© Borgis - New Medicine 3/2011, s. 90-92
Małgorzata Kołodziejczak1, *Iwona Sudoł-Szopińska2, Paweł Grochowicz1, Krzysztof Wagiel1
Utility of fistulography in diagnosing a post-traumatic rectal fistula – a case report
1Proctology Department, Hospital at Solec, Poland
Head of Department: dr hab. med. Małgorzata Kołodziejczak
2Department of Diagnostic Imaging, Institute of Rheumatology and Department of Diagnostic Imaging, Medical University of Warsaw, Poland
Head of Department: prof. dr hab. med. Iwona Sudoł-Szopińska
Summary
Background. Classical fistulography in most coloproctological centers has been replaced by anorectal ultrasound and magnetic resonance fistulography which are considered the „gold standards” in preoperative diagnosis of perianal fistulas. However, in case of a non-cryptogenic fistula, there still is a place for standard fistulography.
Aim. To present the role of standard fistulography in the preoperative assessment of a recurrent, post-traumatic fistula-in-ano.
Material and Methods. A 47-year-old man was admitted to the proctology department. Five years previously he had experienced an impalement injury to the perineum upon a ladder. At that time, the perineal wound was checked and the bleeding controlled. Since then he had been operated on four times due to recurrent anal fistulas. Anorectal ultrasound, followed by fistulography and computed tomography were performed.
Results. Anorectal ultrasound demonstrated an extrasphincteric fistula not communicating with the rectum. Fistulography revealed the fistula to be running parallel to the rectal wall, and confirmed the lack of an internal opening. Additionally, approximately 30 cm from the anal verge, the fistula came to an end with an outline of a non-contrasting foreign body. Computer tomography showed this foreign body to be located within the right iliopsoas muscle, with its lower margin against the right iliac artery. Laparotomy was performed, and a 10 cm long piece of wood was removed.
Conclusions. 1. In the preoperative diagnostics of a perirectal fistula, whose etiology is not cryptogenic, fistulography serves as an accurate yet simple, fast, and minimally-invasive diagnostic method. 2. Computer tomography allows for the precise localization of a foreign body with respect to its surrounding structures.
Introduction
The preoperative diagnostic algorithm for cyptogenic perirectal fistulas is generally known and accepted. Magnetic resonance imaging (MRI) and anorectal ultrasound (AUS) are considered the „gold standards” (1, 2). The use of multiplanar imaging, sequences like fat suppression, and contrast enhancement in MRI, plus three dimensional techniques with hydrogen peroxide enhancement in AUS, have made it possible to delineate primary and secondary fistulous tracts and fluid collections with respect to the external anal sphincter and puborectalis muscle, and identify the internal opening site (1, 3).
Herein we report a rare case of a post-traumatic fistula around a foreign body in the retroperitoneal space, which was diagnosed by classical anal fistulography – an imaging method considered by and large obsolete.
Case report
A 47-year-old man was admitted to the proctology department due to recurrence of an anal fistula. Five years previously he had experienced an impalement injury to the perineum upon a ladder. At that time, the perineal wound was checked and the bleeding controlled. Since then he had been operated on four times due to recurrent anal fistulas.
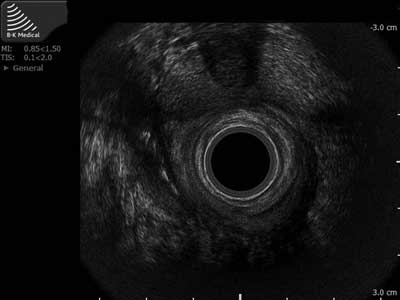
In the proctological examination, the active and passive tone of the sphincters was appropriate. On the right side, 2 cm from the anal verge the external opening of the fistula was localized. Anoscopy and rectoscopy did not reveal an internal opening of the fistula. The patients was sent for AUS, and was examined in the left lateral position using the BK Medical scanner, Profocus 2202, with a 2050 type 3D mechanical volumetric endoprobe of 6-16 MHz frequency. A suprasphincteric fistula without an internal opening was demonstrated (fig. 1).
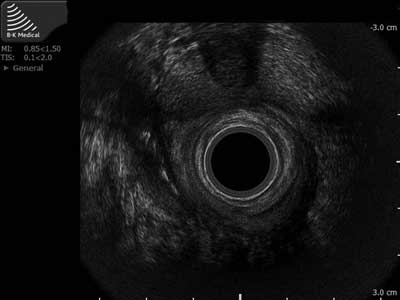
Fig. 1. Anorectal ultrasound demonstrates an extrasphincteric fistula in perirectal tissue, on the right side.
In order to confirm lack of communication with the rectum, fistulography was carried out after cannulating the external opening of the fistula with a narrow bore polythene catheter (with a metal marker strapped in place). Approximately 50 ml of uropolinum was injected and films were taken in the anteroposterior and lateral position. This imaging technique revealed the fistula to be running parallel to the rectal wall on the right side, towards the abdominal cavity, without evidence of communication with the rectum. Approximately 30 cm from the anal verge, the contrast delineated an outline of a 10 cm long foreign body in the abdominal cavity (fig. 2). Biphasic spiral computed tomography (CT) further showed it to be located within the right iliopsoas muscle, with its lower margin against the right iliac artery (fig. 3).

Fig. 2. Anal fistulography reveals a fistula running parallel to the rectal wall, towards the abdominal cavity, without evidence of communication with the rectum, and approximately 30 cm from the anal verge it shows an outline of a non-contrasting foreign body, 10cm in length.

Fig. 3. CT coronal reconstruction demonstrates a foreign body in the right iliopsoas muslce, with its lower margin against the right iliac artery.
Laparotomy was performed, and a 10 cm long piece of wood was removed from the right iliopsoas muscle (fig. 4). The patient was discharged home on the eighth day after operation, without signs or symptoms of the fistula.

Fig. 4. At surgery, the 10cm long piece of wood in the right iliopsoas muscle was identified.
Discussion
Fistula-in-ano has a significant recurrence rate up to 25%, largely due to missed secondary tracks or failure to identify the internal openings (4, 5). To maintain the recurrence rate as low as possible, the surgeon must understand the exact relationship of the fistula to the perianal anatomical structures and spaces. An accurate preoperative imaging method, one which delineates the primary and secondary tracks, the sites of the internal opening and pus collection, may help prevent recurrences and inadvertent sphincter injury (6). If recurrence of a fistula is suspected, such an imaging method may demonstrate clinically undetected sepsis, and reveal the site of residual sepsis (2).
Initial reports on the usefulness of fistulography in diagnosing recurrent anal fistulas were greatly optimistic, with detection rates of 84-96.3% (7). Results of subsequent works were very divergent. More disappointing articles presented a concordance of fistulography with intra-operative findings in only 16% of cases. While in 10% fistulography could falsely show internal openings to the rectum and high extensions; such misrepresentations could lead to perforations of the rectum and formation of iatrogenic fistulas in the course of the surgical procedures (4, 7-10). On this basis, fistulography was deemed inaccurate and unreliable (8). In other publications though, the sensitivity of fistulography in identifying the primary track of the fistula was found to be 83.3% (11) up to 100% (6, 12).
Thus it is not surprising that in recent years in the available literature, there have not been many publications about classical fistulography, which in most coloproctological centers has been replaced by AUS and MR fistulography. Aside from one case from 2008, in which the authors compared fistulography with AUS and detected a significant benefit of AUS over fistulography and clinical examination (10).
In comparison to MR and AUS, fistulography may be disappointing for several reasons. It is difficult to relate the primary tract to the external anal sphincter and levator ani muscles, as they are not visible in fistulography (2). Also, contrast may either spill onto the skin, causing an ambiguous image of the fistula, or it may rapidly reflux back into the rectum, suggesting an extrasphincteric tract with a rectal opening (2). Administration of the contrast often causes discomfort.
In spite of the largely critical stance of Bartram and Buchanan (2), these authors note that fistulography could be helpful in chronic, high perianal fistulas, having an external opening distant from the anus, and in confirming its communication with the rectum.
Anorectal ultrasound is a minimally invasive technique that provides detailed images of sphincter defects, anorectal sepsis and the course of the fistulous track (4-6,13,14); however, in the case of high perianal fistulas, it has limited utility. On the other hand, MRI has been reported to allow more accurate depiction and classification of fistula-in-ano than AUS, but is expensive and not available in many centers. Moreover, both AUS and MRI are unreliable in assessing the internal opening of a fistula (15, 16).
The case we have presented shows that in selected patients anal fistulography may provide useful information for the definitive management of fistula-in-ano. A similar conclusion was drawn by Weisman and Orsay, who in 1991 presented a retrospective review of 27 patients undergoing anal fistulography, including 1 patient with an iatrogenic fistula and 1 case of a fistula due to perforation by a foreign body (7). In 48% of their patients, data obtained from the fistulogram revealed either an unexpected pathology or directly altered surgical management. This had also been the case with our patient, in whom fistulography showed the course of the recurrent fistula, its cause, and indicated a lack of communication with the rectum. AUS proved to be useless, being unable to ascertain the retorperitoneal space. Thus the results of fistulography determined the type of surgical approach used (laparotomy), while the addition of spiral CT allowed for safe removal of the foreign body.
Piśmiennictwo
1. Sun MR, Smith MP, Kane RA: Current techniques in imaging of fistula in ano: three-dimensional endoanal ultrasound and magnetic resonance imaging. Semin Ultrasound CT MR 2008; 29: 454-71. 2. Bartram C, Buchanan G: Imaging anal fistula. Radiol Clin N Am 2003; 41: 443-457. 3. Zbar AP, Armitage NC: Complex perirectal sepsis: clinical classification and imaging. Tech Coloproctol 2006; 10: 83-93. 4. Seow-Choen F, Nicholls RJ: Anal fistula. Br J Surg 1992; 79: 197-205. 5. Law PJ, Bartram CI: Anal Endosonography: Technique and normal anatomy. Gastrointestinal Radiol 1989; 14: 349-535. 6. Elangovan S, Bhuvaneswary V, Nadarajan S, Kannan RR, Velmurugan S: Comparative study of fistulography and anal endosonography in fistula-in-ano. Indian J Radiol Imaging 2002; 12: 343-6. 7. Weisman RI, Orsay CP, Pearl RK, Abcarian H: The role of fistulography in fistula-in-ano. Dis Colon Rectum 1991; 34: 181-184. 8. Kuijpers HC, Schulpen T: Fistulography for fistulo-in-ano. Dis Colon Rectum 1985; 28: 103-104. 9. Halligan S: Review: imaging fistula-in-ano. Clinical Radiol 1998; 53: 85-95. 10. Tapes B, Cerni I: The use of different diagnostic modalities in diagnosing fistula-in-ano. Hepatogastroenterology 2008; 55: 912-5. 11. Pomarri F, Pittarello F, Dodi G, Pianon P, Muzzio PC: Radiologic diagnosis of anal fistulae with radio-opaque markers. Radiol Med 1988; 75: 632-7. 12. Pomerri F, Dodi G, Pintacuda G et al.: Anal endosonography nas fistulography for fistula-in-ano. Radiol Med 2010; 22 [Epub ahead of print] 13. Choen S, Burnett S, Bartram CI, Nicholls RJ: Comparison between anal endosonography and digital examination in the evaluation of anal fistulae. Br J Surg 1991; 78: 445-447. 14. Law PJ, Talbot RW, Bartram CI, Northover JMA: Anal endosonography in the evaluation of perianal sepsis and fistula in ano. Br J Surg 1989; 76: 752-755. 15. Shahid M Hussain, Stoker J, Schouter WR et al.: Fistula-in-ano: Endoanal sonography versus endoanal MR Imaging in classification: Radiology 1996; 200: 475-481. 16. Cho DY: Endosoniographic criteria for an internal opening of fistula-in-ano. Dis Colon Rectum 1999; 42: 515-518. 17. Lunnis PJ, Barker PG, Sultan AH: Magnetic resonance imaging of fistula-in-ano. Dis Colon Rectum 1994; 37: 708-718.