerous narrowing, a guide tube was inserted through the stricture with fluoroscopic control. In the case of obstruction, preliminary clearing and decompression of the stricture site with dilators were performed. Then, after introduction of balloon catheters through the guide tube, the balloons were gradually filled with dilation of the strictures to a diameter enabling insertion of the stent set. Under double endoscopic and radiological control, after contrast administration above the narrowing, the stent expanding the stricture was released. The result of stent placement was documented by radiological photographs and the subsequent X-ray check of stent location was performed 48 hours after its implantation.
Results
Twenty stents were implanted in 19 patients. In all patients, the indication was metastatic gastrointestinal cancer and non-eligibility to an open surgical procedure.
Stents could be implanted in all patients planned for this procedure. Problems with stent placement occurred only in one patient. During implantation into a stricture due to sigmoid colon cancer, stent slipped down and incompletely filled up the tumour lumen. In this case, a short supplementary stent was added, which finally allowed obtaining a satisfactory result of the procedure.
The delayed results based on the follow-up of 8 to 20 months are as follows: 3 patients with stents implanted for cancerous obstruction of the oesophagus died at 3, 4 and 6 months of follow-up due to disease progression, with persisting patency of the gastrointestinal tract. Anterior resection removing the tumour and the stent was performed after neoadjuvant chemotherapy and regression of the lesions in one patient in whom a stent was implanted for sigmoid colon cancer. In the subsequent stage, the patient underwent ablation of metastatic lesions in the liver and currently still remains under surgical follow-up. In another patient, symptoms of obstruction of a stent implanted due to inoperable cardia carcinoma developed 6 months after stent implantation. The diagnostics revealed that the stent migrated and was propped against the gastric wall adhering to its tip, which additionally impaired the passage. Feeding jejunostomy was performed in this patient, in view of the patient′s extremely poor general condition. In the remaining 15 cases, the implanted stents remained patent, and 12 patients of this group underwent a course of chemotherapy. All patients are under the care of an oncological hospice or their families and undergo surgical follow-up examinations every 3 months. Summing up, in the technical aspect, stent placement into cancer strictures was successful in all cases and appeared to be effective with respect to maintaining gastrointestinal tract patency in 18 out of 19 patients.
Discussion
The use of self-expanding stents is more and more common in palliative treatment of gastrointestinal cancers (1). Good immediate results described in the literature but also those arising from our own experience encourage to further development of this method. In the case of oesophageal and gastric cardia tumours this procedure practically replaced invasive, operative implantation of oesophageal prostheses (fig. 3). A new indication for the procedure is the use of stents in advanced colonorectal cancers to prepare the patient to neoadjuvant treatment before the planned surgical procedure (fig. 4). It is a procedure preventing the occurrence of obstruction during relatively long systemic treatment (2). Due to technical difficulties, the transverse colon and the right part of the colon are practically inaccessible for this method of proceeding. Currently, studies are conducted on transcutaneous access to this part of the large bowel (3, 4).
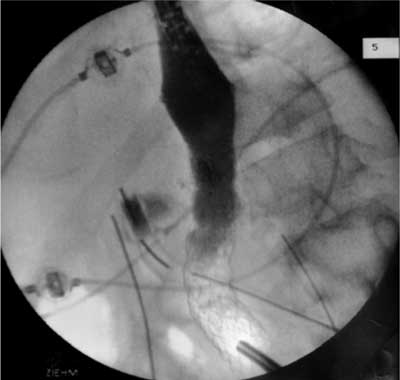
Fig. 3. Sealing of the fistula.

Fig. 4. Fistula.
Based on our experience and literature analysis, we may conclude that the safest method of placing stents within the gastrointestinal system is a technique using double imaging, i.e. the use of endoscopic viewing and radiological imaging during the operation (5, 6, 7). Double imaging allows appropriate placement of the stent and makes it possible to immediately detect complications during the procedure. The most common perioperative and early complications listed in the literature are stent migration occurring in 6-8% of the patients, tumour perforation in 4%, stent kinking and obstruction in 1-3%, bleeding in 1% of the operated patients (1-10).
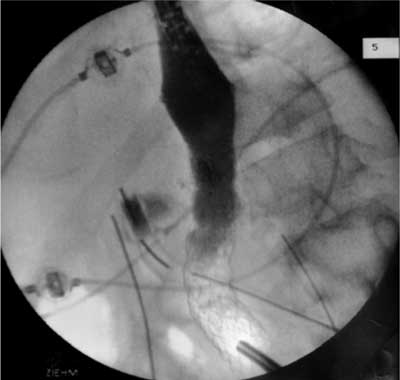
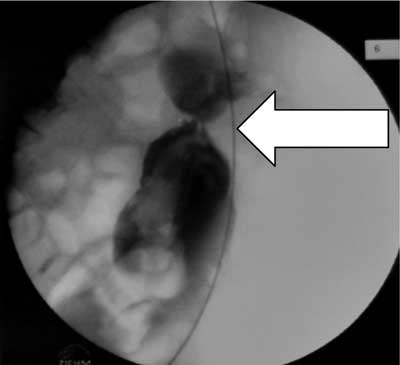
An interesting direction of the method development is the use of stents in emergency conditions such as gastrointestinal obstruction (11, 12, 13). Patients with a high surgical risk arising from an advanced cancer process and coexisting medical disorders can be found eligible for this method. In this manner patients avoid a necessary emergency operation, which is usually creation of an enterostomy. In the second stage, after general condition improvement is obtained, the patient can be operated or can undergo systemic treatment. In our material, we performed with a good effect two operations in patients with complete obstruction of the sigmoid colon. One patient was then subjected to elective surgery and the second patient was found eligible for systemic treatment (fig. 5, 6).
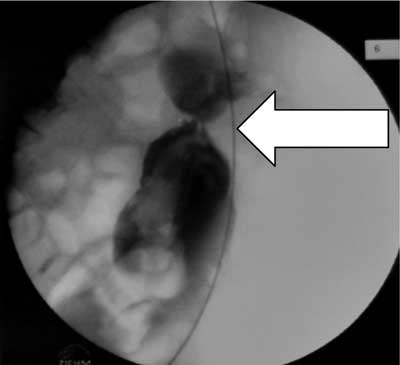
Fig. 5. Obstruction of descending colon.

Fig. 6. After stent placement in descending colon.
The immediate results and the results within up to 20 months of follow-up obtained by us are good, consistent with those described in the literature. They encourage to further development of the described treatment method. There are no studies which would directly compare the results of classical surgical treatment and the described method with the use of stents, but already the initial comparison of these methods demonstrates lower mortality, an incomparably lower number and importance of complications related to the procedure and a better perspective for further cancer treatment with the minimally invasive endoscopic method.
Conclusions
1. Stent implantation into the gastrointestinal tract lumen due to inoperative carcinomas under endoscopic and X-ray control is effective and safe.
2. In the case of left colonic cancers in patients in poor general condition and of gastrointestinal tract subobstruction, this procedure should be considered first, before the potential surgical operation.
Piśmiennictwo
1. Brehant O, Fuks D, Bartoli E et al.: Elective (planned) colectomy in patients with colorectal obstruction after placement of a self-expanding metallic stent as a bridge to surgery: the results of a prospective study. Colorectal Dis 2008 May 9 (Epub ahead of print). 2. McLoughlin MT, Byrne MF: Endoscopic stenting: where are we now and where we go? World J Gastroenterol 2008; 14(24): 3738-803. 3. Trompetas V: Emergency management of malignant acute left-sided colonic obstruction. Ann R Coll Surg Engl 2008; 90(3): 181-6. 4. Liberman H, Adams DR, Blatchford GJ et al.: Clinical use of the self-expanding metallic stent in the management of colorectal cancer. 2000; 180, 6: 407-412. 5. Kim TH, Song HY, Park IK et al.: Usefulness of multifunctional gastrointestinal coil catheter for colorectal stent placement. Eur Radiol 2008 (Epub ahead of print). 6. Baerlocher MO, Asch MR, Vellahottam A et al.: Safety and efficacy of gastrointestinal stents in cancer patients at a community hospital. Can J Surg 2008; 51(2): 130-4. 7. van Hoft JE, Focken P, Marinelli AW et al.: Dutch Colorectal Stent Group: Early closure of a multicenter randomized clinical trial of endoscopic stenting versus surgery for stage IV left-aided colorectal cancer. Endoscopy 2008; 40(3): 184-91. 8. Vape P, Huhinen H, Rantala A et al.: Adoption of self-expanding metallic stents in the palliative treatment of obstructive colorectal cancer-look out for perforations. Surg Laparosc Endosc Percutan Tech 2008; 18(4): 353-6. 9. Gupta K, Freeman ML: Enteral and colonic self-expanding metallic stents. Rev Gastroenterol Disord 2008; 8(2): 83-97. 10. Dormann AJ, Deppe H, Wigginghaus B: Self-expanding metallic stents for continuous dilatation of benign stenoses in gastrointestinal tract – first results of long-term follow-up in interim stent application in pyloric and colonic obstructions. Gastroenterol 2001; 39: 957-960; DO1:10.1055/s-2001-18531. 11. Harris GJC, Senagore AJ, Lavery JC, Fazio VW: The management of neoplastic colorectal obstruction with colonic endolumental stenting devices. Am J Surg 2001; 181, 6: 499-506. 12. Kim H, Kim SH, CHoi SY et al.: Fluoroscopically Guided Placement of Self-Expandable Metallic Stents and Stent-Grafts in the Treatment of Acute Malignant Colorectal Obstruction. J Vasc Interv Radiol 2008; 7 (epub ahead of print). 13. Stenhouse GJ, Page B, McKelvi A et al.: Self expanding wall stents in malignant colorectal cancer; is complete obstruction a contraindication to stent placement? Colorectal Dis 2008; (epub ahead of print). 14. Lopes CV, Pesenti C, Bories E et al.: Self-expandable metallic stents for palliative treatment of digestive cancer. J Clin Gastroenterol 2008; 42(9): 991-6. 15. Gomez Herrero H, Paul Diaz L, Pinto Pabon I, Lobato Fernandez R: Cardiovasc Intervent Radiol 2001; 24(1): 67-9. 16. Ernst S, Stippel D, Lackner K: Placement of palmaz stent in malignant duodenal stenosis through a cutaneous fistula. Eur Radiol 1999; 9(6): 1142-4. 17. Keymling M, Wagner HJ, Vakil N, Knyrim K: Relief of malignant duodenal obstruction by percutaneous insertion of a metal stent. Castrointestinal Endoscopy 1993; 39: 439-441.