© Borgis - New Medicine 4/2003, s. 97-99
Radoslaw Owczuk1, Magdalena Anna Wujtewicz1, Wioletta Sawicka1, Maria Wujtewicz1, Arkadiusz Piankowski1, Barbara Kwiecinska1, Agnieszka Markul2, Ewa Januszewska-Michalak2, Iwona Bednarska-Zytko3, Barbara Skoczylas-Stoba3, Irena Burdak4
Analysis of effective out-of-hospital resuscitations in the elderly
1 Department of Anaesthesia and Intensive Care, Medical University of Gdansk, Poland
Head: Maria Wujtewicz, MD, PhD
2 Department of Anaesthesia and Intensive Care, St. Adalbert´s Specialist Hospital, Gdansk, Poland
Head: Ewa Januszewska-Michalak, MD
3 Department of Anaesthesia and Intensive Care, N. Copernicus´ Regional Specialist Hospital,
Gdansk, Poland
Head: Barbara Skoczylas-Stoba, MD, PhD
4 Department of Anaesthesia and Intensive Care, Railway Hospital, Gdansk
Head: Irena Burdak, MD
Summary
In this paper we present the results of a questionnaire study concerning out-of-hospital resuscitations performed on the elderly (> 70 years of age). Included were 69 cases of cardiac arrest. The mean patient age was 74.6 yrs; men were more numerous than women (60.9% vs. 39.1%). The most common cause of circulation arrest was ventricular fibrillation. We analysed the patients´ state on their admission to hospital, as well as the outcomes. Most patients died a short time after admission to hospital. Of the analysed patients 7,2% survived for a period longer than 12 months.
Cardiac arrest in elderly persons is often perceived as a natural ending of their lives, particularly in those with chronic ailments. Resuscitating these patients may be considered as a treatment which is unnecessary or is fated to fail. Previous reports on cardiopulmonary resuscitation (CPR) in the geriatric population have presented different opinions from those included in the current standards and guidelines on resuscitation (1). This policy causes many physicians to initiate the reanimation of elderly patients very reluctantly. However, the DNR "do not resuscitate” rule, which is in force in some countries, concerns only selected cases of hospitalised patients, and may be applied after a scrupulous analysis of all the pros and cons of reanimation by a special committee. In no case does rule apply this to out-of-hospital reanimations, where another rule ("first rescue, then ask”) should be obeyed (2).
Current publications concerning restrictions on resuscitation include only such conditions as decapitation, body charring or decay, or the presence of rigor mortis, but do not include the patient´s age (3, 4). The aforementioned ”unwillingness” to start resuscitating elderly persons with cardiac arrest (CA) may also be caused by the rescuers´ opinions on whether or not the short– and long-term CPR outcomes in these patients will be satisfactory. Analysis of references published in English does not support these doubts univocally, and there are no publications from Polish sources. The specificity of the Polish healthcare system, due to society´s low level of education on basic (non-instrumental) life support, and to the ever-developing medical rescue system, may result in different findings from those concerning more highly-developed countries. Therefore, analysis was covered out-of-hospital cardiopulmonary resuscitations which were judged effective in persons of over 70 years of age.
MATERIAL AND METHODS
The analysis included cases of cardiac arrest and effective cardiopulmonary resuscitation in out-of-hospital environments in persons of over 70 years, in whom prehospital aid was given by reanimation teams (R teams) from the Regional Emergency Medical Service Station in Gdańsk.
First, the report books of the EMS R teams from 1997 to 2001 were analysed. Resuscitation was treated as effective if the patient was transported and admitted to a hospital emergency department. Secondly, study questionnaires were sent to departments of intensive care in 4 hospitals.
Seventy-one replies to questionnaires were obtained. Two cases of isolated respiratory arrest were excluded; and so 69 cases of cardiac arrest in out-of-hospital environments were for analysed.
Two scales were included in the questionnaire: the Glasgow Coma Scale (GCS), and the five-gradelarge Cerebral Performance Category (CPC) (according to 5).
RESULTS
The analysis included 69 questionnaires, 27 of which concerned women (39.1%), and 42 men (60.9%). The mean age in the studied population was 74.61 years (range of 70-91 yrs; std 4.84). Age of women ranged from 70 to 91 yrs, and mean age was 74.96 yrs (SD 5.71; median 74 yrs). Men´s age ranged from 70 to 89 yrs with mean value of 74.38 yrs (SD 4.24; median 74 yrs). No statistically significant difference was found between the mean ages of the men and women (p = 0.629).
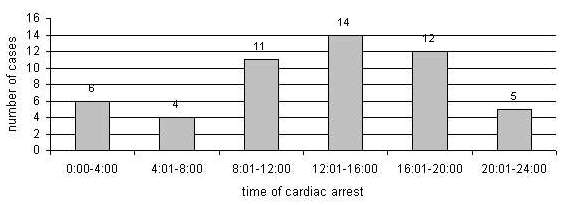
In 52 cases the time of cardiac arrest was established, as shown in fig. 1.
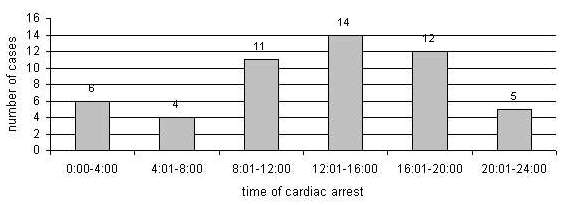
Fig. 1. Incidents of cardiac arrest by time of day.
In 36 patients cardiac arrest occurred at home (52.1%), in 9 persons it happened in the street, one patient had CA in church and another one in a bank. No cases of cardiac arrest in a workplace were noted, and in 22 cases the environment where CA and resuscitation took place could not be stated.
With the aid of each patient´s medical documentation, the following ailments from before the CA incident were found: ischaemic heart disease – 40 cases; history of myocardial infarction – 21; arterial hypertension – 21; chronic circulatory insufficiency – 20; brain stroke/hemiparesis – 9; bronchial asthma/COPD – 7; diabetes mellitus – 14; disturbances of cerebral circulation – 7. Four patients suffered from neoplastic disease; in two of them the disease was disseminated, and two were cured of cancer. One patient had been previously resuscitated 13 months before (discharged from hospital with a CPC score of 1).
The most frequent pathogenic cause of cardiac was ventricular fibrillation (VF), observed in 33 cases altogether. Asystole occurred in 9 cases, and bradyasystole in 4 cases. No cases of pulseless electrical activity (PEA) or pulseless ventricular tachycardia (PVT) were observed. In 29 cases the medical documentation contained no remarks on the mechanisms of patients´ cardiac arrest! Before transportation to hospital the majority of the patients (95.6%) were intubated. Three persons had their airways unprotected, and in two of them respiration was inefficient.
Adrenalin was the most frequently administered drug (40 documented cases), whilst atropine was administered in 21 cases, lignocaine in 17 cases, and bretylium in 2 cases of VF; no case of amiodarone administration was found. Bicarbonate solution was administered in 19 patients, and 24 patients were treated with corticosteroids (dexamethasone or hydrocortisone). Other applied medication included frusemide (7 patients), aminophylline (one patient), verapamil (one patient), digoxin (one patient), and drip infusion of dopamine (8 patients) or dobutamine (2 patients). Electrical defibrillation was performed on 29 patients; in two of them this was the only method of treatment which permitted the restoration of efficient circulation.
On admission to emergency departments 18 patients (26.1%) showed no vital signs; in each case CPR was initiated in the emergency department. CPR was effective in 5 cases, and in 13 cases death in the emergency department was recorded.
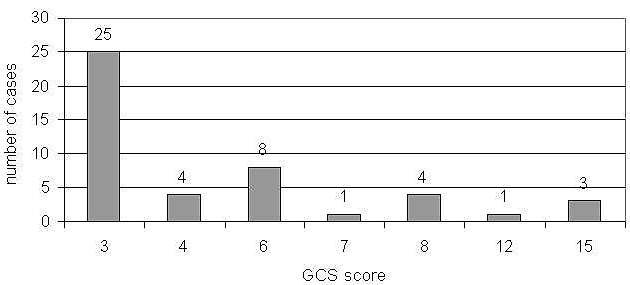
Vital signs on admission were observed in 51 patients, breathing was evaluated as efficient in 7 patients (13.7%), and circulation was efficient in 26 patients (50.98%). The consciousness of 3 persons was described as "complete”. In 46 persons consciousness was assessed by means of the GCS; scores are presented in fig. 2.
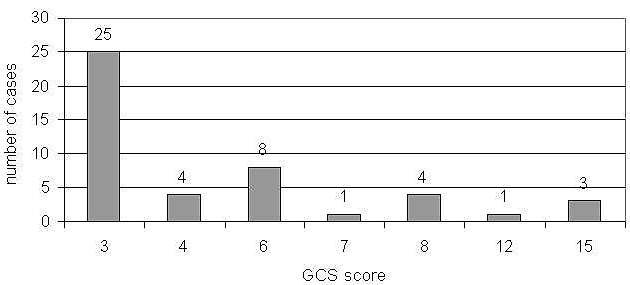
Fig. 2. Patient assessment by the Glasgow Coma Scale on admission to emergency departments.
ECG charts showed ventricular and supraventricular extrasystole (12 and 2 patients, respectively), atrial fibrillation (9 patients), LBBB in 6 patients, RBBB in one patient. The ST interval was lowered in 8 cases, and Pardee´s wave was present in 6 cases.
The majority of patients (73.2%) were admitted to intensive care departments, but others were admitted to cardiology (17.9%) or internal disease departments (8.9%).
On admission, 43 of 56 patients died in their admitting department after varying time intervals. Within 24 hours those deceased totalled 14 patients (25%), from 24 hrs to 7 days – 15 patients (26.8%), and from 8 to 31 days from admission another 14 patients died (25%). Thirteen patients (23.2%) were discharged from the ICU and transported to other departments. In this group, 6 patients died during the course of further hospitalisation and 7 patients (3 women and 4 men) were discharged from hospital. In 6 of these patients cardiac arrest occurred with VF, and in one bradyasystole was diagnosed. On admission to hospital all these patients had efficient circulation, and in 4 of them breathing was assessed as insufficient. A GCS evaluation of these patients on admission was performed in 5 cases (one patient – 12 points, one patient – 8, one patient – 6, 2 patients – 4). When transported from intensive care to other departments, the CPC was assessed; in 4 patients the consciousness level was assigned grade 1, in 2 patients grade 2, and in one patient grade 3. It was noted that 5 of these patients (constituting 7.24% of the studied population) survived more than 12 months. No data was available on the outcome in 2 patients after their discharge from hospital.
DISCUSSION
The outcome of CPR depends on many factors, including type of environment where the incident took place, presence of witnesses, the performance of initial rescue manoeuvres, the time before arrival of professional rescuers, or the mechanism of CA (5, 6, 7). According to data in the literature, the patient´s age does not determine the early results of resuscitation (8), although there are reports on worse late prognosis of CA in the elderly. Weston et al. demonstrated lower survival rates in a group of patients aged> 69 years in whom cardiac arrest occurred in out-of-hospital environments. They reported that potential causes of this may include a lack of witnesses of cardiac arrest, and a higher incidence of cardiac arrest mechanisms associated with a poor prognosis (9). Additionally, the results of treatment of post-resuscitation diseases in aged persons are much worse than those in younger patients (8, 9).
The group contained a majority of men (60.9%), which is consistent with the reports in literature. In most publications, cases of cardiac arrest in out-of-hospital settings mainly affected the male population, irrespective of the age group (59-73.8%) (4, 9, 10, 11). The geriatric population also showed an analogous male preponderance (10).
Cardiac arrest occurred most often in patients´ homes, and in the majority of cases during the daytime, which warrants the suggestion of presence of a witness to the incident. However, the analysed medical documentation lacks some data on CA witnesses and on initial rescue procedures possibly performed by them before the arrival of the reanimation emergency medical team. This fact prevented us from including these extremely important prognostic factors (5, 12) in the analysis. Finn et al. carried out an analysis of cardiac arrest incidence in the daytime, and noted that persons of over 65 years experienced CA mostly during the day, which is consistent with our findings (10).
As in other reports, VF was the most common cause of CA in our study. It should be noted that although VF was observed in 33 patients, electrical defibrillation was performed on only 29 of them, although defibrillation is the most effective method of VF treatment (13, 14), and defibrillators are available in every emergency service team´s vehicle. The lack of cases of PEA and PVT may be surprising, as the mentioned mechanisms of CA are relatively common in elderly patients (6, 9). No one primary non-cardiac cause of CA was distinguished, but it should be noted that non-cardiac causes of CA are less frequently observed in the elderly compared to younger patients (15).
In most patients the applied pharmacotherapy was consistent with current standards (16). However, the frequent use of glycocorticosteroids may be surprising, especially the administration of hydrocortisone which is difficult to explain. Incidental major errors were also observed in prehospital management. Noteworthy were two patients with insufficient breathing who were transported to hospitals without intubation, as well as a case of digoxin administration in a patient with VF.
The outcome of CPR in the studied population is similar to that reported by other authors. As many as 23% of patients admitted to hospitals after sufficient breathing and circulation was restored were transported for further treatment to other departments. Seven patients were discharged from hospital, the majority of whom were males and patients with CA caused by VF. Therefore, it may be assumed that the percentage of survivals in excess of 12 months reached 7.24%, the result being close to the those reported by other authors (4, 17). In our situation the results are satisfactory, but an improvement of life rescue services and basic education on life support for large groups would allow us to achieve better results.
Piśmiennictwo
1. Hołub S.: Reaniamcja. W: Kamiński B. (red.) Anestezja i reanimacja, PZWL Warszawa 1975. 2. Skinner D.V. et al.: Cardiopulmonary resuscitation. Oxford University Press, Oxford 1993. 3. Colquhoun M.C. et al.: ABC of resuscitation. BMJ Books, London 1999. 4. Iwami T. et al.: Age and sex analyses of out-of-hospital cardiac arrest in Osaka, Japan. Resuscitation 2003; 57:145-152. 5. Cummins R.O. et al.: Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation 1991, 84, 960-975. 6. Engdahl J. et al.: Factors affecting short- and long-term prognosis among 1069 patients with out-of-hospital cardiac arrest and pulsless electrical activity. Resuscitation 2001; 51:17-25. 7. Engdahl J. et al.: The epidemiology of out-of-hospital "sudden" cardiac arrest. Resuscitation 2002; 52:235-245. 8. Ritter G. et al.: The effect of bystander CPR on the survival of out-of-hospital cardiac arrest victims. Am. Heart J. 1985; 110:932-937. 9. Weston C.F.M. et al.: Predicting survival from out-of-hospital cardiac arrest: a multivariate analysis. Resuscitation 1997; 34:27-34. 10. Finn J.C. et al.: Outcomes of out-of-hospital cardiac arrest patients in Perth, Western Australia, 1996-1999. Resuscitation 2001; 51:247-255. 11. Kim C. et al.: Out-of-hospital cardiac arrest in men and women. Circulation 2001; 104: 2699-2703. 12. Śliwkiewicz K. i wsp.: Wykorzystywanie wzorca z Utstein do zbierania danych dotyczących pozaszpitalnych zatrzymań krążenia. Med. Intens. Rat. 2002; 5:209-215. 13. Kosiński S.: Czynniki wpływające na skuteczność defibrylacji elektrycznej. Med. Intens. Rat. 2002; 5: 201-207. 14. Mysiak A.: Nowe spojrzenie na genezę oraz skuteczność profilaktyki i terapii migotania komór serca. Med. Int. Ratunk. 2002; 5:193-199. 15. Engdahl J. et al.: Characteristics and outcome among patients suffering from out of hospital cardiac arrest of non-cardiac aetiology. Resuscitation 2003; 57:33-41. 16. de Latorre F. et al.: European Resuscitation Council: European Resuscitation Council Guidelines 2000 for Adult Advanced Life Support. A statement from the Advanced Life Support Working Group and approved by the Executive Committee of the European Resuscitation Council. Resuscitation 2001; 48:211-221. 17. Bonnin M.J. et al.: Survival in the elderly after out-of-hospital cardiac arrest. Crit. Care. Med. 1993; 21:1645-1651.