Agata Wasilewska, *Lidia Zawadzka-Głos
Bilateral antrochoanal polyp: case report, literature review and clinical guidelines
Obustronny polip choanalny – opis przypadku. Przegląd literatury
Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Lidia Zawadzka-Głos, MD, PhD
Streszczenie
Polip choanalny jest łagodną zmianą zapalną zatok przynosowych. Wywodzi się w większości przypadków z błony śluzowej zatoki szczękowej, wychodząc zwykle przez ujście dodatkowe zatoki, a stąd sięga do nozdrzy tylnych i nosogardła.
Celem pracy jest przedstawienie charakterystyki klinicznej i leczenia polipów choanalnych (ACP) oraz przedstawienie bardzo rzadkiego przypadku pacjentki z obustronnym polipem choanalnym i dużą tendencja do nawrotów dolegliwości.
Polipy choanalne stanowią około 1/3 wszystkich polipów zatok przynosowych u dzieci, większość z nich występuje jednostronnie. U dzieci obserwuje się także większą częstość nawrotów niż u dorosłych. Zmiana wymaga diagnostyki różnicowej ze zmianami nowotworowymi.
Leczenie jest operacyjne. Złotym standardem jest endoskopowa operacja zatok. Obejmuje ona usunięcie masy polipa z nozdrzy tylnych, endoskopowe poszerzenie ujścia zatoki szczękowej i usuniecie zmian polipowatych i przyczepu polipa z jej wnętrza.
Obserwacja pooperacyjna musi być prowadzona przez co najmniej 2 lata w celu wykrycia ewentualnych nawrotów.
Summary
Antrochoanal polyps are unilateral benign lesions that arise within the maxillary sinus antrum. The purpose of this study was to review the clinical characteristics and treatment of antrochoanal polyp (ACP).
A retrospective analysis was performed to investigate the case of one patient with an extremely rare bilateral polyp with a high incidence of recurrence.
ACPs account for approximately one-third of polyps occurring in children. Most of them are unilateral. The recurrent course of ACP is more prevalent in the paediatric population than in adults. ACPs require differential diagnosis with malignancies. The mainstay of treatment is surgery. The gold standard is endoscopic sinus surgery with complete removal of polyp mass under endoscopic control and widening of the maxillary sinus ostium via the middle meatus.
Postoperative follow-up of at least 2 years is very important to monitor patients for recurrence.
Introduction
Antrochoanal polyps (ACPs) are benign inflammatory lesions that occur in the paranasal sinuses. In the majority of cases, ACPs originate in the mucosa of the maxillary sinus, typically passing through the additional ostium and extending to the posterior nostrils and the nasopharynx (1, 2).
ACPs may also arise from the sphenoidal sinus, ethmoid sinuses, frontal sinus and the nasal septum, however these cases are far less common (1, 2). ACPs usually occur unilaterally. The disorder typically affects children and young adults, with antrochoanal polyps accounting for 28-50% of all polyps in children. Also, the rate of recurrence is higher in the paediatric population (1-4).
Unlike polyps accompanying allergy or cystic fibrosis, ACPs have not been observed to coexist with other disorders.
The aetiopathogenesis of antrochoanal polyps is not fully understood. ACPs originate in the mucosa of the maxillary sinus. They are believed to arise from an intramural cyst, and have an association with chronic maxillary sinusitis (1, 2, 5).
The most common sites of origin include the medial and posterior walls of the sinus in the region of the ethmoid-maxillary angle. As the polyp grows, the polypoid mass extends towards the posterior nostrils. In advanced cases, it crosses the posterior nostrils and involves the nasopharynx. The part located in the sinus (antral) presents as a thin-walled cyst filling the maxillary sinus.
The polyps were suspected to have an allergic aetiology, but histopathological examinations have found no eosinophilic infiltrates; the polyps are neutrophilic. The polyp surface is covered with pseudostratified ciliated epithelium, with a small amount of goblet cells. It consists of loose connective tissue, often with signs of oedema and scattered supraepithelial infiltrates of inflammatory cells, plasmocytes and lymphocytes.
Antrochoanal polyp presents as unilateral nasal obstruction with simultaneous mucous or mucous-purulent discharge. Other symptoms include headaches and dysfunction of the sense of smell. Cases of patients with obstructive sleep apnoea have also been reported (1, 2, 6).
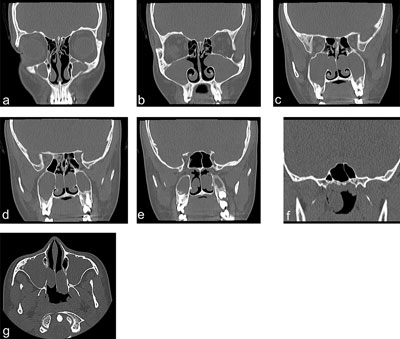
Epistaxis is an extremely rare complaint. Frontal rhinoscopy reveals the presence of a smooth grey mass representing a part of the polyp in the region of its attachment site. A large-sized polyp may be visible in the oropharynx posteriorly from the soft palate. The diagnostic work-up includes CT scan of the paranasal sinuses and nasopharynx in frontal and axial planes (fig. 1a-g).
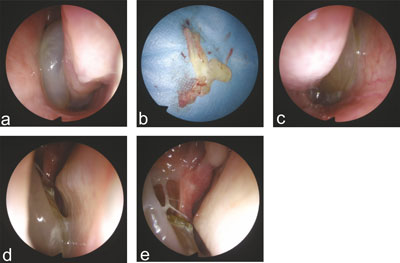
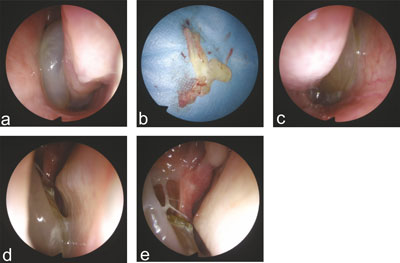
Fig. 1a-e. Intraoperative pictures (endoscope 30 degrees); a – an antrochoanal polyp of the left nasal cavity before removal; b – removed polyp from the left nasal cavity, consists of parts that previously inhabited the nasopharynx (at 12 o’clock), maxillary sinus (7 o’clock), nasal cavity (3 o’clock); c – right-side nasal cavity antrochoanal polyp before removal; d, e – condition after removal of the right maxilla antrochoanal polyp
A lesion is differentiated with congenital nasal anomalies: glioma, teratoma and dermoid cyst; nasal and nasopharyngeal tumours: nasopharyngeal angiofibroma (locally aggressive tumour occurring in adolescent males and manifesting primarily as nasal bleeding and bone erosion within the sinus walls seen on CT); and malignant tumours: rhabdomyosarcoma, esthesioneuroblastoma, lymphoma and histiocytosis. Other conditions to include in the differential diagnosis are myelomeningocele, significant adenoid hypertrophy or inferior turbinate hypertrophy, a sinus cyst and foreign body in the nasal cavity (1, 7).
ACPs are treated surgically. The gold standard is endoscopic sinus surgery. The procedure involves the removal of polyp mass from the posterior nostrils, endoscopic widening of the maxillary sinus ostium, and resection of polypoid lesions and the polyp’s attachment from within the sinus. Antrochoanal polyps are unilateral lesions. The literature contains only isolated case reports on bilateral lesions of this type (8-12).
The aim of the study is to report a very rare case of a patient with bilateral antrochoanal polyp associated with a high rate of recurrence.
Case report
The girl was admitted to the Department for the first time at the age of 13 with symptoms of bilateral nasal obstruction. CT scan of the sinuses revealed a lesion corresponding to antrochoanal polyp located in the right nasal cavity, originating from the right maxillary sinus. Other findings included adenoid hypertrophy and bilateral opacity of ethmoid cells. The patient underwent bilateral endoscopic opening of the ethmoid and maxillary sinuses followed by the removal of inflammatory mucosa together with the antrochoanal polyp attachment. The significantly enlarged adenoid was also removed.
The condition recurred – this time bilaterally – approximately one year after the surgical procedure. A CT scan of the sinuses revealed antrochoanal polyps located bilaterally, extending to the posterior nostrils on the right, and a smaller-sized polyp on the left. The polypoid lesions were removed bilaterally together with pathologically altered mucosa.
After 1.5 years, the girl, 16-years old at the time, was electively admitted to the Department, presenting symptoms of bilateral nasal obstruction and snoring. She reported no feeling of secretion moving down the back of the throat, and no disturbance of the sense of smell.
Laryngological examination revealed bilateral nasal obstruction. Frontal rhinoscopy found grey polyps located bilaterally in the middle and inferior meatus. The nasal discharge was purulent-mucous on the right, and mucous on the left. No polyp was visible in the oropharynx.
CT scan of the paranasal sinuses showed antrochoanal polyps located bilaterally in the maxillary sinuses. In addition, the examination revealed small areas of mural mucosal thickening in the right sphenoidal sinus and in isolated ethmoidal cells on the right side. The ostia of both maxillary sinuses, and the ostium of the right sphenoidal sinus were obstructed. The nasal septum was deviated to the right. The right middle nasal turbinate was pneumatized. No signs of bone destruction were observed in the structures of the nasal cavity.
The girl was found eligible for bilateral intranasal surgical removal of antrochoanal polyps using endoscopic optics (fig. 2a-e). The intranasal and antral parts of the polyp were removed bilaterally. The polyp’s attachment within the inferior wall of the maxillary sinus was removed in its entirety together with a fragment of abnormal mucosa. The girl was otherwise healthy, without a history of chronic treatment. No allergies were found. Other abnormalities included factor VII deficiency in the blood coagulation system, without clinical relevance.
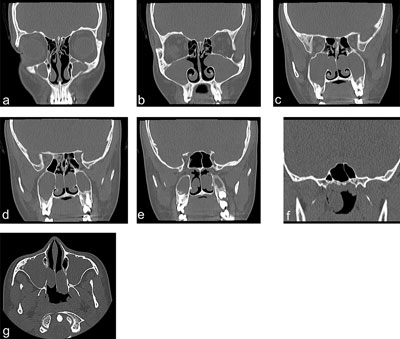
Fig. 2a-g. Images from CT scan of the paranasal sinuses without contrast before surgery in the frontal planes (a-f) and in the axial plane (g)
Every histopathological examination found a polyp covered with pseudostratified ciliated epithelium, with signs of oedema and inflammatory infiltrates of mononuclear cells as well as fragments of inflammatory mucosa sampled from the sinus mucosal layer, without other abnormalities.
Discussion
Antrochoanal polyps are benign inflammatory lesions that arise from the maxillary sinus. They account for approximately one-third of all polyps occurring in children. The lesion usually develops unilaterally, with bilateral antrochoanal polyps accounting for only 1-4% of all ACPs. There is no tendency for familial occurrence.
The cause is still not fully understood. Histopathological evidence has been obtained for the theory that ACP arises from an intramural maxillary sinus cyst, as it exhibits the same histopathological features as the cystic part of the polyp (1, 5). Intramural cysts originate from root canals during childhood. In addition, the coexisting obturation of the maxillary sinus ostium associated with the inflammatory process of allergy leads to the polyp being pushed from the sinus into the nasal cavity (1).
Histologically, ACPs are characterized by neutrophilic infiltrates, unlike polyps arising from the ethmoid sinuses which reveal predominantly eosinophilic infiltrates. Another difference is the fact that polyps originating from the ethmoid sinuses are usually bilateral (1, 3, 4).
Certain anatomical anomalies in the lateral wall and nasal septum deviation have been observed as predisposing factors to the development of antrochoanal polyps. Aydin et al. have found that the maxillary sinus volume in patients with antrochoanal polyps was bilaterally (i.e. on the polyp and non-polyp sides) higher than in the control group. Also, the ACP group was found to have a greater frequency of nasal septal deviation (usually on the opposite side of the ACP), compared to the control group (13).
The gold standard in surgical management is endoscopic sinus surgery. Key aspects include significant widening of the maxillary sinus ostium and thorough removal of the polyp’s attachment (14).
Double-endoscopic approach and access from the canine fossa are recommended in the surgical treatment of lesions projecting from the lateral and frontal walls of the maxillary sinus (2).
A wide antrostomy in the middle meatus is indicated in children with recurrent ACPs. Other coexisting pathologies, such as nasal turbinate hypertrophy, enlarged adenoid or lesions in the ethmoid sinuses, should be removed, and endoscopic septoplasty should be performed in order to improve ventilation of the sinus. Wide-angle (45 and 70°) nasal endoscopes are recommended for performing the procedure, with the additional use of a microdebrider, if required (2, 14).
A lower incidence of recurrences is associated with endoscopic sinus surgery plus mini-Caldwell surgical procedure, but the technique is contraindicated in children on account of the risk of damage to the primordia of permanent teeth. At present, the method has only historical importance (2, 15).
Conclusions
In view of the fact that the rate of ACP recurrence in children is considerably higher, postoperative follow-up should be at least 2 years, which allows the detection of 95% of recurrences (16).
Piśmiennictwo
1. Skotnicka B, Zielnik-Jurkiewicz B (pod red. D. Gryczyńskiej): Otolaryngologia dziecięca. Alfa-medica Press, Bielsko-Biała 2007: 259-261.
2. Frosini P, Picarella G, De Campora E: Antrochoanal polyp: analysis of 200 cases. Acta Otorhinolaryngol Ital 2009; 29(1): 21-26.
3. Segal N, Gluk O, Puterman M: Nasal polyps in the pediatric population. B-ENT 2012; 8(4): 265-267.
4. Caimmi D, Matti E, Pelizzo G et al.: Nasal polyposis in children. J Biol Regul Homeost Agents 2012; 26(1 suppl.): S77-83.
5. Zheng W, Hu G, Liu B et al.: Observe the origin of antrochoanal polyp and the comparison of the curative effect of antrochoanal polyp. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2016; 30(3): 209-212.
6. Veerappan I, Ramar R, Navaneethan N et al.: Antrochoanal polyp presenting as obstructive sleep apnea. Indian J Pediatr 2013; 80(11): 959-961.
7. London NR Jr, Reh DD: Differential diagnosis of chronic rhinosinusitis with nasal polyps. Adv Otorhinolaryngol 2016; 79: 1-12.
8. Oner F, Sakat MS, Gozeler MS et al.: Bilateral antrochoanal polyp. J Craniofac Surg 2015; 26(7): e661-662.
9. Basu SK, Bandyopadhyay SN, Bora H: Bilateral antrochoanal polyps. J Laryngol Otol 2001; 115: 561-562.
10. Myatt HM, Cabrera M: Bilateral antrochoanal polyps in a child: a case report. J Laryngol Otol 1996; 110: 272-274.
11. Yilmaz YF, Titiz A, Ozcan M et al.: Bilateral antrochoanal polyps in an adult: a case report. B-ENT 2007; 3: 97-99.
12. Jmeian S: Bilateral antrochoanal polyps in a child: an extremely rare case. JRMS 2006; 13(2): 57-58.
13. Aydın S, Taskin U, Orhan I et al.: The analysis of the maxillary sinus volumes and the nasal septal deviation in patients with antrochoanal polyps. Eur Arch Otorhinolaryngol 2015; 272(11): 3347-3352.
14. Eladl HM, Elmorsy SM: Endoscopic surgery in pediatric recurrent antrochoanal polyp, rule of wide kostium. Int J Pediatr Otorhinolaryngol 2011; 75(11): 1372-1375.
15. Kelles M, Toplu Y, Yildirim I et al.: Antrochoanal polyp: clinical presentation and retrospective comparison of endoscopic sinus surgery and endoscopic sinus surgery plus mini-Caldwell surgical procedures. J Craniofac Surg 2014; 25(5): 1779-1781.
16. Chaiyasate S, Roongrotwattanasiri K, Patumanond J et al.: Antrochoanal Polyps: How Long Should Follow-Up Be after Surgery? Int J Otolaryngol 2015; 2015: 297417.