© Borgis - New Medicine 4/2003, s. 100-103
Radoslaw Owczuk, Magdalena A. Wujtewicz, Wioletta Sawicka, Maria Wujtewicz, Maria Szlyk-Augustyn, Anna Wadrzyk
Analysis of causes of Emergency Medical Service resuscitation teams being called to elderly patients
Department of Anaesthesia and Intensive Care,Medical University of Gdansk, Poland
Head: Maria Wujtewicz, MD, PhD
Summary
In this study we have analysed the causes of Emergency Medical Service resuscitation teams being called to persons aged over 70 years during the year of 2001 in the city of Gdańsk. A total of 2016 call constituted 18.22% of all prehospital emergency medical interventions during the period. More female (60.81%) than male patients required aid. Medical and neurological problems predominated among the causes of EMS calls. Chest pain was the call reason in 20.88% of patients, and dyspnoea and simple fainting in 16.17% and 15.53% of cases respectively. Unconsciousness was recorded in 14.88%, brain stroke in 4.56% of patients. The number of EMS visits to persons with injuries was much lower, and constituted only 4.38% of all calls. During the period 22 effective CPRs were provided and 135 deceases occurred before EMS arrival. In 88.6% of cases the cause of calling was consistent with the actual situation found at the site.
Constant medical progress results in the acceleration of population ageing. In the USA during a five-year period an increase in the number of admissions of elderly patients to emergency departments was observed (1). It is believed that in an emergency medical intervention in a person over 65 years old, probability of his/her admission to hospital is five times higher than in a younger persons; similarly, the chance of admission of an elderly patient to the intensive care department is five times greater (2). Similar problems are observed in Poland, but there is a lack of publications about the use of Emergency Medical Service (EMS) by elderly patients in our country.
MATERIAL AND METHODS
All Emergency Medical Service resuscitation team calls to persons over 70 years of age during 2001 in Gdańsk were subject to this analysis. Analysed data included: patient age, cause of the call, and consistency of the causes for calling and the actual findings at the site. In 2001, the emergency resuscitation service was supplied in Gdańsk and area by 5 teams. In the year, there were approx. 400,000 persons registered in the area covered by the Gdańsk EMS Station.
The fact of a patient´s admission was considered the measure of efficacy of cardiopulmonary resuscitation. Consistency of the cause for calling and the actual event was noted positive when the reason for calling was part of the clinical diagnosis, and patient´s state or symptoms might have changed before the arrival of the EMS team.
RESULTS
In 2001 the 5 teams at the EMS Station in Gdańsk supplied medical services in 31 930 cases, of which 11 063 interventions were effected by resuscitation teams. In 2016 cases services concerned persons over 70 years, which made up 18.22% of the resuscitation teams (R) interventions. Women constituted 60.81% of patients and men 39.19%.
The age of patients ranged from 70 to 100 years (mean age 77.3 years; SD 5.72). The percentages of respective age groups are presented in table 1.
Table 1. Characteristics of patients´ age in the analysed group.
| Age group | 70-74 yrs | 75-79 yrs | 80-84 yrs | 85-89 yrs | 90-94 yrs | 95-99 yrs | 100 yrs |
| Number of patients (%) | 748 (37.1%) | 600 (29.8%) | 404 (20.0%) | 188 (9.3%) | 65 (3.2%) | 10 (0.5%) | 1 (0.05%) |
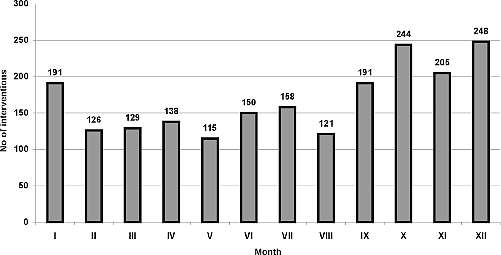
Distribution of the R teams´ callings in subsequent months is shown in figure 1.
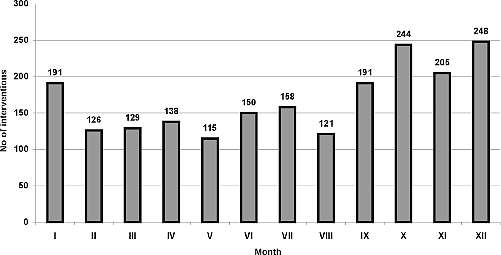
Fig 1. Number of calls for EMS by month.
Causes of calls are listed by quantity in table 2.
Table 2. Cause of calling for EMS in view of mean patient age, standard deviation of age, and sex.
| Cause of calling | Number of patients | % of patients | Mean age
(standard deviation) | Women/Men |
| Chest pain
(incl. cardiac pain, retrosternal pain) | 421 | 20.88 | 76.82 (5.26) | 268 / 153 |
| Dyspnoea | 326 | 16.17 | 77.60 (5.66) | 178 / 148 |
| Fainting | 313 | 15.53 | 77.29 (6.05) | 213 / 100 |
| Unconsciousness | 300 | 14.88 | 77.49 (6.01) | 177 / 123 |
| Brain stroke
(incl. suspicion
of stroke, paresis) | 92 | 4.56 | 78.52 (5.85) | 58 / 34 |
| Asthma | 91 | 4.51 | 75.25 (4.37) | 55 / 36 |
| Digestive tract haemorrhage | 44 | 2.18 | 77.59 (5.86) | 21 / 23 |
| Loss of contact
with a person | 43 | 2.13 | 78.37 (6.56) | 29 / 14 |
| Arrhythmia | 42 | 2.08 | 76.40 (4.33) | 28 / 14 |
| Hit by a vehicle | 27 | 1.34 | 76.50 (4.67) | 13 / 14 |
| Head injury | 26 | 1.29 | 78.40 (6.57) | 10 / 16 |
| Coma | 23 | 1.14 | 79.70 (7.21) | 13 / 10 |
| Hypertension | 22 | 1.09 | 77.23 (5.73) | 18 / 4 |
| Seizures
(incl. epileptic fit) | 21 | 1.04 | 77.00 (6.21) | 10 / 11 |
| Fall from height | 17 | 0.84 | 77.65 (6.61) | 12 / 5 |
| Decease? | 16 | 0.79 | 79.63 (5.2) | 7 / 9 |
| Lying in the street | 12 | 0.59 | 76.58 (6.35) | 5 / 7 |
| Pulmonary oedema | 11 | 0.55 | 80.09 (5.92) | 6 / 5 |
| Traffic accident | 11 | 0.55 | 77.45 (4.37) | 6 / 5 |
| Rattling breath | 8 | 0.4 | 80.25 (7.54) | 2 / 6 |
| Beaten person | 7 | 0.35 | 72.1 (3.52) | 4 / 3 |
| Cyanosed person | 6 | 0.3 | 81.33 (3.89) | 3 / 3 |
| Dying | 6 | 0.3 | 79.33 (3.88) | 4 / 2 |
| Agony | 4 | 0.2 | 79.75 (8.42) | 3 / 1 |
| Does not breathe | 3 | 0.15 | 76.00 (4.58) | 2 / 1 |
| Others | 124 | 6.16 | 77.86 (5.66) | 81 / 43 |
The specificity of the R team tasks in the emergency medical system is indicated by the gravity of the cause for a call. The teams are sent to persons in whom the Despatch Manager at the EMS station suspects a direct life– and health-threatening incident. Among these are priority situations, for which the knowledge, skills and medical supplies of the R team may determine the patient´s survival. To our belief, the causes presented below are such priorities. Together with the causes for call and their numbers, diagnoses made at the event sites are noted as well as numbers of patients with given diagnoses (in brackets):
– acute chest pain (421): exacerbation of coronary artery syndrome (CAS) (225), hypertension (34); arrhythmias (27), circulatory insufficiency (26), intercostal neuralgia (14), fainting (12), abdominal pain (11), decease before arrival (10), pulmonary oedema (4), others (58);
– fainting (313): syncope (105), fainting (53), CAS (25), disturbances of cerebral circulation (DCC) (20), hypertension (18), decease before arrival (11), brain stroke (10), cardiac arrhythmias (6), others (65);
– dyspnoea (326): CAS (58), circulatory insufficiency (46), bronchial asthmatic fit (42), pulmonary oedema (33), pneumonia (18), arrhythmias (17), hypertension (14), decease (12), chronic obstructive pulmonary disease (COPD) (11), syncope (8), respiratory insufficiency (5), cardiac arrest (1), others (61).
– unconsciousness (300): fainting (67), decease (59), brain stroke (34), cardiac arrest (18), DCC (15), fainting (14), seizures (13), unconsciousness due to unspecified cause (9), CAS (9), hypoglycaemia (8), head injury (8), others (46);
– brain stroke (92): brain stroke (45), DCC (14), syncope (12), hypertension (6), fainting (3), others (12);
– loss of contact with the person (43): syncope (7), brain stroke (7), DCC (6), CAS (4), fainting (3), others (16);
– hit by a vehicle (27): head injury (14), multiple body injuries (8), limb injuries (4), suspicion of spine injury (1);
– coma (23): hypoglycaemia (15), ketotic coma (5), cerebral coma (1), head injury (1), COPD (1);
– convulsions (21): epileptic fit (5), DCC (4), fainting (3), cardiac arrest (1), others (8);
– fall from height (17): head injury (7), limb injuries (6), decease (2), other injuries (2);
– pulmonary oedema (11): pulmonary oedema (5), circulatory insufficiency (3), atrial fibrillation (1), pneumonia (1), decease before arrival (1);
– "rattling breath” (8): decease before arrival (2), circulatory insufficiency (2), coma (1), chronic renal insufficiency (1), brain stroke (1), arm injury (1);
– cyanosed person (6): COPD (2), brain stroke (2), fainting (1), decease before arrival (1);
– "person dying” (6): decease before arrival (3), fainting (1), chest pain (1), DCC (1)
– does not breathe (3): cardiac arrest (1), pneumonia (1), circulatory insufficiency (1)
During the analysed period 22 effective cardiopulmonary resuscitations were performed. Causes for calls in this group were: unconsciousness (18 patients), asthmatic fit (1), "doesn´t breathe” (1), seizures (1), fainting (1).
Decease before the arrival of the EMS team occurred in 135 cases.
Consistency of causes for calling EMS and actual diagnoses was positive in 1787 (88.6%) cases. The majority of patients (1402 persons) were transported to hospital. In 471 cases (23.4%) a medical service was supplied at the event site; 8 patients refused transportation to hospital.
DESCRIPTION OF RESULTS
In the study we analysed the causes for 2016 calls for EMS to persons over 70 years of age, supplied by resuscitation teams in one city during one year. This age group comprises approximately 10% of the inhabitants of the city population. The incidence of R team calls for this age group was 18.22%, which indicates a greater demand for EMS in this population, when compared to younger persons. Women constituted the majority of the cases, which is consistent with the sex distribution for the given age group. Comparison of the results with those of other authors is difficult, due to the different ranges of patient age groups in other publications. Witczak et al. found that the incidence of EMS R team calls to persons over 61 years was 37.2% (3). In a report on EMS calls in the city of Poznań, the index reached 36.8% (4). Analyses of emergency department activities in the USA and Australia revealed a 33-54.6% incidence of transportation of patients over 65 years to these services by EMS vehicles (2, 5, 6, 7).
The two largest groups of causes for EMS calls were internal diseases and neurological problems (89.47% altogether). Callings for injuries were much less frequent (4.37%). A similar preponderance of internal diseases over injuries has been observed by other authors (4, 8, 9). According to Ettinger, the incidence of internal and neurological diseases in elderly patients hospitalised in emergency departments reaches 75%, whereas in younger patients these caused 53.2% of admissions (6).
Chest pain is the major cause of calls, most often resulting from diseases of the circulatory system. Diseases of other organs of the thorax (e.g. pneumonia) or of organs outside the thorax (e.g. abdominal pain) were also diagnosed. Women constituted the majority of the chest pain group (63.6% of women vs. 36.4% of men), despite the fact that the most common disease in this group, which is CAS, is observed more frequently in men over 70 years (15%) compared to women of the same age (9%) (10).
Fainting was the second most common cause of calls. At the event site diverse diagnoses were given – from transient worsening of the patient´s well-being or syncope, to decease occurring before the arrival of the team. The lack of specificity in causes, and the extremely divergent actual diagnoses point to a need for more careful history-taking and questioning by the EMS dispatchers who decide to send teams.
Dyspnoea, being the third most numerous cause of calls in the analysed group, is a relatively unspecific symptom, which occurs in many diseases, including those observed in the elderly population (11). The main diagnoses were diseases of the circulatory system, including serious conditions as pulmonary oedema. Calls to unconscious persons included a large number of cases of cardiac arrest. Unfortunately, the available references do not contain analyses of causes of unconsciousness in the elderly population, which makes it impossible to compare the results herein with those of other authors.
Injuries, resulting in a small percentage of calls and actual diagnoses were in most cases caused by vehicle impact, falling on, falling from a heights and other traffic accidents. The references concerning injuries in the elderly mention falling down (tumbling) as the main cause of injuries (54%) (12). In our study virtually no such cases were noted, however they may be hidden in calls to persons who have apparently fainted, with head injuries, or "lying in the street”. The analysed actual diagnoses included only 6 cases of a common senile pathology, which is femoral neck fracture. This is probably due to the supply of an emergency medical service to these patients by the general medical teams.
Patients who had medical aid were transported to various hospitals (69,5%), while in 6.7% of cases decease was diagnosed. Altogether, this constitutes 76.2% of the patients to whom the EMS was called. It may be assumed that the remainder, approx. 25% of patients, did not require intervention by the reanimation team. This may be due to the fact that the personnel receiving calls in EMS stations finds it difficult to verify or query symptoms mentioned by the caller. Our own experience shows that callers often aggravate their current symptoms, or add other ones, hoping to receive the EMS aid sooner. However, this does not eliminate the need for the EMS dispatcher to send a reanimation team to any case when a life-threatening condition is suspected.
Piśmiennictwo
1. Strange G.R., Chen E.H.: Use of emergency departments by elder patients: a five-year follow-up study. Acad. Emerg. Med. 1998; 5(12): 1157-1162. 2. Sanders A.B.: Care of the elderly in emergency departments: conclusion and recommendations. Ann. Emerg. Med. 1992; 21(7):830-834. 3. Witczak W. i wsp.: Stany zagrożenia życia w materiale Oddziału Pomocy Doraźnej ZOZ w Puławach. Zdr. Publ. 1994; 105(8): 276-279. 4. Ulatowska-Szostak E., Marcinkowski J.T.: Analiza wyjazdów pogotowia ratunkowego w mieście Poznaniu. Probl. Med. Społ. 1997; 32:385-390. 5. Clark M.J., Fitzgerald G.: Older people´s use of ambulance services: a population-based analysis. J. Accid. Emerg. Med. 1999; 16(2):108-111. 6. Ettinger W.H. et al.: Patterns of use of the emergency department by elderly patients. J. Gerontol. 1987; 42(6):638-642. 7. Singal B.M. et al.: Geriatric patient emergency visits. Part I: Comparison of visits by geriatric and younger patients. Ann. Emerg. Med. 1992; 21(7): 802-807. 8. Dickinson E.T. et al.: Geriatric use of emergency medical service. Ann. Emerg. Med. 1996; 27(2):199-203. 9. McConnel C.E., Wilson R.W.: The demand for prehospital emergency services in an ageing society. Soc. Scie. Med. 1998; 46(8):1027-1031. 10. Malik N.: Diagnosis and Management of Acute Coronary Syndromes, Geriatrics and Ageing 2001; 4(8):11-14. 11. Malkin L.: Diagnostic approaches to new onset respiratory symptoms in the elderly: dyspnoea and cough. Geriatrics and Aging 1999; 2(5):18-26. 12. Grisso J.A. et al.: Injuries in an elderly inner-city population. J. Am. Geriatr. Soc. 1990; 38(12):1326-1331.